Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Doi:10.1016/j.jcrs.2005.08.055
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
Enhancement outcomes after photorefractive
keratectomy and laser in situ keratomileusis
using topographically guided excimer laser
Leopoldo Spadea, MD, Angela Di Gregorio, MD
PURPOSE: To evaluate the efficacy and safety of topographically guided excimer laser photoablationto retreat unsuccessful myopic and hyperopic photorefractive keratectomy (PRK) and laser in situ ker-atomileusis (LASIK).
SETTING: Eye Clinic, San Salvatore Hospital, University of L'Aquila, L'Aquila, Italy.
METHODS: At least 3 months after primary PRK (Group A) or primary LASIK (Group B), 48 eyes of 42patients were submitted to PRK or LASIK enhancements. The eyes were treated with an excimer laserlinked to a computerized videokeratography unit with a topographically supported customized abla-tion workstation.
RESULTS: The mean follow-up was 27.8 months G 8.2 (SD). In Group A, the uncorrected visual acuity(UCVA) changed from 0.5 G 0.7 logarithm of the minimum angle of resolution (logMAR) (range 20/600to 20/200) to 0.1 G 0.7 logMAR (range 20/60 to 20/20); the mean best spectacle-corrected visual acuity(BSCVA) changed from 0.1 G 0.7 logMAR (range 20/50 to 20/20) to 0 G 0.7 logMAR (range 20/50 to20/20) after the enhancement. In Group B, the UCVA changed from 0.7 G 0.8 logMAR (range 20/600 to20/40) to 0.1 G 0.7 logMAR (range 20/40 to 20/20); the mean BSCVA improved from 0.2 G 0.8 logMAR(range 20/30 to 20/20) to 0 G 1.3 logMAR (range 20/25 to 20/20) after surgery.
CONCLUSIONS: The enhancements using topographically guided excimer laser photoablation witha topographically supported customized ablation method resulted in satisfactory and stable visualoutcome with good safety and efficacy after unsuccessful PRK and LASIK.
J Cataract Refract Surg 2005; 31:2306–2312 Q 2005 ASCRS and ESCRS
Excimer laser refractive surgery has proven to be an effec-
primary unsuccessful PRK or LASIK, topography-based ab-
tive and safe technique to correct low to medium refractive
lation, which has been adapted to the corneal irregularity,
errors. In eyes with a regular surface and curvature of the
should provide better results. The recently introduced ex-
cornea, conventional excimer laser photorefractive kera-
cimer laser customized ablation has proven to be a powerful
tectomy (PRK) or laser in situ keratomileusis (LASIK)
technique to treat irregular corneas.The objective of this
can provide good results.Nevertheless, if the cornea has
study was to determine whether topographically guided ex-
an irregular surface shape, such as reoperation after
cimer laser photoablation can be effective and safe for thetreatment of the residual myopia or hyperopia after primarymyopic or hyperopic PRK or LASIK.
Accepted for publication May 27, 2005.
From the Eye Clinic, San Salvatore Hospital, University of L'Aquila,
PATIENTS AND METHODS
L'Aquila, Italy.
Patients were enrolled between March 2000 and July 2002,
None of the authors has a financial or proprietary interest in any
after the local ethics committee approved the study protocol.
methods or materials mentioned.
Forty-eight eyes of 42 patients who requested retreatment for sig-
Reprint requests to Leopoldo Spadea, MD, Via Benozzo Gozzoli
nificant undercorrection or overcorrection after PRK or LASIK
34, 00142 Rome, Italy. E-mail:
were enrolled in this prospective noncomparative case series.
Q 2005 ASCRS and ESCRS
0886-3350/05/$-see front matter
Published by Elsevier Inc.
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
Table 1. Mean manifest refraction spherical equivalent in all patients after first refractive procedure (42 patients).
Mean MRSE (D) (Range)
Undercorrected and
Overcorrected Eyes
(ÿ4.75 to C2.50)
(ÿ1.50 to C0.50)
LASIK Z laser in situ keratomileusis; MRSE Z manifest refraction spherical equivalent; O Z overcorrected eyes after the original treatment; PRK Z photo-refractive keratectomy; U Z undercorrected eyes after the original treatment
The mean preoperative refraction is shown in According
power; when the SRI is elevated, the corneal surface in front of
to the primary refractive procedure, patients were divided into
the pupil is irregular, leading to a reduction in BSCVA.
