Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Microsoft word - lf surg. handbook-eng2nded1.doc
LYMPHATIC FILARIASIS MORBIDITY PROJECT
SURGICAL HANDBOOK
An Aid to District Hospital Surgeons
2nd edition, Summer 2007
LF -Filaricele surgery handbook*
IMPORTANT NOTICE: Techniques described in this Handbook
are only for treating LF patients who have normal scrotal skin!
Surgical techniques described here and during The West Africa LF-
Morbidity Project's training workshops are contraindicated in
patients with significant lymphoedema of the scrotal skin,
elephantiasis of the scrotum, or lymph-scrotum. Such conditions
may generally require reconstructive surgery.
In such cases, both procedures (filaricele resection and
reconstructive urogenital surgery) should be done in a single
session and using a different surgical technique on the LF-hydrocele
sac.
Reconstructive LF-surgery must always be undertaken at tertiary-
care hospitals by expert surgeons who have extensive experience in
skin transplants and the highly specialized care of such LF-related
conditions.
Techniques described here are only for use on "ordinary" cases of
LF-hydrocele/filaricele that are uncomplicated by skin
manifestations.
Note for the 2nd edition:
The technique taught here has been well received and produces good results in the
hands of African district hospital doctors. This 2nd edition has been updated and
modifications introduced based on three years of experience teaching LF-hydrocele
surgery and outcomes evaluations that showed some clarifications to be necessary.
* Presentation of information in this handbook does not constitute "publication". Information is
presented here as an aid to memory especially for surgeons participating in educational LF-surgery workshops under the West African LF-Morbidity Project. This is not intended as adefinitive text. A more in-depth text is being prepared for publication by Prof. J. Noroes ofRecife, Brazil, who has contributed massively to the preparation of this handbook through hisyears of research and clinical work on LF, as well as to wording in the Handbook itself. Anymistakes are nevertheless the fault of the authors. Material in this booklet may be reproduced,extracted, or copied in part or in whole, for educational, purely non-commercial purposespertaining to national LF Elimination activities, and on the condition that the authors arerecognized. Rights are retained by the authors.

LF-hydrocele / filaricele, a debilitating, impoverishingcondition that afflicts an estimated 40 million men in 83countries.
This 50 year old incapacitated farmer with 5 children hadhis filaricele for 20 years. It contained 4.2 liters of fluid,making farm work and procurement of income for hisfamily all but impossible.

A 35 year old man whose scrotum contained approximately2 litres of fluid, significantly hampering him in his work asa farmer. His wife had left him because of his condition.
Table of Contents
Patient overview and medical / surgical history form
Pre-op. laboratory investigations
Transillumination to light
Ultrasonography of the scrotum
Informed consent form
Other pre-operative necessities
Intra-operative requirements and procedures
Post operative care
Local anesthesia for LF-hydrocele / filaricele
Relevant anatomical highlights
Patient care and follow-up form
Data collection form-socioeconomic impact; surgery outcomes
Recipe for permanganate solution
Equipment list – Instruments and Disposables for LF surgery
PATIENT OVERVIEW AND MEDICAL / SURGICAL HISTORY FORM1.1.
Name of the patient
Date of birth if known (age)
Address: (Home town/village; house name or number where available)
Marital status/Number of wives/Number of children/Widower/Divorcee
Date of first consultation
ABOUT THE FILARIAL DISEASE2.1.
Duration of scrotal swellingOn the Right side:
On the left side:
Clinical diagnosis:Right side filaricele: small ( ) medium ( ) large ( )Left side:
small ( ) medium ( ) large ( )
Additional urogenital LF clinical manifestations:
Status of filarial infection (MF-status; antigen card test result)
TYPE OF LF SURGERY4.1.
PAST MEDICAL HISTORY
PAST SURGICAL HISTORY
CURRENT MEDICATIONS (include aspirin etc.)
Large or chronic alcohol consumption? (important for the anaesthesia )
Physical examination
(More information and photos concerning physical examination, p. 8-11)
Status of hygiene at 1st consultation: good ( ); reasonable ( ); bad ()Comments:
State of conjunctiva:NOTE: This is mainly to assure against operating on a jaundiced patient, e.g. in situations whereroutine pre-operative liver-function tests may not be available. It will also give warning ofpotentially severely depressed haemoglobin (Hgb) level / severe anemia. Hgb should in all casesbe measured pre-operatively.
SCROTAL EXAMINATION
Inspection of the skinLook for skin infection and entry lesions of all kinds, lymphoedema,lymph-scrotum, warts etc.
NOTE: It is very important to rule out any infection of the skin, even if it is outside of the genitalarea. Urethritis should also be ruled out or treated prior to any urogenital surgery.
9.4.2. Palpation findings
Determine whether the swelling is purely scrotal or inguino-scrotal.
You are trying to determine whether the swelling is a filaricele, ahernia, or a filaricele and a hernia in the same patient.
NOTE: The point is that the surgery is different, with the incision placed very differently, ifhernia is involved.
9.4.3. Transillumination / Ultrasound findings
(see p. 8-11 regarding transillumination and ultrasound)
9.5. Status of the penis
Detect any lymphoedema and/or urethral secretion, or other skinlesionsNote: Urethritis and any infected skin lesion should be treated prior to any urogenital surgery.
9.6. Examine the limbs
Verify the presence or absence of any lymphoedema, entry lesion(s),and/or skin infection.

10. Pre-operative Laboratory Investigations
10.1 Haemoglobin:
10.2. Filariasis blood tests:
10.2.1 Thick blood film for microfilaria:
Photo 1. Microfilaria in thick blood film stained with Geimsa; x400 lens.
10.2.2. Antigen Card Test result (if done):
Simple urinalysis for protein, sugar, red blood cells, etc.
Urinalysis Results:
If urine-sugar positive, one should measure serum blood-sugar.
Blood sugar result:
NOTE: Deal with any diabetes before considering operation for LF-hydrocele/filaricele. Onlypatients with stable, normal or essentially normal blood sugar should be considered for scrotal
surgery because of the elevated risk of post-operative infection that comes with inadequatelycontrolled diabetes.
Results of any other blood tests done:
(End of patient registration form, p. 5 - 7)

Photo 2. Lymphoedematous penis and scrotum where operation is contraindicated at normal
district and regional hospitals.
Transillumination to light
NOTE: Transillumination is non-specific and not considered an adequate tool for pre-operatively assessingcases believed to be LF-hydrocele. If positive, it means there is a thin sac wall and may indicate fairly clearfluid in the sac, but it reveals nothing about the origin of that fluid. Where ultrasound is available,
transillumination is not necessary, as it offers no additional information.
Where possible, the patient should always be examined using ultrasound to differentiate between congenitalhydrocele on the one hand, and LF-associated conditions with lymphangectasia on the other hand, detectpossible worm-nests and determine their location, etc. Also, ultrasound permits proper pre-operativeassessment of the testis, etc, which is important.
Transillumination is mentioned here, only because some consider that it provides a little useful informationin hospitals that do not have access to ultrasound examination.
