Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Microsoft word - phd thesis 200611 final version.doc
A community-based factorial trial on Alzheimer's
disease.
Effects of expectancy, recruitment methods, co-
morbidity and drug use.
The Dementia Study in Northern Norway
Fred Andersen, MD
‘Navigare necesse est. Vivere non est necesse'
Pompeius 56 f. Kr
Contents
1. Acknowledgement
2. Funding
3. Summary
4. List of papers
5. Abbreviations
6. Introduction
6.1 Casuistry
7. Background
7.1 Definition
7.2 Literature on the topic
7.3 Aging and cognition
7.4 Alzheimer's disease
7.5 The epidemiology of AD
7.6 The histopathological findings in AD
7.7 Diagnosing AD
7.8 Screening of cognitive impairment and other functions in AD
7.9 Diagnostic criteria
7.10 Therapeutic options
7.11 Clinical trials, recruitment methods and external validity
7.12 Co-morbidities and drug treatment in Alzheimer individuals
8. Purposes of the study
9. Methods
9.1 Participants and recruitment methods
9.2 Two-by-two factorial design
9.3Outcomes
9.4 Organisation and management of the study
9.5 Validating study groups
9.6 Diagnosis and inclusion
9.7 Intervention
9.8 Testing and follow-up
10. Ethical considerations
10.1 Consent competence
10.2 About study design
10.3 Approvals
11. Data and statistics
11.1 Data recording
11.2 Statistics
12. Results
12.1 Recruitment methods and baseline characteristics
12.2 Cross-sectional comparison
12.3 Symptomatic treatment
13. Discussion
13.1 Recruitment methods and selection bias
13.2 Co-morbidities and current medication
13.3 Symptomatic treatment
13.4 Strengths and weaknesses
14. Conclusion
15. Reference list
16. Appendix
1. Acknowledgements
Beginning with an application to The Regional Committee for Medical Research Ethics
in Northern Norway in 2003 the Dementia Study in Northern Norway has been ongoing
for eight years. My wife and some times even I have considered the process to be similar
to a marathon: the end was always far ahead. First of all, I am thankful to her and the rest
of my family, who have endured my nearly endless focus on dementia for so many years.
My scientific supervisor Torgeir Engstad and his family have supported me and
participated in my struggle for funding, approvals and publications at each stage of the
study. The scientific advisory board consisting of Bjørn Straume, Matti Viitanen and Dag
Seeger Halvorsen has given me scientifical support. Thanks also to Tom Wilsgaard for
his statistical support. Special gratitude goes to Samuel Hykkerud and Kjell Sjøbrend
who have participated in examining and diagnosing a number of individuals with
cognitive impairment. Most of all I am grateful to the staff at the study centre, Kristin
Tverback, Merete Hjertø and Herdis Svendsen for daily administration, testing and
monitoring of patients included in the study. I want to express my gratitude to the
patients, nurses and general practitioners who participated and contributed to this study. I
also want to thank Inger Sperstad and the Clinical Research Centre at the University of
Tromsø for randomising patients and for data support; Per Baadnes at the Institute of
Community Medicine, University of Tromsø, for support with the screening procedure;
André Christoffer Andersen for the development and maintenance of our web site
http://dsnn.no and the staff at the pharmacy in Nordland Central Hospital for medical
distribution. Finally I would like to thank The Norwegian Women's Public Health
Association and our sponsors (see Funding) for necessary economic and practical
support. Among these the municipality of Steigen has played an important role as service
centre for the study and employer of the study staff. Last but not least, I want to pay
special gratitude to the Árran Lulesami Centre which has supported me with office
facilities and the peace to accomplish the final analyses of the study and write this thesis.
2. Funding
The Northern Norway Regional Health Authority; The National Centre of Rural Health at
The University of Tromsø; Health and Rehabilitation; The Directory of Health and Social
Welfare in Norway; the County Officer of Nordland and the Municipality of Steigen
constituted the funding group. Pfizer delivered donepezil and placebo, but had no
influence on the study design, data collection, analyses or publication.
3. Summary
BACKGROUND: Alzheimer's disease (AD) is an age-related progressive
neurodegenerative disorder causing irreversible cognitive impairment. The prevalence of
AD increases with age as does a number of other age-related physical illnesses. With an
exception for a genetic impact and risk factors such as cardiovascular and
cerebrovascular diseases no etiological factors have been identified. Usually, clinical
trials on AD have recruited participants from memory clinics, hospitals or nursing homes
using stringent inclusion criteria. These sampling methods could be at risk of selection
bias. Current therapy for AD includes non-pharmacological and pharmacological
symptomatic treatment. A number of studies on symptomatic treatment have reported
contradictory results. Drug treatment of co-morbidities in AD could reinforce cognitive
AIM OF THE STUDY: The main purpose of the present study was to examine the effects
of stimulation therapy on cognitive test performance in community dwellers 65 years of
age or older with a recent diagnosis of mild to moderate AD in Northern Norway. A
secondary purpose was to examine whether donepezil increased the effect of stimulation
therapy on cognition (Paper 3). During the study two additional purposes were included:
1. To compare baseline characteristics between participants included by two different
recruitment methods within the same geographical area (Paper 1)
2. To compare co-morbidities, current medical treatment and inappropriate medication
between participants with and without AD (Paper 2).