2 groups: Group A after PRK and Group B after LASIK. Group A
In Group A (re-PRK) the mean time between the first treat-
consisted of 37 eyes of 32 patients (13 women and 19 men;
ment and the retreatment was 20.63 G 25.16 months (range 6
mean age 38.3 years G 8 [SD] [range 23 to 55 years]) ().
to 108 months). In Group B (re-LASIK), the mean time between
Group B consisted of 11 eyes of 10 patients (4 women and
the first treatment and the retreatment was 3.82 G 1.40 months
6 men; mean age 39.9 years G 9.1 [SD] [range 23 to 54 years])
(range 3 to 6 months). Informed consent was obtained from
). Myopic or hyperopic patients (after primary excimer
each patient.
laser procedure) were newly stratified in the 2 groups.
All eyes enrolled in this study had been treated originally
with the MEL-70 excimer laser (Carl Zeiss Meditec) using a stan-dard PRK or LASIK procedure (Hansatome microkeratome
Surgery was performed by 1 surgeon (L.S.) using the MEL-70
[Baush & Lomb], 160 mm plate, 9.5 mm suction ring). The pri-
excimer laser linked to computerized videokeratographer TMS-3
mary indications for retreatment were significant regression or
with topographically supported customized ablation workstation
overcorrection relative to the original refractive defect, which
(TOSCA). TOSCA is a system that allows performance of topogra-
led to the patients' request for treatment of their residual refrac-
phy-supported refractive surgery in which the individual patient
tion. The patients were submitted to a complete ophthalmologic
corneal topography is measured and converted to a custom abla-
examination including manifest and cycloplegic refraction, uncor-
tion profile. The TMS-3 allows viewing of an axial map and an el-
rected visual acuity (UCVA) and best spectacle-corrected visual
evation map, which is useful for the planned calculation of the
acuity (BSCVA), tonometry, computerized videokeratography
ablation pattern. The colors on the map indicate deviations
using TMS-3 topography (Tomey), 50 MHz ultrasound pachy-
from a perfect spherical surface. Relatively high areas are not ele-
metry to measure the epithelium and overall corneal thickness
vations; they are areas just above the sphere. The TOSCA software
(Sonogage), noncontact endothelial specular microscopy (Seed
selects the keratometric value of the perfect sphere as a reference
SP500), infrared pupillometry (Colvard, Oasis) and fundus
surface (best-fit sphere) and converts this information into a con-
trol program for the excimer laser, which exactly ablates the col-
Two topographic indices were analyzed to verify the changes
ored elevation (yellowish brown) to the nominal color (gr
in corneal surface regularity: surface asymmetry index (SAI) and
TOSCA includes the tissue-saving algorithm (TSA) module that
surface regularity index (SRI). The SAI measures the difference
achieves a combined correction by piling up spherical and cylin-
in corneal powers at every ring (180 degrees apart) over the entire
drical correction with sparing of the ablated corneal tissue. The
corneal surface. The SRI is correlated with the potential visual
TSA maintains the same ablation profile and allows preservation
acuity and measures the local fluctuations in the central corneal
of and increases in the ablation depth. This algorithm considers
Table 2. Preoperative data before PRK retreatments (32 patients).
Corneal Thickness (mm)
(20/100 to 20/25)
BSCVA Z best spectacle-corrected visual acuity; MRSE Z manifest refraction spherical equivalent; Time Z months elapsed between the first treatment andthe retreatment; UCVA Z uncorrected visual acuity
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
Table 3. Preoperative data before LASIK retreatment (10 patients).
(20/400 to 20/20)
(ÿ1.50 to ÿ4.75)
(20/100 to 20/50)
BSCVA Z best spectacle-corrected visual acuity; MRSE Z manifest refraction spherical equivalent; Time Z months elapsed between the first treatment andthe retreatment; UCVA Z uncorrected visual acuity
the geometric rule that the larger the area and/or the smaller the
No patients showed a rise in intraocular pressure during the
ray of curvature, the deeper the ablation must be to obtain the de-
follow-up. Each patient was examined starting from the first hour
sired change and vice versa.
after the treatment and after 1, 7, and 15 days, and 1, 6, 12, 24, and
The laser settings were as follows: 193 nm wavelength, 35 Hz
frequency, 180 mJ/cm2 fluence, and 0.25 mm ablation rate. The la-ser uses a 1.8 mm diameter flying spot with a gaussian profile. Anactive eye-tracking system oriented to a metal ring acted as an
Statistical Analysis
artificial limbus and maintained the centration. A cone for con-trolled atmosphere was added to the laser output to extract smoke
Data were collected postoperatively and entered into an Ex-
or particles in the air without creating a draft and to remove all ob-
cel spreadsheet for subsequent analysis (Microsoft, Inc.). Data are
stacles in the path of the laser beam. The refractive goal in all eyes
reported as mean G standard deviation (SD). Statistical analysis
was emmetropia.
was performed using the Student t test.