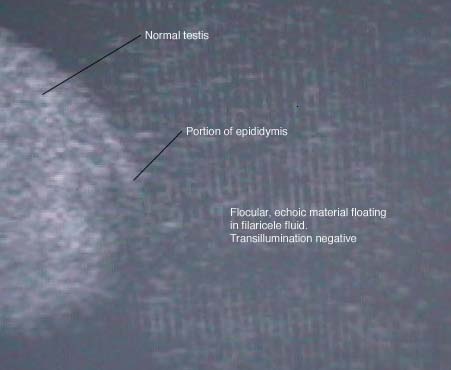
NOTE: If transillumination is negative, it means one may be facing a complex situation (including possibletumor, chylocele, etc). Negative transillumination occurs quite frequently even in LF-hydrocele, in cases
where the sac wall is thick, and in some cases where the fluid contains significant amounts of blood or othercellular matter; in some cases where the lymph fluid in the filaricel has had access to the testis and led totesticular necrosis with testicular matter mixed in with the fluid, etc. Differentiation from tumor is oftenpossible based on palpation and other clinical findings. Careful palpation is more reliable thantransillumination for differentiating from tumor. Cases with negative transillumination can be operated onin district hospitals if the surgeon is prepared to deal with situations that may not be typical filaricele. In
cases where transillumination is negative, you may consider referring the patient to a secondary hospital,depending on your hospital's surgical equipment and your own level of experience as a surgeon.

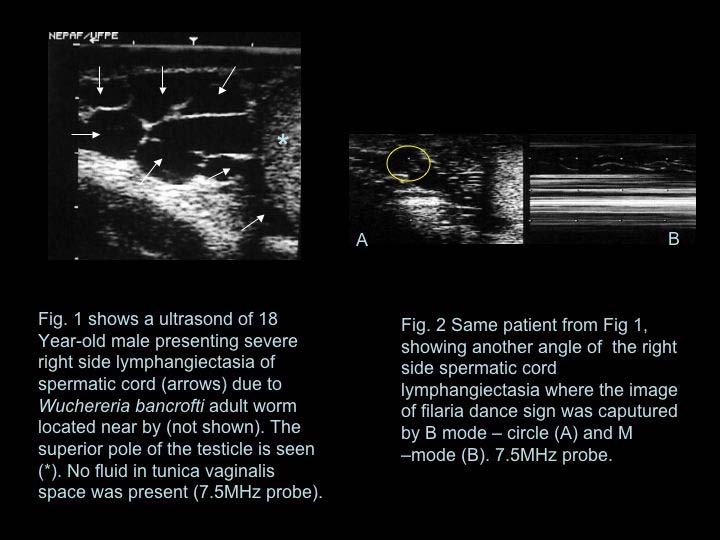
Photo 3. Transillumination test positive, much more obviously so than is usual.
Ultrasonography of the scrotum
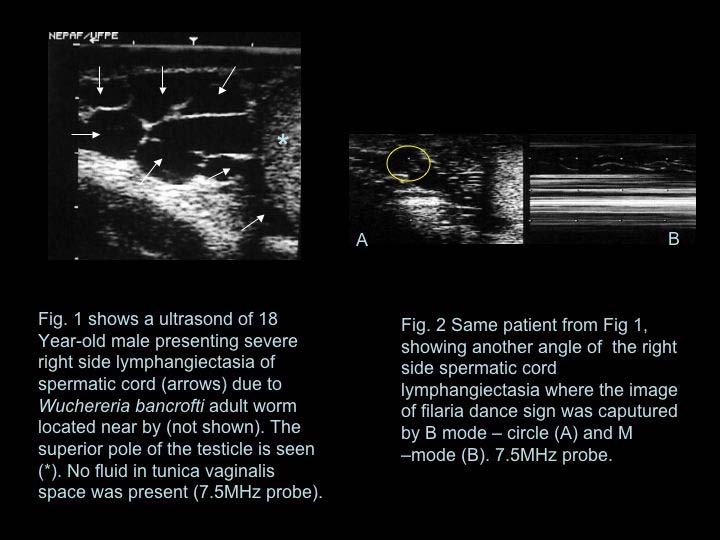
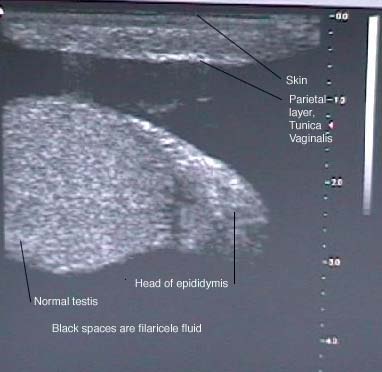
NOTE: Where available, ultrasonography at 7.5 mHz is considered important for differentiating conditionslike epididymal cyst, varicocele, and testicular tumour. It also helps you know the state of the testis beforesurgery, whether it's atrophic or not. Accuracy of ultrasound examination is examiner-dependent, and thetool is generally not yet available in some West African district hospitals.
Photo 4. Lymphangectasia along the spermatic cord
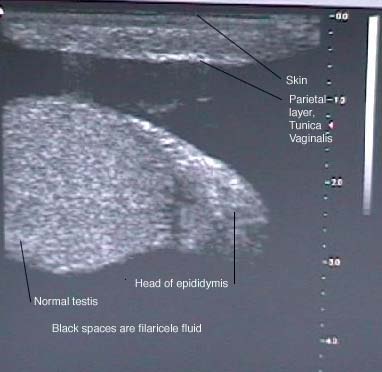
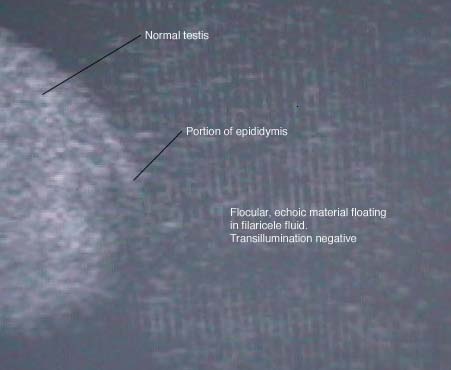
Photo 5. Typical LF-hydrocele/filaricele, black, anechoic fluid around a normal testicle
(transillumination positive). Epididymis to the right and above the testis.
Photo 6. Filaricele/LF-hydrocele with flocular, richly echoic particles in the fluid
Examination of the limbs for signs of oedema, entry lesions, and/or skininfection.
Limb oedema with fibrotic skin. The appearance here is consistent with venous insufficiency.
I . consent to undergo the operation of filaricele surgery,the consequences of which have been explained to me.
This operation will be done under anaesthesia, and I will be in hospital for oneweek, after which I will be discharged and I will be coming for dressings until mywound heals completely. Possible complications that sometimes occur aftersurgery even though the surgeon will do what (s)he can to avoid them include oneor more of the following: bleeding (haemorrhage), blood collection in the scrotum(haematoma), infection (fever etc), return of the problem, etc.
I have been explained that I must take 2 types of anti-infection tablets(antibiotics), three times each day for at least 5 days after the operation.
I have been explained and I understand that it is very important to take the tabletsexactly in the way I have been instructed, for the entire 5-7 day period of thetreatment. I understand that taking these tablets in the right way is very importantfor a good result of the surgery. I have also been explained that I will be giventablets to take against any pain after the operation, and I have been explained howto take those tablets.