1. A cross-sectional comparison of baseline characteristics between participants
a. with AD included by two different recruitment methods (Paper 1)
b. with and without AD regarding co-morbidities, current drug treatment and
inappropriate medication (Paper 2)
2. A two-by-two factorial interventional study comparing stimulation therapy and
standard care to which a randomised, double-blinded, placebo-controlled trial with
donepezil was added (Paper 3)
PARTICIPANTS AND METHOD: The present study was population-based and
conducted at a community level
. One hundred and eighty-seven participants 65 years or
older with a recent diagnosis of AD were recruited in nine rural municipalities; 100 by
postal screening and 87 by general practitioners (GPs). In five municipalities the AD
participants received structured stimulation therapy, and in the remaining four standard
care. All participants were randomised in a double-blinded manner to donepezil or
placebo. In addition 200 cognitively healthy participants 65 years or older were randomly
selected by the screening program and included as control group. The clinical part of the
study lasted from January 2006 until June 2009.
RESULTS: AD participants recruited by screening were younger, more frequently men
and had a higher Mini-Mental-State-Examination (MMSE) 1 sum score as compared to
those recruited by GPs (Paper 1). In a cross-sectional comparison of co-morbidities and
current medical treatments between AD participant and cognitively healthy controls, a
significantly higher number of drugs were found in AD participants, despite no
significant differences in co-morbidities.Mean arterial blood pressure was significantly
reduced and the mean number of antihypertensive drugs significantly increased among
AD participants. The mean number of drugs and the frequency of inappropriate
medication increased in AD nursing home residents (Paper 2).
No time-point differences were found between AD participants receiving stimulation
therapy and those receiving standard care. Both groups retained cognitive test
performances during the one-year follow-up. Donepezil had no additional effect but
significantly more adverse reactions (95% CI 1.5 to 8.7 p=0.002) as compared to placebo.
A head-to-head comparison between stimulation therapy and donepezil did not reveal any
time-trend differences in cognitive test performance (Paper 3).
CONCLUSION: A community-based postal screening of cognitive function preceding
clinical examination may be a suitable recruitment strategy in studies of early-stage AD.
An increased number of drugs and inappropriate medication combined with reduced
mean arterial blood pressure could deteriorate cognitive test performances in AD
participants. AD participants retained cognitive test performance by receiving stimulation
therapy during one year, but no better than those receiving standard care. Adding
donepezil to these non-pharmacological treatment options did not improve outcome
ClinicalTrials.gov (Identifier: NCT00443014). EudraCT database (no; 2004-002613-
4. List of publications
Fred Andersen, Torgeir A Engstad, Bjørn Straume, Matti Viitanen, Dag S Halvorsen,
Samuel Hykkerud and Kjell Sjøbrend.
Recruitment methods in Alzheimer's disease research: general practice versus
population based screening by mail. BMC Med Res Methodol 2010; 10:25.
Fred Andersen, Bjørn Straume, Matti Viitanen, Dager Seeger Halvorsen, Torgeir
Co-morbidity and drug treatment in Alzheimer's disease. A cross sectional study of
participants in The Dementia Study in Northern Norway. Submitted BMC
Geriatrics.
Fred Andersen, Dag S. Halvorsen, Bjørn Straume, Matti Viitanen, Tom Wilsgaard,
Torgeir A Engstad
The effect of stimulation therapy and donepezil on cognitive function in Alzheimer's
disease. A community based RCT with a two-by-two factorial design. Submitted
Journal of the American Geriatrics Society.