The excimer retreatments were performed using topical anes-
thesia with oxybuprocaine 0.4% drops; a sterile eyelid speculum
All patients were treated once, and no intraoperative or
was placed in the operative eye. The patient was directed to
postoperative complications were noted. Forty-eight eyes
look into coaxial light (yellow diode), and the ablation was cen-
of 42 patients with a mean follow-up of 27.8 G 8.2 months
tered on the entrance of the center of the pupil. To remove the cor-
(range 12 to 36) were evaluated in the present study.
neal epithelium, a calculated deeper ablation using TSA softwarewas setted (mean 57.2 G 7.4 mm [range 53 to 69 mm]) to theplanned TOSCA ablation. After the photoablation, a soft contact
Visual Acuity and Refractive Outcomes
lens was applied and a topical antibiotic agent (ofloxacin 0.3%)and artificial teardrops were applied until reepithelialization was
In both groups the UCVA and BSCVA improved
completed (from 4 to 6 days). Topical corticosteroids (butyrate
(). The refractive stabilities are shown in
clobetasone 0.1%) drops were administered for at least 1 monthand then tapered and titrated depending on the corneal haze
and refractive outcome.
The mean manifest refraction spherical equivalent
After topical anesthesia (lidocaine 4% drops), the cornea was
marked with gentian violet to ensure correct replacement of the
(MRSE) for myopic retreatment was ÿ2.54 G 2.60 diopters
corneal flap at the end of the procedure (Bansal LASIK Marker,
(D) (range ÿ0.50 to ÿ6 D); at the last postoperative exam-
ASICO). Then, the hinged flap was carefully lifted with a Paton
ination, it was ÿ0.05 G 0.66 D (range ÿ0.50 to C0.75 D)
spatula and placed against the superior sclera. Before the ablation,
(P!.01). Mean MRSE for hyperopic retreatment was
the stromal bed was dried with a Merocel sponge (Solan) and was
C2.23 G 0.65 D (range C1.25 to C3.25 D); at the last
then ready for laser ablation. At the end of the photoablation, thecorneal flap was placed back in position without sutures, all debris
postoperative examination, it was C0.03 G 0.29 D (range
was irrigated out of the interface, and the flap was centrifugally
ÿ0.25 to C0.50 D) (P!.01). All patients (100%) were
swept with a Merocel sponge to allow adhesion to the stromal
within G0.75 D of emmetropia in MRSE. Approximately
bed. No contact lenses were used in the postoperative period.
77% of patients who had myopic retreatment lost no line
Eye protection with a hard shield was advised for the day after sur-
of best corrected visual acuity (BCVA); 17% had an increase
gery, and all patients were instructed not to rub their eye. For thefirst 5 days, patients received ofloxacin 0.3% drops and butyrate
of 3 lines and 6% of 5 lines. Eighty-two percent of the pa-
clobetasone 0.1% drops 3 times a day. Then they received only bu-
tients who had hyperopic retreatment neither lost nor
tyrate clobetasone 0.1% drops once a day for 10 days.
gained a line of BCVA; 18% increased by 1 line.
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
Table 4. Uncorrected visual acuity and BSCRA, MRSE, and pachymetry at final visit after topographically guided PRK retreatments (32 patients).
Corneal Thickness (mm)
(ÿ0.50 to C0.75)
(ÿ0.25 to C0.50)
BSCVA Z best spectacle-corrected visual acuity; MRSE Z manifest refraction spherical equivalent; UCVA Z uncorrected visual acuity
was 40.15 G 3.36 D (range 35.23 to 47.40 D) (P Z 0.02).
The mean preoperative refractive astigmatism was 1.0
The mean MRSE for myopic retreatment was ÿ2.36
0.99 D (range 0.14 to 3.78 D); post-retreatment it was
1.29 D (range ÿ1.50 to ÿ4.75 D); at the last postoperative
examination, it was ÿ0.11
G 0.72 D (range 0.19 to 2.99 D) (P!.01).
G 0.23 D (range ÿ1 to C1.25 D)
(P!.001). Mean MRSE for hyperopic retreatment was
C1.94 G 0.97 D (range C0.50 to C2.50 D); at the lastpostoperative examination, it was C0.06 G 0.54 D (range
The mean preoperative SimK value was 40.44 G
ÿ0.25 to C0.50 D) (P!.01). Nine eyes (82%) were within
3.72 D (range 36.16 to 46.44 D); after retreatment the
G0.5 D of emmetropia in MRSE and 2 (18%) were within
mean SimK was 38.29 G 3.14 D (range 34.82 to 45.56 D)
G1 D. Thirty-three percent of patients who had myopic re-
(P Z .02). The mean preoperative refractive astigmatism
treatment neither lost nor gained a line of BCVA; 17% had an
was 1.34 G 0.80 D (range 0.47 to 3.12 D); after the retreat-
increase of 1 line, 17% of 2 lines, and 33% of 3 lines. No pa-
ment, it was 0.61 G 0.30 D (range 0.21 to 0.96 D) (P!.01).
tient who had hyperopic retreatment lost or gained a line ofBCVA.