I also agree that photos or clinical data about my condition, its treatment and theresults may be used in research and scientific publications.
Other pre operative necessities
Good bath with thorough washing of the genital area but also the wholebody using soap and water, both the day before surgery and on the morningof surgery.
2. Close-cutting or shaving of scrotal hair
The day before the operation, after the head-to-toe washing, the patientshould be provided a good scissors and instructed that he is to carefully cutall genital hair, especially that on the scrotum but also the rest of his pubichair. He is to cut hairs very close to the skin, being careful not to damage theskin itself.
In many localities, carefully shaving the skin is seen as the only acceptablepre-operative method for hair removal. Shaving should be done with extremecare to avoid damaging scrotal skin. Skin damage makes infection morelikely.
NOTE: In some centres it is considered important not to shave the skin as they see evidence that post-operative infections are perhaps more common after shaving, as a result of small nicks and cuts of the skinduring the shaving process. The evening before surgery, staff needs to confirm a proper result has beenobtained by the patient, and that all public hair has been cut very short, especially on the scrotum.
3. Pre-operative antibiotic dose**
The initial dose of both antibiotics (see the first item of Post-Operative Care,below) must be started the day before surgery and a dose of both antibioticsgiven on the morning of surgery. In our setting it is considered veryimportant for the patient to be under proper antibiotic coverage during theoperation itself. Depending on the type of anesthesia chosen, the patient mayneed to be fasting or on only small amounts of liquids during the day ofsurgery. Experience in rural African settings shows very clearly thathydrocele surgery of all types needs to be done under a proper antibioticumbrella. Otherwise you risk an unacceptably high rate of post-operativeinfections, and even disastrous outcomes.
** Because of the high risk of post-operative infections in settings where this handbook will be used inWestern Africa, and the often disastrous consequences of such infections when they occur in and aroundthe genitalia, the Project Urologist suggests that surgeons working in peripheral African hospitals shoulddefinitely use pre- and post-operative systemic antibiotic medication as specified below. The fact thatpost-operative infections have been seen in 25%-30% of cases following filaricele surgery in Africancountries, regardless of surgical methodology, supports this Project's recommendation to use pre- andpost-operative antibiotics for filaricele surgery in our setting. In some other settings, antibiotic coverwould not be recommended for filaricele surgery because it would be adequate to treat only the very fewpatients who experience post-operative infections in those other settings. In general, it is best for thepopulation and the individual patient that doctors avoid using antibiotics except when really needed.
4. Morning Temperature on day of surgery
Consider postponing surgery if the patient's temperature on the morning ofsurgery is >37.5 degrees Centigrade. If so, also take a blood sample formalaria microscopy and other measures to diagnose and treat any infection,so surgery may become possible as soon as possible.
C. Intra-operative Requirements and Procedures
PLEASE SEE IMPORTANT NOTE INSIDE THE FRONT COVER!
1.1. Pre-Operative Medication
a. Diazapam 10 mg i.v. just before surgery .
b. Pethidine 50 mg. i.m. e.g. when the surgeon starts scrubbing, keeping the
remaining 50 mg. available for the not so rare cases where more isneeded. (Pethidine may not be available in some countries. Tramadol 50 mg. can then be injectedas an anti-inflammatory analgesic.)
1.2. Per-Operative Anaesthesia
Local, spinal, or (rarely in Africa) general anaesthesia
Local anaesthesia will be the norm in many hospitals in our settings. (Pleasesee Annex 2 for more details.) Spinal or general anaesthesia may bepreferred when one has an anaesthetist available with the skill and equipmentto do it.
Local anaesthesia (Xylocain with adrenaline) is placed as follows:
a) 5 ml. in and just on the ventral aspect of both spermatic cords near the
external ring of the inguinal canal; b) along the median raphae; c) infiltrated
well on both sides of the median raphae.
NOTE: Where available, bupivacaine (in a 1:1 dilution with normal saline or water ad inj.) gives a strongand longer lasting effect, and thus requires less drug for the same local anesthesia time. It may thereforealso be less costly all told. However, in most of our settings, bupivacaine may not be available.
As always, patients with a large alcohol consumption may need and tolerate different doses, sometimes behyper-reactive, need to be given special attention as concerns fluid and sometimes sugar intake, etc.
Total xylocain usage is typically 50 – 70 ml. Maximum total dose: < 400 mg.
Somebody should be sitting at the head of the patient throughout the procedure, not least under localaneasthesia, to register the patient's condition and to react promptly if facial contraction or other signsindicate that additional, top-up anaesthetic needs to be injected in and in front of the cord. The patient andthe surgeon both benefit if the patient is free of pain.
When top-up xylocain is given, you should give at least 5 ml at a time. 10 ml. is usually better.
Also, consider topping up the pethidine dose. Many patients, especially young men, need and tolerate a
topping up of their pethidine dose with an additional 25-50 mg, to a total doe of 75-100mg.
Alcoholics and persons with considerable alcohol consumption need special care. They can become agitatedat surgery and hypoglycaemic. The liver of such persons may not easily release glucose under stress.
Therefore, access to a dextrose drip or sugar cubes and a bit of water in the form of soaked compresses thatthe patient can suck on is important in such cases.
Thorough cleaning of the genital area with soap (e.g. ordinary liquid dish-washing soap) and water is undertaken on the operating table. This is donein addition to the patient's shower the previous evening, before the thoroughpre-operative skin-disinfection of the genital area by the surgeon.
The pre-operative day and on the morning of surgery, as well as on theoperating table, be sure to clean under the preputium in uncircumcised men!
3. Midline incision
The incision is along the median raphae of the scrotum, beginning about2cm (about two finger-widths) below the base of the penis and extendingfor a distance of typically 5-7cm, depending on the size of the filaricele.
Total, gentle dissection of the filaricele. As part of the dissection, thefilaricele is pressed out through the surgical incision, being careful to avoidrupture if possible.
Photo 8. Successfully exposed filaricele
NOTE: When the filaricele is truly huge and heavy, the spermatic cord will often be highly stretched.
Dissection must be done very carefully in such cases. In one documented case, the spermatic cord broke
and the LF-hydrocele fell off the operating table onto the floor, previously viable testicle and all, when acareless surgeon allowed a huge LF-hydrocele to slip.
Very Meticulous Hemostasis of any bleeding from the edges of the skin and the inner
surface of the scrotal wall and the outer surface of the filaricele sac is very important at
this point in the procedure, before proceeding to the next step.
Gauzes or compresses should be left in the hemi-scrotum cavity to minimize bleedingby compression and to give us an idea about the extent of any bleeding. This maneuverwill help us to review the hemostasis at the end of the procedure.
NOTE: A cautery machine will be of great help during the haemostasis. You should seriously consider refraining from filaricelesurgery if you do not have access to cautery, because the number of small bleeders can sometimes and unpredictably, thoughby no means always, be considerable and otherwise require a significant number of ties.
NOTE: You should repeatedly return to haemostasis on all structures dealt with during previous steps in the procedure.