5. Abbreviations
Alzheimer's disease
ADAS-Cog
Alzheimer's disease Assessment Scale, cognitive (Scale 0―
70,
increasing disability with increasing score)
Activities of daily living
Barthel Index (Scale 0―
20, better function with increasing
Cholinesterase inhibitor
Cerebrospinal fluid
DSM-IV-TR
Statistical Manual of Mental Disorders fourth edition
Early-onset Alzheimer's disease
Good clinical practice
Global Deterioration Scale
General Practitioner
International classification of diseases 10th Revision
Informant Questionnaire―
Cognitive Decline in the Elderly
Late onset Alzheimer's disease
Montgomery and Aasberg Depression Rating (Scale 0―
60
increasing depression by increasing number)
Mild cognitive impairment
Mini-Mental State Examination (Scale 0―
30, better function
with increasing score)
NeuroPsychiatric Inventory (Scale 0―
144, increasing number
of psychiatric symptoms by increasing number)
NINCDS-ADRDA National Institute of Neurological Disorders and Stroke-
Alzheimer Disease's and Related Disorders
Odds Ratio
Positron emission tomography
Randomised clinical trial
Subjective cognitive impairment
Vascular dementia
6. Introduction
6.1 Casuistry
In 1994, the Department of Psychiatry at the County Hospital in Bodø was invited to
participate in a multicentre international Phase III clinical trial on AD. One of my
patients with a recent diagnosis of AD was included in the study and allocated to active
drug or placebo treatment in a double-blinded randomised manner. This patient was
followed carefully every second week for four months. During this period, the patient's
cognitive function, quality of life and activity of daily living (ADL) improved, both
subjectively and according to observations and formal testing. Patient and family were
satisfied with the treatment. After four months the randomisation code was broken. My
patient was a placebo users. I was astonished and the patient were disappointed. How
could the cognitive and executive functions improve by placebo treatment?
The question remained in my consciousness for years. Nine years later the first protocol
of the Dementia Study in Northern Norway was written.
7. Background
7.1 Definition of dementia
Dementia is an acquired organic mental syndrome followed by general impairment of
cognitive abilities such as memory, judgement and abstract thinking as well as
personality changes. Dementia is irreversible and progressive and does not include
functional mental disorders such as delirium or temporary impaired consciousness2.
The present study focus on AD, a syndrome first described by the German psychiatrist
Alois Alzheimer in 19063;4.
7.2 Literature on the topic
The main focus of the present study is the effect of stimulation therapy on cognitive test
performance in an early-stage AD, to which donepezil treatment is added. Stimulation
therapy comprises reality orientation, physical exercise, cognitive stimulation,
reminiscence activities and various sophisticated sensory stimulations. Pharmacological
treatment mainly involves cholinesterase inhibitors (ChEIs) and memantine.
Scandinavian research centres have participated in interventional AD studies with ChEIs
organised as multicentre RCTs 5-7. Only a few population-based screening programs
aimed to recruit AD participants in clinical trials have been conducted8;9. A head-to-head
comparison between stimulation therapy and ChEIs examining the effects on cognition in
AD has been requested by the scientific community10 but has to my knowledge not been
The literature listed below represents a brief review of the available knowledge of the
effect of stimulation therapy and drug treatment on AD at the onset of the present study 11
and a sample of recently published studies on the topic. A brief review of new evidence
of the impact of placebos in clinical trials is added. A complete and updated reference list
Stimulation therapy
When the present study was initiated, three review papers of the effect of stimulation
therapy on AD were identified in PubMed.
1. In 2004 Heyn et al. published a meta-analysis of the effect of exercise training on
elderly individuals with cognitive impairment and dementia. Published articles
and non-published manuscripts from 1970 to 2003 were identified and 30 studies
(2020 participants) were included. Heyn et al concluded that "physical training
increased fitness, physical function, cognitive function, and positive behaviour in
people with dementia and related disorders"12.
2. In 2003 a review by Clare et al evaluated the impact of cognitive training and
cognitive rehabilitation on early-stage AD. Records from MEDLINE, EMBASE,
CINAHL, PsycINFO and many other databases, waere searched in April 2003.
Six studies comprising cognitive training with a RCT design were included. Clare
et al concluded that the results did not provide strong support for the use of
cognitive training for early-stage AD or VaD. However, only a few studies were
available, hampered with methodological limitations. No conclusion could be
drawn about cognitive rehabilitation due to a complete absence of RCTs on the
3. In 2003 Luijpen et al published a review of studies examining the effects of non-
pharmacological stimulation on cognition, affective behaviour and the
sleep―wake rhythm of cognitively impaired and demented elderly. The
stimulation therapy comprised bright light, physical activity and tactile
stimulation. Luijpen et al concluded that all three types of stimulation appeared to
increase cognitive function14.
Several clinical trials examining the effect of stimulation therapy on AD have been
reported during the last 15 years15-19. In some of them stimulation therapy was added
to ChEI treatment20-22. The most important recent trials and review papers on the
topic are listed below.
1. In 2003 Spector et al published a well-designed single-blinded randomised
multi-centre controlled trial with stimulation therapy for people with
dementia. The study included 201 individuals with dementia. The main
outcome measures were changes in cognitive function and quality of life as
measured by MMSE, ADAS-Cog and the Quality of life – AD scale. The
authors reported significant improvement in cognition and quality of life in
the intervention group23.