Corneal Thickness
The information provided by videokeratographic sys-
The mean preoperative ultrasound central pachymetry
was 462.36 G 71.72 mm (range 417 to 567 mm); after re-
(SimK), of refractive astigmatism and qualitative–quantita-
treatment it was 433.40 G 38.23 mm (range 395 to 525 mm).
tive morphological information of the topographic indicesSAI and SRI. The topographic patterns improved in all eyes
(When the preoperative and postoperative SAI(0.64
The mean preoperative ultrasound central pachymetry
G 0.36 versus 0.73 G 0.34, respectively) and the
was 468.57 G 55.76 mm (range 413 to 570 mm); after the
G 0.36 versus 0.64 G 0.36, respectively) of the
TMS-3 videokeratographic maps were compared, the dif-
retreatment it was 388.33 G 48.30 mm (range 382 to
ferences reached statistical significance (P!.05 in both
The mean endothelial cellular density (ECD) and coef-
The mean preoperative SimK value was 41.43 G 2.73 D
ficient of variation (CoV) were unchanged in both groups
(range 35.74 to 47.33 D); the mean post-retreatment SimK
during the entire follow-up.
Table 5. Uncorrected visual acuity and BSCVA, MRSE, and pachymetry at final visit after topographically guided LASIK retreatments (10 patients).
Corneal Thickness (mm)
(ÿ0.25 to C0.50)
BSCVA Z best spectacle-corrected visual acuity; MRSE Z manifest refraction spherical equivalent; UCVA Z uncorrected visual acuity
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
12 Months
24 Months
36 Months
12 Months
24 Months 36 Months
Spherical equivalent (D) -4.00
Spherical equivalent (D) -4.00
Figure 1. Change in MRSE over time after topographically guided trans-
Figure 3. Change in MRSE over time after topographically guided LASIK
epithelial PRK myopic retreatment (number of eyes).
myopic retreatment (number of eyes).
(from 0 to 5).After the primary treatment, no eye in this
The mean ECD was 2147.83 G 107.47 cells/mm2
series of patients presented a haze score greater than 1. In
(range 1893 to 2341 cells/mm2) and 2101 G 124.04
Group A, corneal haze registered a peak between 3 and
cells/mm2 (range 1688 to 2542 cells/mm2) preoperatively
6 months after the retreatment and afterwards decreased
and postoperatively, respectively (PO.05). The mean CoV
gradually; no patient presented in the last examination
was 45.32 G 4.88 cells/mm2 (range 39 to 57 cells/mm2)
a haze score grater than 1. Interface haze after LASIK re-
and 44.06 G 5.21 cells/mm2 (range 34 to 54 cells/mm2)
treatment (Group B) was minimum (trace) or absent. No
preoperatively and postoperatively, respectively (PO.05).
case of epithelial ingrowth, debris, diffuse lamellar kerati-tis, infections, or keratectasia occurred.
The mean ECD was 2122.18 G 129.78 cells/mm2
(range 1928 to 2298 cells/mm2) and 2039.10 G 133.42
Excimer laser PRK and LASIK have proven to be effec-
cells/mm2 (range 1726 to 2216 cells/mm2) preoperatively
tive and safe techniques to correct low to medium refractive
and postoperatively, respectively (PO.05). The mean CoV
errors. Unfortunately, regressions toward the initial myopic
was 44.21 G 7.90 cells/mm2 (range 38 to 53 cells/mm2)
or hyperopic state and overcorrection are serious problems,
and 42.77 G 4.65 cells/mm2 (range 35 to 50 cells/mm2)
limiting the predictability of excimer laser refractive out-
preoperatively and postoperatively, respectively (PO.05).
come. An estimated 10% to 20% of patients require en-hancement after PRK and 5.5% to 28% after LASIK.
Corneal Complications
Retreatment of a patient who has had excimer laser refrac-
No case of delayed reepithelialization was noted. Ante-
tive surgery calls for careful consideration. Possible causes
rior stromal haze was evaluated using Heitzmann criteria
of regression after PRK and LASIK surgery depend on
12 Months
24 Months
36 Months
12 Months
24 Months
36 Months
Spherical equivalent (D)
Spherical equivalent (D)
Figure 2. Change in MRSE over time after topographically guided trans-
Figure 4. Change in MRSE refraction over time after topographically
epithelial PRK hyperopic retreatment (number of eyes).
guided LASIK hyperopic retreatment (number of eyes).