Soaked compresses should be replaced frequently, and used as an indicator of whether and where there may be ongoingbleeding. And any such bleeding should be taken care of. Many small veins may not bleed immediately, while structures arelifted from the surface and tissues are handled during the procedure. The small veins may only start oozing when the spermaticcord and testis are left lying still for a few minutes.
Aspirate the filaricele fluid with a large syringe or a suction device, and note thenature and amount (ml.) of fluid aspirated.
Open the filaricele sac; inspect the testis; note any abnormalities.
Between two clamps a midline incision is made beginning in the anterior and superior
surface of the filaricele sac fairly near the tail of the epididymis and extended
cephalically until the limit of the spermatic cord.
Now it is possible to inspect the whole interior part of the filaricele sac, the testicle, and the epididymis.
NOTE: In cases being treated for recurrence after a previous intervention that included eversion of the tunica vaginalis, onemust at this point dissect the filaricele sac, separating it from the cord and other structures around which it will usually bewrapped, being careful not to damage the vas deferens and vessels in the spermatic cord. When the filaricele sac has been
liberated from other structures, it is resected as in other cases.
Photo 9. Filaricele sac wall has been opened on the ventral side, exposing the testis and the
epididymis. Both sides of the filaricele sac are clamped. Next, the lateral side will beresected 1-2 cm from the epididymis, and the median side will be excised 1-2 cm fromthe testis.
NOTE: If there is a peritesticular cyst, be sure to look for and ligate the small stalk of blood vessels that isnormally to be found in the cavity in which the cyst was located.
NOTE: If the filaricele has been very large, the vas deferens will often have been thinly stretched and may have anunusual location in the filaricele wall, making it difficult to recognize. Special care is therefore necessary in these cases,to avoid damaging the vas deferens during the dissection process.
NOTE: If the testis is seen to be obviously necrotic (Photo 10), the rest of the operation is simple in that youclamp the chord and perform a traditional orchiectomy.
Photo 10. Necrotic testis in a thick, fibrotic filaricele sac wall. (See Note above, under Step 7.)
Resecting the filaricele sac
Leaving approximately 1 – 2 cm. at the edge of the testis, and beingespecially careful at the epidydimis and the vas deferens, carefully resectthe filaricele sac. Check front and back several times, making sure thedirection of the scissors is appropriate, to avoid damage, and see that asuitable border is left unresected.
In long-standing cases or with chylocele, the filaricele sac may bethickened and fibrosed, and in extreme cases calcified, makingtransillumination negative and resection of the filaricele sac difficult.
Especially in patients with very large filariceles, the distance between theepidydimis and the testis may be increased. Leave the sac alone in this area!Do not resect any such additional tissue.
NOTE: If you ignore the advice to leave sac tissue located between the testis and the epidydimisalone, you will have all kinds of problems, and the bleeding is terrible!!
NOTE: Again, special care must be taken here, in order not to damage the vas deferens which may be thinand difficult to recognize in cases where the filaricele was huge and the cord was heavily stretched.
Photo 11. Resection of the filaricele sac around the testis
Haemostasis of the remaining filaricele sac edge
Use continuous interlocking 3-0 Vicryl sutures about 1 cm. apart at the cutedges of the tunica around the testis.
IMPORTANT NOTE: Vicryl knots tend to unravel! Therefore you must use 6 knots everywhere that youuse Vicryl, and you must leave 1 – 1.5 cm. of thread above the knot when cutting the thread.
If you ignore this advice, you run a high risk of having your beautiful surgery ruined by bleeding and otherproblems that result from sutures coming untied.
NOTE Regarding Suture Material: Vicryl is generally preferable to chromic catgut because Vicryl givesless local reactive inflammation. Vicryl is now available in most or all of our Project's countries.
Special caution is needed to avoid suturing the epididymis in patients ofreproductive age!
Photo 12. Interlocking sutures being placed along the filaricele sac's remaining edge
Haemostasis of the inner scrotal wall
When you think you are finished with Step 9, wrap the testis and cord in clean,
saline-soaked compresses, and leave the testis lying on the field. Wait 5 minuteswhile you inspect the inner wall of the scrotum and deal with any bleeding there, asdescribed in the paragraphs below. If there is no bleeding into the compress thathas been wrapped around the testis and cord, you have good hemostasis and canput the testis in the scrotum, as described below in Step 11.
Having gently wrapped the testis in clean gauze and set it aside,prepare to take out the gauze placed in the hemi-scrotal cavityearlier.
The scrotal pouch is opened widely with clamps, avoiding the skin. Thecompresses are removed, and the scrotal wall is inspected carefully.
Haemostasis is carefully and thoroughly secured on the inner wall of the
scrotum with electrocautery if available, and otherwise using 3-0 Vicrylties.
Placing the testis and dealing with the excessive scrotal skin
This is a good moment to review the haemostasis AGAIN and confirm thatthere is no bleeding in the scrotal cavity, after you have unwrapped thetestis and dealt with any bleeders that became evident while the testis waslying to the side since the end of Step 9.
Place the testis into the hemi-scrotal cavity. The testis should be placed atthe bottom and distally in the scrotum.
NOTE: If you do not place the testis as described, the testicle will later come to be located veryhigh in the scrotum and there will be a lot of skin inferiorly to it.
NOTE: Do not suture the testis to the scrotum. If you place the testis well at the bottom of the scrotum and
bandage as suggested below, the fibrosis that forms will be enough to keep the testis nicely placed in thescrotum. If the testis is not placed carefully at the bottom, on the posterior wall and distally, it may end upbeing located high up towards the inguinal canal.
Be sure there is no torsion of the cord!
Do not resect scrotal skin !
Even with a large filaricele, the size of the scrotum will have normalized considerablyeven during the operation itself.
If you place the testis gently but firmly at the bottom of the scrotum as suggested in Step11, the size of the scrotum will gradually become normal or close to normal later on.
If there was any undetected edema in the scrotal wall as a result of previous lymphaticfilariasis damage to scrotal lymphatics and lymph capillaries, partial excision of the skinwill not solve the problem, and you could worsen the situation if you resect scrotal skin.
Especially in our setting, in peripheral hospitals in Africa, but even elsewhere, it is
generally best not to excise any scrotal skin during LF-surgery.
Closure of the scrotum
The scrotal wall should be closed in 2 layers.
The inner layer should be sutured using interrupted or running, continuoussuturing with 3-0 Vicryl.
It is helpful to wash the area with Normal saline after closing of the innerlayer and just prior to closing the skin.
The outer wall (the skin) is closed, using 3-0 Vicryl, either asintracutaneous continuous suturing or interrupted sutures.
It is very important to achieve excellent approximation of the edges of the skin during surgical
wound closure. There is a tendency for the edges of the skin to bulge between sutures if care is not taken.
Gaps where subcutaneous tissue can be seen will delay wound healing by at least 2-3 weeks. This almostguarantees that you will have post-operative infection. Two – three minutes of care and attention to skinclosure at the operating table prevents weeks of trouble afterward.
In cases where the patient's possibility for personal hygiene may be bad, one may choose to
close the scrotal skin using Nylon sutures if you are absolutely sure the patient will return to have thesutures removed. In the great majority of cases one can use Vicryl , making subsequent removal of suturesunnecessary.