2. In 2006 Graff et al published a single-blinded randomised controlled trial to
assess the effectiveness of community-based occupational therapy for the
ADL functions of patients with dementia and the sense of competence of their
caregivers. The study included 135 participants with mild to moderate
dementia. Ten sessions with occupational therapy during 5 weeks were
provided, and the results were evaluated after 6 weeks and after 3 months. The
authors concluded that occupational therapy improved activities of daily
living of the patients and reduced the burden of the caregiver16.
3. In 2010 Olazaran et al published a systematic review and meta-analysis of the
entire field of evidence-based knowledge of non-pharmacological therapy to
treat AD. They concluded that non-pharmacological therapy was a useful and
cost-effective approach to improve outcomes in AD and related disorders.24
4. Yamaguchi et al (review 2010) focused on how therapists should
communicate with patients and caregivers and offered some proposals for
non-pharmacological intervention in suitable supportive psychosocial context
to obtain optimal results25.
5. In two recent review papers on stimulation therapy in AD, Ballard et al.
(March 2011) and Andrade et al. (March 2009) both emphasise the positive
impact of cognitive training, occupational activities and physical exercise on
cognition and activities of daily living in patients with early-stage AD26;27
ChEI treatment
Early loss of basal forebrain cholinergic neurotransmission is a biochemical hallmark of
AD28;29. Since the early 1990s several drugs with cholinesterase-inhibiting effects have
been developed and tested in clinical trials, including symptomatic treatment of mild to
moderate AD. However, the clinical effects, relevance and the cost-effectiveness of these
drugs have been questioned. The literature listed below reflects some of the scientific
uncertainty related to the effect of ChEI treatment of AD at the time when this study
began, in addition to recently published papers on the topic. A number of review papers
on ChEIs have been identified and all of them concluded that ChEIs have a small to
modest beneficial effect on cognition. One of the review papers included clinical
recommendations30-36. Four of the review papers are summarised below.
1. Trinh et al reviewed papers with ChEI-treated AD participants from 1966 to
December 2001. Twenty-nine parallel groups or crossover double-blinded RCTs
of outpatients treated for at least four weeks were included. They concluded that
ChEIs had modest beneficial effects on neuropsychiatric and functional outcomes
for patients with AD. No conclusion could be drawn as to institutionalisation or
quality of life33.
2. A Cochrane review by Birk et al 2002 included 16 trials of 12, 24 or 52 weeks
involving 4365 participants treated with donepezil 5 mg or 10 mg. A statistically
significant effect on cognition measured by ADAS-Cog was reported after 52
weeks of treatment. Some improvement was found in global clinical state as rated
by an independent clinician. Benefits of treatment were also seen in measures of
activities of daily living and behaviour. Significantly more adverse reactions were
found in participants on 10 mg donepezil compared to placebo30.
3. Raina et al.(2008) conducted a review of 59 unique studies from 1986 through
2006 that evaluated the effectiveness of ChEI and memantine in achieving
clinically relevant improvements, primarily in cognition, global function,
behaviour and quality of life, in patients with dementia. Both ChEI and
memantine had consistent but small effects in the domains of cognition and global
assessment (the clinical-based impression of changes with caregiver input). Fewer
consistencies were found for behaviour and quality of life. Most studies had short
duration. The authors concluded that "treatment of dementia with ChEI or
memantine can result in statistically significant but clinically marginal
improvement of cognition or global assessment"32.
4. A clinical practice guideline for current treatment of AD in the US was published
by Qaseem et al. in March 2008. The guideline recommended that clinicians base
the decision to initiate a trial of therapy with ChEI or memantine on
individualised assessment taking tolerability, adverse effect profile, ease of use
and medical cost into consideration31.
One of the classic trials examining donepezil for AD treatment was published by Rogers
et al. in 199837. They highlighted cognitive deterioration as an inherent trajectory of AD
and showed that cognitive performance could be maintained by nearly one year of
donepezil treatment. However, this randomised, placebo-controlled and blinded part of
trial was run for only three months. At that time the study was opened and the AD
participants in both groups were treated only with donepezil without a control group.
However, the reference to the inherent AD trajectory as the background for evaluating the
effects of symptomatic treatment with donepezil makes this study one of the most
important on the topic. Stabilising cognitive performance has for a long time been
identified as an important treatment outcome in AD research38.
Due to ethical considerations few placebo-controlled trials with ChEIs for AD treatment
have been conducted during the last 10 years
Several RCTs with disease-modifying drugs, including the phenserine enantiomer (a
derivate of physostigmine) have been published7. The results for phenserine enantiomer
were not clinically significant as measured by ADAS-cog, the clinician's impression of
change and the caregivers´ input29. The results of other RCTs of disease-modifying drugs
for AD have so far been disappointing29.