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
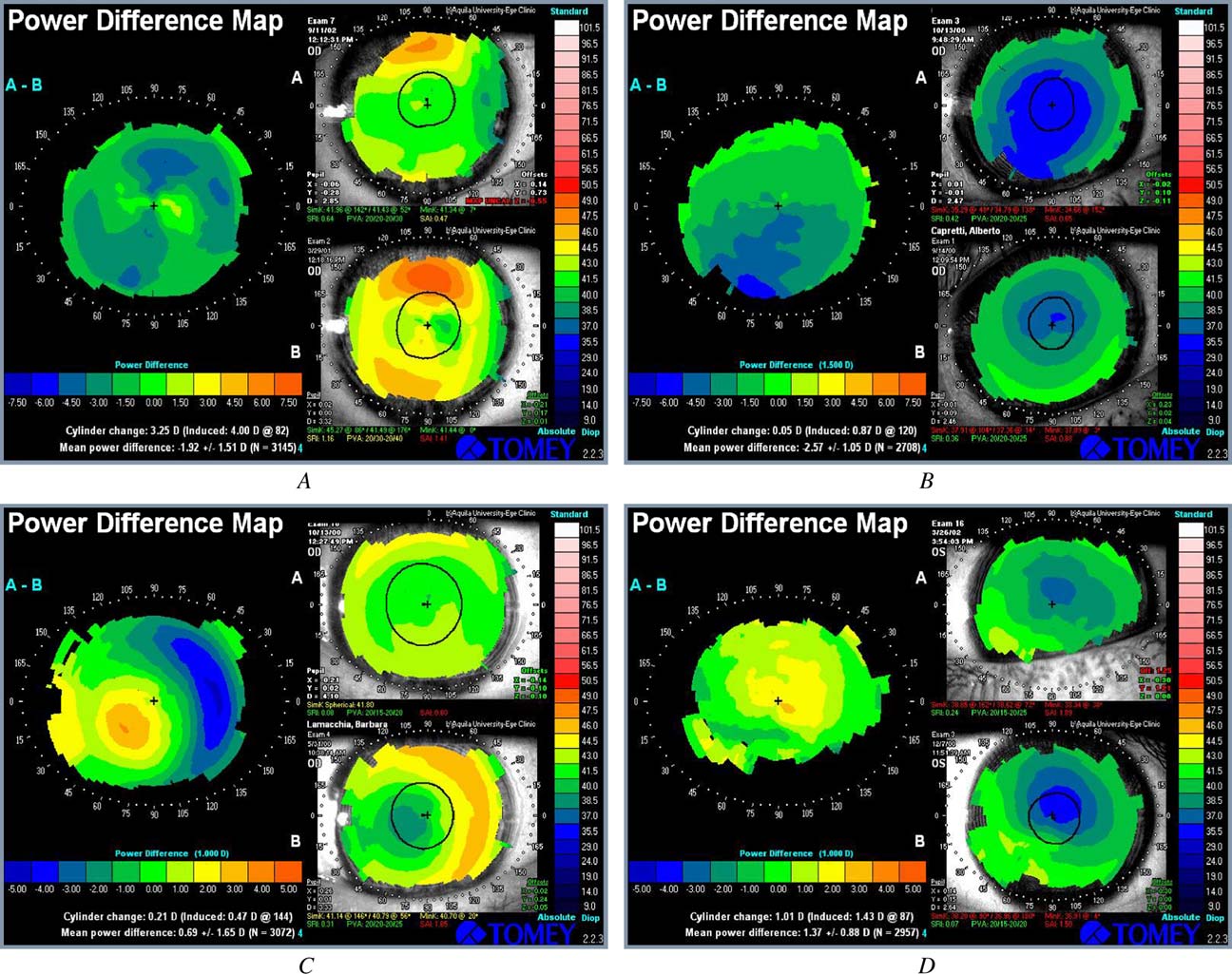
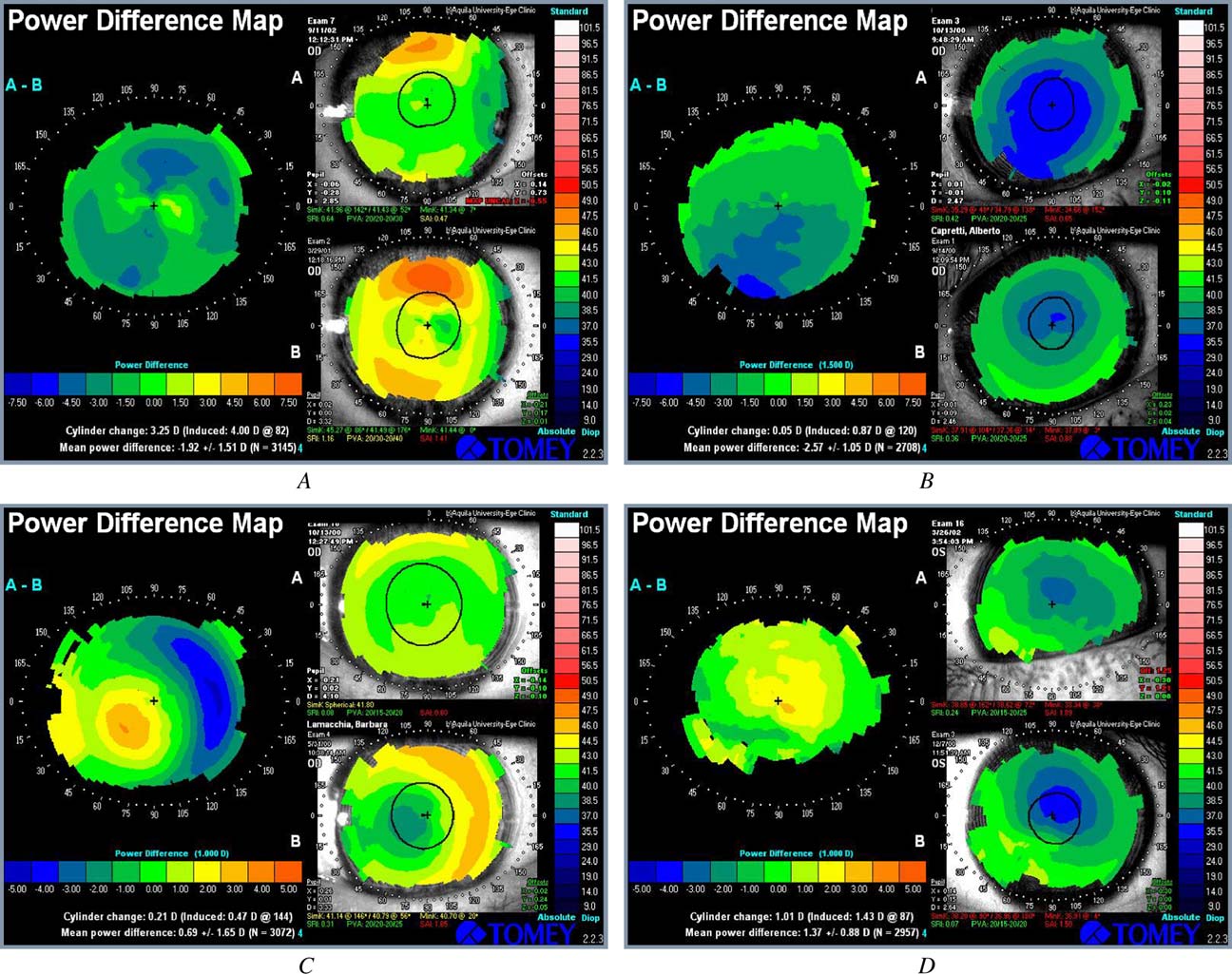
Figure 5. The differential map (left) highlights the improved corneal profile obtained before (bottom right) and after (top right) topographically guided trans-epithelial PRK or LASIK. A: Patient SS, woman, 35 years old. Preoperative MRSE was ÿ6.75 with a BSCVA of 20/20. Four years after PRK, the refractive error wasÿ1.25 (BSCVA 20/20). The calculated TOSCA ablation in the optical zone was 85 mm and the epithelial thickness, 55 mm. Using TSA software, 55 mm ablationwas added for an overall superficial corneal ablation of 140 mm in the optical zone (including epithelium). The final postoperative MRSE was plano witha BSCVA of 20/20. B: Patient CA, man, 42 years old. Preoperative original MRSE was ÿ9.00 D with a BSCVA of 20/20. Four months after LASIK, the refractiveerror was ÿ1.75 D (BSCVA 20/30). The calculated TOSCA ablation in the optical zone was 123 mm. The final postoperative MRSE was ÿ0.25 with a BSCVA of20/20. C: Patient LB, woman, 35 years old. Preoperative MRSE was ÿ6.50 D with a BSCVA of 20/20. Eight months after PRK, the refractive error was C2.00 D(BSCVA 20/20). The calculated TOSCA ablation in the optical zone was 48 mm and the epithelial thickness, 51 mm. Using TSA software, 51 mm ablation wasadded, for an overall superficial corneal ablation of 99 mm in the optical zone (epithelium included). The final postoperative MRSE was plano with a BSCVA of20/20. D: Patient DL, man, 54 years old. Preoperative MRSE was ÿ7.25 D with a BSCVA of 20/20. Two months after LASIK, the refractive error was C2.50 D(BSCVA 20/20). The calculated TOSCA ablation in the optical zone was 58 mm. The final postoperative MRSE was ÿ0.25 with a BSCVA of 20/20 (PVA Z po-tential visual acuity; SAI Z surface asymmetry index; SRI Z surface regularity index).