Photo 13 a, b. Closure of the scrotal wall in 2 layers: a) Inner scrotal wall; b) skin.
There is no need to put a drain in the scrotum before wound closure. Drainsdo not stop bleeding and haematoma formation. They only show the surgeonwhether bleeding is ongoing. Careful haemostasis during the procedure iswhat prevents bleeding. Also, drains increase the risk of infection.
Dressing and bandaging with crepe bandage.
14.1. Betadine* washing of the sutured surgical wound, twice;
* The term "Betadine" is used here because it is utilized in many West African settings as a generic term for skin disinfectantused in pre-operative skin preparation. Any disinfectant suitable for coming in contact with subcutaneous tissues can be used.
Also, please note: Some people react strongly against Betadine and other disinfectants containing iodine. If you see areas withchanged skin when opening the bandage, it is important to refrain from using Betadine or any related substance containingiodine for subsequent dressings and surgery.
14.2. Longitudinal compress;14.3. 2 layers of compress across the scrotum;14.4. Elastic band, 1st in direction of the longitudinal bandage, then
circularly being careful to also include the apex again and to includethe proximal aspect of the cord laterally as high as possible, and upto but not around the penis;
14.5. Tape the end of the elastic bandage to avoid subsequent unraveling
(rather than using the clips supplied with the elastic bandage);
14.6. Apply a suspending tape from one side of abdomen via the apex of
scrotum to other side of abdomen, with gentle degree of "lift" ortension in it.
Photo 14 a – e. Steps in bandaging the scrotum
NOTE: Both surgeons should definitely stay for the bandaging process!
It is very difficult to apply the bandage and get appropriate tension on the crepe bandage with just one pair ofhands. One person must initially hold the end of the bandage at the base of the penis as the bandage is folded at thescrotal-perineal border, while the other unrolls the bandage and wraps it around the scrotum.
Post operative care
Routine Antibiotic Coverage (Please see footnote on page 13.)
Amoxicillin 500mg tab. 3x for 7 days. and metronidazole 400mg tab. 3xfor 7 days (including the day before surgery, and the morning of surgery)
IMPORTANT NOTE: The first dose of both antibiotics must be given theprevious day, before surgery. Antibiotic treatment WITH BOTH DRUGS is thencontinued post operatively for 5 days, including the morning of surgery and continuingwhen the patient is fully awake and comfortable on the afternoon of the surgery day. Ifthere is an infection in spite of this treatment, it may require wound swabbing for cultureand sensitivity analysis, and then local antiseptic/antibiotic in addition to ongoingsystemic antibiotic treatment, or a change in systemic antibiotic.
Post-op. Analgesia (Please see cautionary note, just below!)
Diclofenac 50mg 3x for 5-7 days or ibuprofen 400mg 3x for 5-7 days.
NOTE: Caution is warranted concerning NSAIDs in patients who are hypertensive, diabetic, or old,
because of the potential risk of acute renal insufficiency that may not be dose-dependent, and in patients
with a history of dyspepsia.
Normal cautionary advice must of course be observed concerning all medications mentioned in thishandbook.
MF+ Patients are treated with ivermectine and albendazole
Microfilaria-positive patients are treated with a single dose of albdedazole(400 mg. p.o.) and ivermectin (Mectizan) 200 mg p.o. (In countries outside Africathat are not endemic for onchocersiasis, DEC (diethylcarbamazine) 6 mg p.o.is given as a single doseinstead of ivermectin, together with the albendazole.)
Hospital Admission
One week postoperatively, and then discharge home if the wound is nicelyclosed and dry or the patient lives close enough to return for any furtherbandage changes and other care that may be needed.
NOTE: Evaluations show that patients do excellently when they can be followed up for bandage changesby a conscientious hospital nurse who is expert in surgical wound care, with essentially no complications
following the procedure taught in these workshops. However, even the best surgeons have seen 20% postoperative infection rates in patients who returned to their villages after 2-3 days for wound care by localnurses who are neither equipped nor trained in this special bandaging technique, which is important toachieving good results after filaricele surgery.
Change of dressing
The bandage should not be touched if it is clean the day after surgery!
Only if the bandage is soaked on the day after surgery is it to be removedand changed.
If the bandage is soaked with blood, one should consider giving 10 mg.
Vitamin K i.m.
Sterile change of bandage on Day 3 and Day 5
It is important for a good result (avoiding secondary postoperativehemorrhage and infection) that the bandage change on both Day 3 andDay 5 be done using aseptic technique!
On Day 3, aseptic bandage change. Using sterile gloves, the surgeon orspecially trained nurse carefully disinfects the surgical wound and all ofthe scrotal area twice with Betadine or a similar disinfectant, using a newcompress/gauze for disinfecting the area the second time, just as at surgery.
Use the same bandaging procedure as at surgery, with sterile compresses
applied in the same way, followed by the elastic bandage applied in the
same way, and finally a supporting tape, all applied as taught during the
workshops and illustrated in Photo 14 a - e.
On Day 5, the patient should have a new aseptic bandage change.
On Day 7, aseptic technique should again be used. If the wound is dry andhealing nicely, elastic bandage can be used, but supportive taping is notusually needed because the patient's underwear will normally providesufficient support from Day 7 onward.
If the skin is nicely healing and dry along the whole length of the incision,the patient can resume normal bathing after Day 7 but should be sure toavoid using any local, herbal, or other preparations on the surgical wound.
On Day 14, if all is well, examination of the scrotum suffices.
Where absorbable sutures are used, the patient must be instructed not toremove them; suture knots will fall off after at most 6-8 weeks.
IMPORTANT NOTE: This close post-operative follow-up is essentialbecause any post-operative infection can very quickly become seriouslydangerous in this warm, moist part of the body, the more so in atropical climate under conditions where modern levels of personalhygiene may not be achievable.
If there is any sign of local infection on Day 3, bandages should bechanged daily until the incision heals nicely. Documentation of the stateof the surgical wound at each post-operative examination is veryimportant.
It is important to document all complications such as haemorrhage,haematoma, infection, recurrence etc.
Long term follow up
Long term follow-up for 3 - 5 years is ideal where possible, with a historytaken on the patient's situation, with a physical examination, and ifavailable also ultrasound.
After the wound heals and the patient is discharged from immediate post-operative follow-up at Day 14, follow-up monthly is suggested for twomonths, then at 6 months and one year, then only if they have any problem.
During these latter examinations, one is particularly interested in any signof recurrence and in how the patient is doing.
NOTE: Document any changes in financial self-sufficiency or other quality-of-life indicators at follow-upas compared with before the operation. Annex 5 provides a format for recording desirable long-termfollow-up data for monitoring and evaluating the project's outcomes.
The West African LF-Morbidity Project will attempt to follow up surgeons trained under the project, tocollect data on patients operated on by these surgeons. The hope is to document the effectiveness of theprotocol and the Project on a long-term basis, as well as to document the socio-economic benefitsaccruing to patients and their families. Participating surgeons who provide data on patients they haveoperated on will be recognized in any resulting scientific publications.