A placebo was originally defined as a dummy medical treatment but has recently been
described as any dummy treatment administered to the control group in a controlled
clinical trial2. The placebo effect is defined as the favourable impact of placebo (with a
biologically inert substance or shame intervention) on the course of a disease state. The
placebo effect is reinforced by classical Pavlovian conditioning, firm diagnosis, clinical
testing, novel therapeutic procedures, verbal suggestion of a beneficial outcome and a
positive doctor-patient relationship39-41. The placebo effect in clinical trials has gained
more attention in recent years. Several studies have described the placebo effect as a
complex interaction between the psychosocial context of the intervention and the
expectation of a clinical benefit42;43. In brain-activating rehabilitation the treatment is
recommended to be implemented in a favourable psychosocial context utilising the
impact of expectation and verbal suggestion25. The impact of the placebo effect in clinical
trials has probably been underestimated43. In a recent review Fournier et al (2011) found
that a true effect of antidepressant drugs was nonexistent or negligible compared to
placebo amongst depressed patients with mild, moderate and even severe baseline
symptoms, whereas the true antidepressant drug effect was large for patients with very
severe depressive symptoms 44. The first evidence of a biochemical mechanism
underlying the placebo effect, was demonstrated by Levine et al. in 1978. They found
that the placebo analgesia effect could be blocked by naloxone. This observation
suggested that a placebo could induce the release of endogenous opioids. In recent years
several studies using functional magnetic resonance imaging techniques have visualised
the role of placebos in releasing endogenous neurotransmitters in the brain40;43;45
Few studies have focused on the placebo effect in AD. Benedetti et al. have postulated
that the placebo mechanism depends upon preserved frontal lobe function. They
evaluated lidocaine pain relief in AD individuals compared to controls. The placebo
effect in AD participants with mild cognitive impairment (MMSE 24 ± 1.22) was
preserved but it was significantly reduced in patients with moderate to severe AD
(MMSE 15.6 ± 1.9) compared to controls. A reduced placebo effect was found to be
correlated to reduced frontal executive function as measured by the Frontal Assessment
7.3 Aging and cognition
Memory complaints amongst the elderly are usually interpreted as a clinically normal
age-related condition. However, approximately half of elderly subjects have no cognitive
complaints and objectively normal neuropsychiatric performance. The prevalence of age-
related self-reported cognitive disturbances constituted 20% in one study and varied
between 25% and 56% in three other studies of individuals 65 years of age or older47;48.
Cognitive complains in the elderly are also associated with co-morbidities such as
depression and pain48;49.
Age-related memory impairment and mild cognitive impairment (MCI)
MCI50 is supposed to be a continuum or an intermediary stage of cognitive disability
between age-related memory impairment and early dementia stages, and it could be
reversible51. The most commonly used criteria define MCI as a condition of subjective
memory complaints, abnormal memory for age, normal executive functions and no
dementia52-54. Cognitive impairment should be present without any interaction with ADL.
Depending on the diagnostic tools and criteria55, the incidence rate of MCI individuals ≥
65 years of age progressing to dementia range from 1 to 25% in one review paper56, from
10 to 15% in another57 and was 5.4% in one single cohort study58. In the cognitively
healthy population ≥ 65 years, the incidence rate of dementia is 2%57-59. Amnestic MCI is
a pre-clinical phase of AD lasting several years before the diagnostic criteria of AD are
fulfilled48;60. According to Reisberg et al. (2008) individuals with subjective cognitive
impairment (SCI) and normal MMSE are at a significantly higher risk of cognitive
decline compared to individuals with no subjective cognitive impairment (NCI) and
normal cognition. During a mean follow-up of seven year, 54.2% (n=90) of the SCI
group revealed cognitive deterioration compared to 14.9% (n=7) of the NCI group
(p<0.001)61. In the SCI group 71 of 90 individuals declined to MCI and 19 to dementia.
7.4 Alzheimer's disease
AD represents 65―70% of all dementia diagnoses, 90% of which occurs in individuals
who are 65 years of age or older. The cardinal initial symptom of AD is impaired
episodic memory and an inability to retain recently acquired information. With disease
progression impairment of other cognitive domains, such as visuospatial, verbal and
executive functions and semantic memory, occurs. Changes of social behaviour and
personality are common, especially in advanced disease stage62. Increasing cognitive
disability gradually influence ADL63. Delusions and psychotic behaviour are not typically
initial symptoms but can occur at any time during the disease course62. The natural
cognitive deterioration is characterised by a yearly 2 – 3-point decrease in MMSE sum
score corresponding to an increase of 6 – 12 points in Alzheimer's disease Assessment
Scale, cognitive (ADAS-Cog)64 score65-67.