patient, type of instruments, parameters of treatment, and
healing process to the laser treatment or to biomechanical
different postoperative therapy. The surgeon should deter-
changes in the cornea. Variability of stromal repair can de-
mine and consider any errors in evaluation and perfor-
pend on patient's general conditions and age. The presence
mance. Refraction, biomicroscopy, and videokeratography
of general pathologies associated (tendency toward hyper-
are required to detect any changes in corneal curvature
glycemia or diabetes) can delay reepithelialization; even
that might have occurred during follow-up in response to
diseases of immune system can determine changes in the
pharmacologic therapy. If the initial refractive procedure
healing process.An adequate production in quantity, but
was correctly conducted, the reason for failure is related
mainly in quality, of tear film is essential for correct lami-
to the individual's biological response in terms of abnormal
nation of the epithelium during healing process.The
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
ENHANCEMENTS AFTER TOPOGRAPHICALLY GUIDED PRK AND LASIK
important factors that result from photoablative surgical
procedures are the quality of surface ablation and the crea-
1. El Danasoury MA, El Maghraby A, Klyce SD, Mehrez K. Comparison of
tion of a new corneal profile which do not induce an epithe-
photorefractive keratectomy with excimer laser in situ keratomileusis
lial hypertrophy, with significant curvature variations.
in correction low myopia from ÿ2.00 to ÿ5.50 diopter; a randomized
Finally, postoperative topical therapy can modulate the
study. Ophthalmology 1999; 106:411–420; discussion by JH Talamo,
evolution of refraction during the assessment after PRK
and minimize the appearance of corneal haze.Decentra-
2. Alessio G, Boscia F, La Tegola MG, Sborgia C. Topographically-driven
excimer laser for the retreatment of decentralized myopic photore-
tion of treatment, the presence of a small optical zone (eval-
fractive keratectomy. Ophthalmology 2001; 108:1695–1703
uated through computerized corneal topography), and
3. Tamayo Fernandez GE, Serrano MG. Early clinical experience using
an overcorrection may determine the request for a
custom excimer laser ablations to treat irregular astigmatism. J Cata-
ract Refract Surg 2000; 26:1442–1450
The success rate of enhancement is generally lower
4. Daush D, Schro¨der E, Dausch S. Topography-controlled excimer laser
photorefractive keratectomy. J Refract Surg 2000; 16:13–22
than that of the primary procedurThe risk factors
5. Heitzmann J, Binder PS, Kassar BS, Nordan LT. The correction of high
for retreatment include degree of attempted correction, ini-
myopia using the excimer laser. Arch Ophthalmol 1993; 111:1627–1634
tial and residual astigmatism, age, and sex.
6. Gartry DS, Larkin DFP, Hill AR, et al. Retreatment for significant regres-
The recently introduced excimer laser customized ab-
sion after excimer laser photorefractive keratectomy; a prospective,
lation seems to be a powerful technique to treat corneal
randomized, masked trial. Ophthalmology 1998; 105:131–141
7. Hersh PS, Fry KL, Bishop DS. Incidence and associations of retreatment
irregularities and may increase the success rate in retreat-
after LASIK. Ophthalmology 2003; 110:748–754
ments.In the present study, we found, after a mean fol-
8. Wilson SE, Mohan RR, Hong J-W, et al. The wound healing response
low-up of almost 2 years, an improvement in MRSE from
after laser in situ keratomileusis and photorefractive keratectomy; elu-
ÿ2.54 to ÿ0.05 for PRK myopic retreatments and
sive control of biological variability and effect on custom laser vision
from ÿ2.36 to ÿ0.11 for LASIK myopic retreatments;
correction. Arch Ophthalmol 2001; 119:889–896
9. Spadea L, Fasciani R, Necozione S, Balestrazzi E. Role of the corneal
from C2.23 to C0.03 for PRK hyperopic retreatments
epithelium in refractive changes following laser in situ keratomileusis
and from C1.94 to C0.06 for LASIK hyperopic retreat-
for high myopia. J Refract Surg 2000; 16:133–139
ments. All patients had a refractive error within G0.75 D
10. Lyle WA, Jin GJC. Retreatment after initial laser in situ keratomileusis.
after the PRK enhancement and within
J Cataract Refract Surg 2000; 26:650–659
G1.00 D after the
LASIK enhancement. Also, the topographic patterns signi-
11. Lipshitz I, Lowenstein A, Varssano D, Lazar M. Late onset corneal haze
after photorefractive keratectomy for moderate and high myopia.