E. External monitoring and Evaluation
The West Africa LF Morbidity Project has done one evaluation and intendsto again have results of its surgical training efforts evaluated externally. It isenvisioned that this will involve visits by an external surgeon to a randomlyselected and significant proportion of patients operated on by those trainedunder the Project. The aim will be to ascertain surgery outcomes in terms of
infections and other complications, as well as long-term beneficial andnegative impact of operations. The main purpose of this effort will be tocollect evidence for the benefit (or otherwise) of the project's activities in ascientifically reliable manner.
Thambugala RL. Radical cure of filaricele of the tunica vaginalis; The technique of excision ofthe sac. 1971 British Journal of Surgery; Vol 58, No 7: 517-518.
Wright JE. Midline scrotal incision and simple dressing. 1966 Medical Journal of Australia;Vol. 2: 14-16.
Young HH. Radical cure of filaricele by excision of serous layer of the sac. 1940 Surgery,Gynecology and Obstetrics; 70: 807-812.
About pathogenesis and treatment of lymphoedema of genitalia and limbs
Dreyer G, Addiss D, Dreyer P, Noroes J. Basic Lymphoedema Management; Treatmentand Prevention of Problems Associated with Lymphatic Filariasis. 2002. HollisPublishing, USA; Available at: [email protected]
In French:
Dreyer G, Addiss D, Dreyer P, Noroes J. Guide pratique pour la prise en charge des casde lymphoedema; Traitment et prevention des affections liées à la filariose lymphatique.
2003. Hollis Publishing, USA; Available at: [email protected]
About ultrasound diagnosis and lymphangectasia
Amaral F, Dreyer G, Figueredo-Silva J, Noroes J, Cavalcanti A, Samico SF, Santo A,Coutinho A. Live adult worms detected by ultrasonography in human bancroftianfilariasis. Am J Trop Med Hyg 1994; 50:753-757.
Noroes J, Addiss D, Santos A, Medeiros Z, Coutinho A, Dreyer G. Ultrasonographicevidence of abnormal lymphatic vessels in young men with adult Wuchereria bancroftiinfection in the scrotal area. J Urology 1996; 156:409-412.
Dreyer G, Noroes J, Figueredo-Silva J. Elimination of lymphatic filariasis as a publichealth problem. New insights into the natural history and pathology of bancroftianfilariasis: implications for clinical management and filariasis control programs. Trans RoySoc Trop Med Hyg 2000; 94:594-596.
Dreyer G, Noroes J, Figueredo-Silva J, Piessens WF. Pathogenesis of lymphatic diseasein bancroftian filariasis: A clinical perspective. Parasitology Today 2000; 16:544-548.
About the twin approaches to LF elimination
Seim AR, Dreyer G, Addiss D. Controlling morbidity and interrupting transmission: twinpillars of lymphatic filariasis elimination. Revista da Sociedade Brasileira de MedicinaTropical 1999; 32:325-328.
The two most common urogenital manifestations of lymphatic filariasis develop in two ways, differentfor LF-hydrocele/filaricele on the one hand, and for lymphoedema and elephantiasis of the scrotum andpenis on the other hand, although the same underlying pathology is behind both conditions.
Underlying pathology of the lymph vessels
In post-puberty males, the W. bancrofti parasite has a predeliction for lymph vessels of the spermatic
cord. In lymph vessels with a living nest of parasites, a gradual and continuous dilatation of the lymph
vessel occurs as long as the adult worms are alive. The mechanism is as yet unknown but suspected to
entail endothelial proliferation in the lymph vessels stimulated by substances secreted from the parasite.
Dilatation stops when the adult worms die, leaving each lymph vessel irreversibly dilated as much as it
was when the last adult worm died or was surgically removed.
LF-hydrocele / filaricele
Ordinary, non-filarial hydrocele contains fluid that is an ultra-filtrate accumulated in the tunica
vaginalis. Such ultra-filtrate contains neither cells nor proteins to any significant degree.
LF-hydrocele/filaricele develops when lymphatic fluid from dilated scrotal lymphatics enters into the
tunical space, presumably as a result of rupture of thin-walled lymphatic vessels. Unlike in congenital,
non-filarial hydrocele, this is not a filtrate. It is lymph fluid, complete with lymphocytes, macrophages,
and a wide variety of proteins. Lymph is damaging to tissue when present in large amounts outside the
normal system of lymph capillaries and collecting vessels. Thus, testicular necrosis is seen in cases
where large, longstanding filaricele has included leakage of the fluid to the testis itself. It is to avoid
continuing leakage of lymph, with the risk of damage resulting to the testis and other scrotal tissues, that
the LF-hydrocele sac is resected during the procedure taught by the West African LF Morbidity Project.
Lymphoedema and elephantiasis of the scrotum
The basic pathology behind disease in LF-lymphoedema and LF-hydrocele / filaricele is dilatation of the
lymphatic vessels, lymphangectasia. Analogous to what occurs in veins when patients have varicose
veins, the fine lymphatic valves that normally assure one-way flow cannot meet at the middle when the
lymph vessel diameter increases too much; flow through the vessel becomes less efficient, and the area
drained by that lymph vessel becomes less well protected against bacteria and other pathogens that daily
cross the skin in small numbers, as a result of skin injuries (entry lesions), etc. The lymphatic
insufficiency caused by LF allows larger numbers of bacteria to persist and even develop under the skin
of the scrotum, a limb, or a female breast, leading to "acute attacks" with their characteristic
inflammation.
Inflammation during acute attacks damages lymphatic capillaries, leading to lymphoedema and furtherlymphatic insufficiency, with an even greater tendency towards new acute attacks. A vicious cycle isthus established that progresses towards fibrosis, thickening of the cutaneous tissues, and developmentof elephantiasis.
That vicious spiral can be broken by careful daily skin hygiene with soap, water, thorough rinsing andcareful drying, as well as protecting the skin against entry lesions. While the original lymph vesseldilatation is permanent, impressive clinical improvement and complete termination of diseaseprogression is seen with proper, daily self-care measures undertaken by LF-lymphoedema patients.
LOCAL ANESTHESIA FOR LF-HYDROCELE / FILARICELE
Diazepam 10 mg. i.v. should be given to all patients just before surgery.
In addition to calming the patient and alleviating the anxiety naturally associatedwith undergoing a surgical intervention, many patients experience a beneficialtendency towards a degree of amnesia for events experienced under a dose of thatsize. N.B. Pre-medication is important for a good result if local anesthesia is used.
Pethidine 50-100mg i.m., is given 5-15 minutes before surgery as a centrallyacting analgesic and improves the effectiveness of the local anesthetic. An initial50 mg. dose should be followed by an additional 25-50 mg. if the patient toleratesthe first dose well and shows signs of needing additional analgesia during theprocedure. Where Pethidine is not available, Tramadol 50 mg. can be injectedas an antiinflamatory analgesic.
Lidocaine hydrochloride 2% with adrenaline 1/1000 dilution; Normally 40ml. (Maximum Total Dose ≤ 400 mg. Xylocain)
NOTE: In some countries Xylocain is available pre-mixed with adrenaline. Where this is not the case, for each 20ml. of Xylocaine, placed in a small sterile bowl, one should add 1 ml of 1/1,000 concentration of adrenaline.