7.5 Epidemiology of AD
The incidence and prevalence of AD increase steeply with ageing and depend strongly on
the diagnostic criteria68-70. The overall prevalence ranges from 5.4 to 10.3% in a
population ≥ 65 years3;71. The prevalence of AD is 3% in the 65―74 year age group and
increases to 47% in those above 85 years. No significant differences amongst countries
have been reported72-74, although differences amongst ethnical groups are found75;76.
Increased longevity and a steadily increasing number of individuals reaching the age of
retirement in developed countries in the years to come will reinforce the impact of AD on
public health services and may represent an unsustainable economic burden on
societies3;72;73;77-81.
AD is a heterogeneous syndrome. Both genetic and environmental factors have an
etiological impact82. The genetically attributable risk of AD is postulated to be 70%27.
Early-onset AD (EOAD) (<65 years of age) accounts for less than 10% of all AD
individuls83 84. Late-onset AD (LOAD) is a sporadic condition with an inherent but not
genetically dominant disposition85;86. Individuals who are homozygous for the APOE ε4
allele are at an increased risk of LOAD85 and having a close relative with AD increases
the risk of AD. Known environmental risk factors include negative lifestyle habits (i.e.
excess weight, inactivity, smoking) and co-morbidities such as metabolic syndrome,
hypertension in midlife and cardiovascular and cerebrovascular diseases87;88
Level of education may modify the deterioration of AD89;90, providing support to the
"cognitive reserve" model65. A meta-analysis in 2006 confirmed that low education may
be a risk factor for dementia91.
Insufficient nutrition, especially reduced consumption of vitamin B12 and folic acid, has
been associated with AD, but convincing causal interaction is still lacking92, and the
deficiency stages can be secondary.
7.6 The histopathological findings in AD
The AD brain shows medial temporal lobe atrophy especially in the entorhinal cortex and
hippocampus (in the floor of the inferior horn of the lateral ventricle) and in parts of the
frontal and parietal lobes93. The histopathological hallmarks of AD are senile plaques and
neurofibrillary tangles in the cortex27.
7.7 Diagnosing AD
The diagnosis of AD in general practice is based on a careful medical history usually
extended by a caregiver; cognitive and neuropsychiatric tests; clinical examination and
neuroimaging. In memory clinics, more advanced diagnostic tools and procedures are
provided. Typical findings are problems in episodic memory, visuospatial tasks, verbal
and executive functions. The diagnosis is supported with hippocampal atrophy in
magnetic resonance imaging (MRI), changes in biomarkers in cerebrospinal fluid (CSF)
such as elevated total tau and phosphorylated tau protein, low level of β-amyloid42 in
cerebrospinal fluid (CSF)94, temporoparietal hypoperfusion in Single Photon Emission
Computer Tomography (SPECT), decreased glucose metabolism in tempo-parietal lobes
and increased amyloid deposits in frontal lobes as assessed with positron emission
tomography (PET)95.
7.8 Screening of cognitive impairment and other functions in AD
MMSE is the test most widely used to screen and monitor changes in cognitive function.
The cognitive domains assessed are memory, language, abstraction, visouspatial and
executive functions. The test favours individuals with higher education96. In Norway the
clock drawing test97 is also used routinely to assess executive and visuospatial functions.
It is validated and easy to use.
In AD drug trials, ADAS-Cog is the most widely applied cognitive test to follow disease
progression98. ADAS-Cog covers the typically deteriorated cognitive domains in AD, and
frequent repetitions do not tend to improve the results. It is validated and translated into
A number of additional cognitive, neuropsychiatric, ADL and depression tests and semi-
structured questionnaires have been developed.
Various population-based screening tools of cognitive impairment and AD have been
evaluated. Caregiver-based telephone interviews have good agreement with the
assessment by general practitioners8. A two-step population-based screening of cognitive
impairment by a postal questionnaire and a subsequent telephone interview was
developed by van Uffelen et al. Individuals with probable MCI as diagnosed by screening
were invited to a face-to-face clinical assessment. Screening compared to clinical
assessment had a 41% agreement in diagnosing MCI 99. In general, self-administered
postal questionnaires have several advantages over face-to-face assessment. They are
cheap and suitable in surveys, requiring no training and provide a high response rate in
elderly people. In England and Wales a postal screening approach for morbidity in the
elderly has been advocated100.