ficatively improved in all eyes for SAI and for SRI topo-
Ophthalmology 1997; 104:369–373; discussion by JH Talamo, 373–374
graphic indices, and the UCVA results were 20/50 or
12. Spadea L, Bianco G, Balestrazzi E. Four techniques for retreatment
better in PRK retreatment group and 20/30 or better in
after excimer laser photorefractive keratectomy. J Refract Surg 1996;
LASIK retreatment group. These results are better if com-
pared with the results obtained using standard PRK and
13. Spadea L, Colucci S, Bianco G, Balestrazzi E. Long-term results of exci-
mer laser photorefractive keratectomy in high myopia: a preliminary
LASIK retreatment techniques.
report. Ophthalmic Surg Lasers 1998; 29:490–496
The choice of performing a transepithelial ablation
14. Pop M, Aras M. Photorefractive keratectomy for regression; one year
is secondary to the consideration that the epithelial layer
follow-up. Ophthalmology 1996; 103:1979–1984
might change and mask the corneal surface irregularity.
15. Snibson GR, McCarty CA, Aldred GF, et al. Retreatment after excimer
Therefore, when adopting a topographically guided exci-
laser photorefractive keratectomy; the Melbourne Excimer LaserGroup. Am J Ophthalmol 1996; 121:250–257
mer laser PRK, an epithelium inclusive videokeratography
16. George SP, Johnson DG. Photorefractive keratectomy retreatments;
map is used, which uses the epithelium like a masking
comparison of two methods of excimer laser epithelium removal.
agent. On the other hand, we accept the risk of creating
Ophthalmology 1999; 106:1469–1480
a small irregular ablation when the laser is applied to
17. Pe´rez-Santonja JJ, Ayala MJ, Sakla HF, et al. Retreatment after laser in
some points on the epithelium and to others on the stroma
situ keratomileusis. Ophthalmology 1999; 106:21–28; discussion byME Whitten, 28
as the result of different ablation rates.
18. Rashad KM. Laser in situ keratomileusis retreatment for residual myo-
In conclusion, the enhancement techniques using to-
pia and astigmatism. J Refract Surg 2000; 16:170–176
pographically guided excimer laser photoablation with to-
19. Mulhern MG, Condon PI, O'Keefe M. Myopic and hyperopic laser in
pographically supported customized ablation method may
situ keratomileusis retreatments; indications, techniques, limitations,
obtain a satisfactory and stable visual outcome with good
and results. J Cataract Refract Surg 2001; 27:1278–1287
20. Seiler T, Kriegerowski M, Schnoy N, Bender T. Ablation rate of human
safety and efficacy and no vision-threatening complications
corneal epithelium and Bowman's layer with the excimer laser
in selected cases after PRK and LASIK.
(193nm). Refract Corneal Surg 1990; 6:99–102
J CATARACT REFRACT SURG - VOL 31, DECEMBER 2005
Source: http://www.ivistechnologies.it/localhost/ivis_site/files/documents/24Spadea2005.pdf
Diagnóstico y tratamiento de la Luis Miguel Rodríguez Fernández1 Salvador Gracia Manzano2 1Unidad de Nefrología Pediátrica Servicio de Pediatría. Hospital de León 2Nefrología Pediátrica. Hospital Universitario Virgen de la Arrixaca. Murcia deben producirse a una edad socialmente (¿A qué llamamos enuresis nocturna y qué
Ebook Word Document: Complimentary Treatment Strategies for CFS IBS and many other immune related illnesses – the recovery plan I followed that cured my CFS: Please note that below treatment strategies are only to complement existing treatment and in no way replace current medical treatment The following is a brief summary of some notes from . This book literally saved my life and I was so greatful that I came across it. I really suggest you buy Patient Health self from Amazon or the Maker's diet as it's an essential recovery tool for anyone who is seriously unwell. I want to firstly say that I am in no way affiliated with any of the below products mentioned, there is no benefit in me telling you this important knowledge and no this is not some MLM marketing propaganda - I simply want you to know this amazing program that saved my life and may help you – everyone should know about this. And it is not only important for anyone who wants to recover from bowel problems but basically it may help recovery from any illness that is affected by a weak immune system.