Adrenaline is an important component because it reduces bleeding.
Be sure to aspirate every time you insert the needle, before pushing on the plunger, to assure against injectingadrenaline intravascularly.
NOTE: As noted in the text itself, where available, bupivacaine (in a 1:1 dilution with normal saline or water adinj.) gives a strong and longer lasting effect, and thus requires less drug for the same local anesthesia time. It maytherefore also be less costly all told. However, in most of our settings, bupivacaine may not be available.
The following steps are employed when giving the lidocaine:
5 ml of the lidocaine is injected into and in front of the spermatic cord onboth sides (even for unilateral disease), proximally, fairly close to theinguinal canal.
10 ml is injected into the median raphae of the scrotum starting 2cm belowthe penis.
20 ml is injected subcutaneously around the filaricele, spreading out fromthe median raphae.
As and when necessary, the injections into the cord(s) are repeateddepending on the patient's response.
Be sure to use an adequate amount when topping up the localanaesthesia (e.g. 5 or preferably 10 ml.) !
ANNEX 3
RELEVANT ANATOMICAL HIGHLIGHTS
Please see illustration on the next page.
Arterial supply of the scrotal wall
Anterior scrotal arteries are branches of the internal pudendals and anastamose freely
with the posterior scrotal arteries at the apex of the scrotum.
Posterior scrotal arteries are branches of the perineal artery (inferior perineal branch)
given off at the base of the scrotum.
Collateral arterial supply to the testis
The artery to the vas and the cremasteric artery both supply collaterals to the testis.
Therefore, in any cases where accidental damage is caused to the testicular artery, thetestis can be left in place.
Venous drainage of the scrotal wall
Anterior scrotal veins accompany the anterior scrotal arteries, converge at the neck of
the scrotum and join the external pudendal vein.
Posterior scrotal veins run with their respective arteries from the apex to the base of
the scrotum and join the veins draining the posterior wall to become the perineal vein,
which joins the internal pudendal vein in the pelvis.
Lymphatic drainage of the scrotal wall and contents, and the penis
A set of lymph vessels accompanies each set of arteries and veins, as usual. Superficial
structures of the penis and scrotum are drained to a superficial group of inguinal nodes, while
deep penile structures, including the penile urethra, drain both to those superficial nodes and to
deep inguinal nodes. The testis drains directly to deep retroperitoneal, pelvic lumbar nodes.
It is this difference that explains why patients can have extreme lymphangectasia (dilatation) ofscrotal cord lymphatics in LF-hydrocele / fialricele, while the scrotal skin is normal in mostpatients. Patients who have lymphoedema of scrotal skin also have similar pathology affectingthe scrotal wall's drainage system. In those cases, damage to the scrotal wall's lymphatics hasled to repeated "acute attacks" and cycles of damage to lymph capillaries, with fibrosis that canprogress to elephantiasis, as in the legs. Such patients also have pathology of the separatetesticular drainage system that has led to their LF-hydrocele / filaricele.
Innervation of the scrotum and its contents
Innervation of the scrotum and its contents is by the posterior cutaneous nerve of the thigh and
the ilio-inguinal nerve (taking care of the dorsal and anterior aspects of the skin, respectively)
and by the genital branch of the genito-femoral nerve (innervates contents of the spermatic cord
and its contents including the testis and epididymis. The former nerve is on the ventral aspect of
the spermatic cord. The latter nerve lies within the spermatic cord and follows the artery.
This pattern of innervation has very practical implications for filaricele surgeryunder local anesthesia: Local anesthetic for the testis and epididymis mustespecially be placed in and in front of the spermatic cord at the start ofsurgery, and when topping-up may be needed.
ANATOMICAL HIGHLIGHTS continued
Illustration thanks to Prof. Joaquim Noroes
PATIENT CARE AND FOLLOW-UP FORM
Items to register for surgical care of LF filaricele patients§
2. Date of birth (age):
3.Marital status:
Characteristics of the filaricele
1. Duration of scrotal swelling:
3. Associated scrotal conditions:
1. Ultrasound findings:
2. Transillumination:
7. Estimated weight of the filaricele:
Other pathological conditions
1. Lymphoedema of limbs:
§ Page 5 of this Manual is intended as a summary overview-page of patient-notes, presentingkey pre-, per-, and post-operative information. Pages 5-7 can be photocopied and used as pre-operative patient charts. This form (pages 33-35) is intended for detailed documentation oftreatment the patient receives, and the outcomes of treatment. It can also be photocopied andused as a checklist of things to remember and be aware of. Some items from pages 5-7 aretherefore repeated here.
3. Laboratory tests: MF status: LF-antigen status:
Anaesthesia (for each category, write medication, dosage used, and time(s))
1. Pre-operative NSAID:
1. Date, start-time, stop-time, duration:
2.a. Surgical procedure(s) carried out:
2.b. Orchidectomy ?
(In situations where a testis was necrotic and in cases that turned out to be tumor testis, i.e. non-LF-related tumor)
2.c. Herniorrhaphy ?
(In situations where hernia turned out to be the diagnosis or co-existed with a filaricele)
3. Nature of filaricele fluid:
8. Volume of fluid:
3. Antifilarial TX:
5. Other medications:
Including, if given, any tetanus toxoid, infusions, Vitamin K, blood transfusion, iron supplementation
(if the patient is anaemic), etc.
Immediate (Day 0-5; specify when, and describe)
Late (Day 6 and beyond; specify when, and describe)
1. Infection (including any scrotal abscess):
1. Haemorrhage (secondary):
2. Wound breakdown:
3. Necrotic testis:
4. Fournieres gangrene:
Duration of hospitalization and follow-up
1. Duration of hospitalization:
2. Period of follow up:
3. Period before stitch removal: (In cases where resorbable sutures were not used)
Date(s), Surgeon's name and Signature
ANNEX 5 - Surgery Outcomes Data Registration Form (Draft) (1st of 2 pages)
1. Name of the Patient (family name, given name): .
2. Date of birth / _/ _/
3. Village/Town of residence: .
4. District : Region :
5. Duration of the disease : _ years
6. Diagnosis - initial : .
7. Ultrasound findings (if done) .
8. Date of hospitalisation : _/ _/ _/
9. Operative findings and technique used :.
10. Operation outcomes : .
11. Diagnosis - final : .
12. Date of departure from hospital : _/ _/ _/
13. Duration of hospitalisation _
14. Direct Cost of the actual surgery2 : / /
15. Post operative follow-up findings: .
Month 1 : .
Month 6 : .
Year 1 :.
Year ( _): .
Please ask the patient the questions printed on the next page as part of the follow-upassessment.
1 Number of the patient next to the initials for the hospital2 Include the cost of medications, the surgery itself, and the hospitalisation
ANNEX 5 - Surgery Outcomes Data Registration Form (2nd of 2 pages)
Four Socio-economic topics to ask the patient about
Patient name and residence (or number as noted at the top of this Annex):
Assessment time point:
6 months post-op 12 months post-op 18 months post-op 24 months post-op other (please specify)
Request to the patient:
I am going to ask you some questions.
Please indicate which statement best describes your own situation today.