7.9 Diagnostic criteria
Three sets of diagnostic criteria based on clinical examination are most frequently used in
clinical trials. Two of them have been developed and revised over years (ICD-9 → ICD-
10, DSM-III → DSM-III-R→DSM-IV) and have gradually been approached to one
According to ICD-10101;102 dementia in LOAD is a chronic neurologic disorder involving
several cognitive domains in individuals ≥ 65 years. A LOAD diagnosis presupposes
impaired memory (especially short-term and episodic memory) and disturbances in one
or more executive functions such as abstracting, judgment and problem solving.
Disturbances in language (especially semantic memory) and visuospatial functions
strengthen the diagnosis. The observed cognitive deficits should interfere with social or
occupational activities and represent a significant decline from a previous level of
functioning. Decline in cognitive function should be steady and progressive and not due
to delirium, depression, endocrine disorders, nutrition deficiencies, infectious diseases or
other dysfunctions in the central nervous system. Decline in cognitive function should
have lasted for at least six months and consciousness disturbances should be excluded69.
DSM-IV TR
According to the Statistical manual of mental disorders, fourth addition (DSM-IV-TR)103,
a dementia diagnosis of AD requires both memory deficits (especially impaired ability to
learn new information and recall previously learned information) and deficits in at least
one additional cognitive domain (aphasia, apraxia, agnosia, and/or executive functions),
both interfering with social functioning and ADL94. The course is characterised by
gradual onset and continuing cognitive decline. Delirium, depression and other causes of
dementia or cognitive impairment should be excluded. Normal consciousness is required.
The National Institute of Neurological Disorders and Stroke-Alzheimer Disease and
Related Disorders (NINCDS-ADRDA)103 criteria for probable AD require a clinically
and neuropsychologically established diagnosis of dementia including deficits in at least
two cognitive domains: 1. Memory impairment; i. e. the loss of learning ability and/or the
ability to recall previously learned information. 2. One or more of the following
disturbances: apraxia, aphasia, agnosia and executive functions. Loss of function should
be a substantial decline from previous abilities and should influence ADL. The
disturbances should begin slowly and gradually become more severe. Delirium should be
excluded. The criteria include normal motor, sensory, and coordination functions at an
early disease stage and the absence of focal neurologic symptoms. Laboratory tests and
cerebral computed tomography (CT) should exclude other possible causes of cognitive
impairment before the diagnosis of Alzheimer's disease can be made with confidence.
These criteria also include neuropsychological tests to provide confirmatory evidence of
Although no gold standard diagnostic criteria of AD exist, Ballard et al. emphasise that
the diagnostic criteria and procedures mentioned above have a sensitivity and specificity
> 80 % for discriminating Alzheimer's disease and healthy cognition27. Dubois et al
emphasise that DSM-IV-TR and NINCDS–ADRDA criteria have been validated against
neuropathological findings with diagnostic accuracy ranging from 65 to 96%. In a recent
study from Lund, Sweden, 84% of patients with a clinical AD diagnosis had a significant
Alzheimer neuropathological component104. The specificity of the present diagnostic
criteria against other dementias is only 23–88%94. New diagnostic options such as CSF
biomarkers and functional PET have increased accuracy and are currently closest to a
gold standard diagnostic tool94. However, the sensitivity and specificity of the current
routinely available diagnostic tools, relying on cognitive tests and medical history, are
still insufficient. In combination with various diagnostic criteria, this insufficiency could
influence the calculation of both prevalence and incidence rate69;70 and makes the
calculation of predictive values and the accuracy of current tests less certain.
7.10 Therapeutic options
As long as no causal treatment of AD exists, therapies must concentrate on prevention
and symptomatic treatment105-107 by means of stimulation with and without
pharmacological treatment or pharmacological treatment alone. The development of
efficient disease-modifying drugs has until recently failed27. The unsuccessful approach
focused on a causal therapy has demonstrated a probably insufficient basic understanding
of AD pathogenesis29. AD is a multifactor disorder108. A single drug acting against a
single target linked to a single pathogenic pathway or disease is not likely to be found29.
At the moment, intervention against risk factors and symptomatic treatment is the only
therapeutic option105.
Intervention on risk factors in AD
With the growing prevalence of AD, sustainable intervention methods against known risk
factors are important. Health conditions and lifestyle are risk factors associated with AD
and could be the most reasonable targets of an optimal preventive strategy87;88. Lifestyle
habits including nutrition and physical activities may modify many risk factors109.
Increasing evidence suggests that an active lifestyle among the elderly including social,
mental, and physical engagement may prevent AD. The strongest evidence is found for
increasing an individual's level of physical activity, followed by the cessation of smoking
Treating hypertension in midlife may reduce the risk of dementia112. Interventions and
medical treatment of cardiovascular risk factors in AD are supposed to delay AD
progression and improve prognosis. So far treating cardiovascular risk factors and
metabolic syndrome have not influenced cognitive decline or AD progression113. There is
conflicting evidence about the preventive effect of antihypertensive treatment27;113.