16. General satisfaction with the surgical procedure:
1. I have no problems after the operation, and am glad that I had the surgery done2. I have some problems after the operation, but I am glad that I had the surgery done3. I do not know if I am glad that I had the surgery done or not4. I wish I had not had the surgery done (Please explain: _
17. Change in ability to work because of the surgery:
1. My ability to work is much better after the surgery than it was before2. My ability to work is a little better after the surgery than before, but not much3. My ability to work after the surgery is the same as it was before4. My ability to work is worse than it was before the surgery (Please explain: _
18. Change in economic situation after the surgery:
1. The surgery made my economic situation much better2. The surgery made my economic situation better than before, but not much3. The surgery made no difference to my economic situation4. The surgery made my economic situation worse (Please explain: _
19. Change in Family life after the surgery:
1. The surgery made my family life very much better than it was before2. The surgery made my family life better than before, but not much3. The surgery made no difference to my family life4. The surgery made my family life worse. (Please explain: _
NOTE: It is suggested that national LF elimination programmes and interested surgeons do morethorough prospective assessments of the socio-economic impact of LF-hydrocele disease and theimpact of its repair. The Euro-Qol scale and WHO's WHODAS scale seem among the well suited toolsthat can be useful when doing formal prospective studies. The LF Monitoring & Evaluation support groupin Atlanta (accessible through CDC (US Centers for Disease Control and Prevention) or The Task Forcefor Child Survival, both in Atlanta, USA) may be able to help in designing rigorous, prospective socio-economic impact studies. Such expertise may also be accessible through the African LF Support Centreat the Nogouchi Memorial Institute in Accra, Ghana.
RECIPIE FOR POTASIUM PERMANGANATE SOLUTION
Add 100mg of potassium permanganate crystals to 100ml. of water (equals 1 gram ofpotassium permangante crystals to 1 litre of water for large amounts).
Store the solution in an amber coloured bottle away from light.
The freshly prepared solution should be used within seven days.
This potassium permanganate solution is useful for skin disinfection and cleansing forall kinds of skin ulcers, bacterial and fungal skin infections, and for applying to gauzeor clean strips of white cotton cloth that can be soaked and inserted, even as wicks,into skin-folds or between toes, when treating advanced lymphoedema caused by LF(or other conditions).
ANNEX 7 EQUIPMENT LIST
Kit for Filaricele Surgery
Proposed by
Dr. Sunny Mante
as revised June 2007
Number pr. patient
3 (1 for each scrubbed person)
3 (Depends on nr. in op. room)
Non permeable/plastic apron
Surgical blades (e.g. size 10 or 15)
3 (Depends on nr. in op. room)
Gauze (e.g. 30cm. x 30 cm compresses)
50 compresses(30 compresses at surgery +20 for post op. skin disinfectionand dressings, Days 3, 5 and 7)
Vicryl/Maxon/Dexon 3-0 (2-0 can be used where 3-0 is unavailable)Gloves
6 pairs (double-set for each
(Note: Size is individual, usually 7 1/2 - 8)
person scrubbed; 2 surgeons, 1nurse)
4-5 rolls (1 at surgery; 1 atbandage change Days 3, 5, 7;plus any additional)
Plaster, 6 inch width
(Note: Sticky tape for bandaging,
depending on how many cases
not plaster as in "plaster cast")Infusion set
1 - In readiness
Surgical hand wash brushes
3 (1/person scrubbed-in)
& solutionsDiazepam10mg injection
Pethidine ad inj. 100mg
2% lidocaine with adrenaline
unilateral cases)
Amoxycillin capsules 500mg
3x /day for 7days
Metronidazole Capsules
3x /day for 7 days
400mgDiclofenac tablets 50mg
3 x /day for 5days
Vitamin K injection 10mg
For patients found bleeding first day post-
(In readiness only. Not routine.)
operatively.
Povidone iodine solution
250 ml. (including forbandage changes)
Dextrose saline infusion
500 ml. In readiness
Normal/saline infusion
500 ml. In readiness
Surgical blade handle
Small artery forceps
Big artery forceps
Small needle holder
Big needle holder
Metzembaum scissors
Gallipot / Bowl for sponges
Dissecting forceps - toothed
Dissecting forceps - non toothed 1
Sponge holding forceps
G. Dreyer – Photos 1, 4.
S. D. Mante - Pages 2 and 3; and photos nr. 2, 3, 5, 6, 8-11, 13, 14.
J. Noroes – Anatomy illustration, p. 32.
A. R. Seim – Photos 7, 12.
The West African LF Disability Project, for which this handbook is produced, was
supported in its initial pilot year by The Bill and Melinda Gates Foundation, Catholic
Medical Mission Board (CMMB), Interchurch Medical Assistance (I.M.A.), and HDI
(Health & Development International). The government of Norway has provided
funding for the Project in 2005 – 2007 through NORAD, and Johnson & Johnson has
kindly provided support for medical and surgical supplies used in the training
workshops, beginning in 2005.
Professor Gerusa Dreyer and Professor Joaquim Noroes have contributed massively tothis handbook in so many ways, and we extend our profound appreciation to them both.
Dr. Yao Sodahlon kindly provided the basis for the first page of Annex 5, while the LFMonitoring and Evaluation Group in Atlanta USA provided generous input that led theauthors to formulate the questions on the second page of Annex 5. We gratefullyacknowledge the patients who allowed themselves to be photographed, so theirexperiences can assist in the training of surgeons throughout West Africa. And wesimilarly acknowledge the surgeons who have provided valuable inputs through thequestions they asked, their discussion and comments, during the training workshops, the2006 evaluations in Burkina Faso, Ghana, and Togo, and the June 2007 workshop inSenegal. Also, we extend our warmest thanks to the many others who in multiple wayslarge and small have made this handbook and the entire West African LF MorbidityProject possible.
Production of this handbook's first edition (2005) in English was supported by fundingfrom The Bill and Melinda Gates Foundation, and HDI. The handbook was translatedinto French in 2006 with support from Johnson & Johnson.
Printed in Norway by HDI.
Source: http://hdi.no/pdfs/LF/lymphatic-filariasis-guide.pdf
GUIDELINES FOR THE ADMINISTRATION OF DRUGS THROUGH ENTERAL FEEDING TUBES 2nd Edition October 2003 NJWATT/PHARM/Review Date October 2004 Disclaimer Representations in this guide are believed to be true and accurate. The Primary Care Trusts, NHS Trusts, and their employees, or agents accept no liability for loss of any nature to persons, organisations, or institutions which may arise as a result of errors. Users of this guide are reminded that crushing medication or opening a capsule to aid administration results in unlicensed administration. It is recommended that unlicensed administration methods are authorised by the prescriber and documented in writing.
Vous souhaite de joyeuses Fêtes de fin d'année et tous ses voeux pour 2006 Journal édité par la commune de Meyrin en collaboration avec l'Association des Habitants de la Ville de Meyrin et le Cartel des sociétés meyrinoises Décembre 2005 No70 Meyrin Ensemble, Case postale 89, 1217 Meyrin 1 Gastronomie et sciencePour Noël, la gastrophysique dévoile ses cartes