However, physical activities and interventions to promote a healthy lifestyle will
probably reduce the incidence of several AD risk factors27 and are the most promising
AD-modifying efforts114.
Symptomatic treatment (non-pharmacological and pharmacological therapy)
As AD is a progressive neurodegenerative disease, any considerable improvement of
cognition is not likely. The best obtainable result of symptomatic treatment would be
postponing an inevitable cognitive deterioration. This is an esteemed goal for
symptomatic treatment, and verified by a number of clinical trials on the topic37;115;115;116.
How sustainable this postponement of cognitive decline could be is still unknown, but
any postponement of cognitive deterioration will be valuable both for the patients and the
Stimulation therapy
Various non-pharmacological interventions for individuals with dementia are available,
including physical exercise, occupational therapy, cognitive rehabilitation and social
stimulation.12;13. A number of small interventional studies have been conducted in recent
years and most of them report positive effects of stimulation therapy compared to control
treatment10;15;23;117;118. A meta-analysis from 2004 on exercise training in elderly with
dementia reported improved fitness, physical and cognitive function, and positive
behaviour12. A new systematic review performed by Olazaran et al. (2010)24 examined
179 RCTs on stimulation therapy. According to the criteria of Oxford University's Centre
for Evidence-Based Medicine, 13 high-quality trials were found of which seven (54%)
reported positive results; 113 of 166 (68%) low-quality trials were positive. In spite of
these results, Olazaran et al. concluded in this way: "Non-pharmacological treatment
emerges as a useful, versatile and potentially cost-effective approach to improve
outcomes and quality of life in AD and related disorders for both persons with dementia
and caregivers". A third systematic review (2008) dealing with mild to moderate AD,
provided practical recommendations on non-pharmacological and pharmacological
interventions. One conclusion was that there is good evidence that individualised exercise
programs have an impact on functional performance119. Furthermore, Lujipen et al
concluded in a review that improvement in cognition and affective behaviour by bright
light, physical activity and tactile stimulation and by cholinesterase inhibitors had similar
effect sizes. All three types of stimulation appeared to increase cognitive function14.
Drug treatment (ChEI and memantine)
During the last 15 years, the AD neuropathological focus has been on insufficient
neurotransmission in affected brain areas, initially on cholinergic and glutamate synapses
in particular. Since the early 1990s several drugs with ChEI effects have been developed
and tested. The external validity of these early phase III RCTs on ChEI was hampered by
short duration and by the restrictive subject selection criteria120 which would have
excluded 90% of eligible community-dwelling AD individuals121. One large community-
based industry-independent donepezil study included 595 AD individuals and lasted for
more than one year (the AD2000 trial)122. An increase in mean MMSE sum score of 0.8
points in the donepezil group over placebo was found (p<0.001) whereas other outcomes
were insignificant32. The main conclusion from meta-analyses of cholinesterase inhibitors
is that ChEIs (donepezil, rivastigmine and galantamine) have a modest beneficial effect
on cognition and a questionable clinical efficacy30;36;123;124. In Norway, three
cholinesterase inhibitors have received legal marketing for symptomatic treatment of
mild to moderate AD. A guideline for dementia treatment in general practice
recommends that clinicians should base their decision to prescribe ChEI or memantine on
individualised assessment, taking tolerability, adverse effect profile, ease of use and
medical cost into consideration31.
Therapy combining non-pharmacological and pharmacological treatment
The effect of stimulation therapy in patients treated with ChEIs has been evaluated in
several studies19;20;22;125. In these studies, AD individuals were randomised to stimulation
therapy combined with ChEI or ChEI only (controls). These studies were open or single-
blinded and reported significant effects of stimulation therapy added to ChEI. No studies
have so far compared ChEI with stimulation therapy in a head-to-head clinical trial10.
7.11 Clinical trials, recruitment methods and external validity
Most clinical trials on AD using stringent inclusion criteria have recruited participants
from memory clinics, hospitals or nursing homes126. In contrast, some trials have
recruited AD participants by advertising in newspapers. These methods provide samples
with different characteristics. Hence, the validity of these studies is questionable and the
results from some of these studies could hardly be generalised127.
7.12 Co-morbidities and drug treatments in AD individuals
As a consequence of the increased number and severity of co-morbidities in AD
individuals128-130 necessary medical treatment could be more extensive compared to
cognitively healthy individuals. Neuropsychiatric symptoms in AD are common,
especially in advanced disease stages. The symptoms could require treatment with
psychotropic drugs. Increasing the number of drugs administered, especially psychotropic
drugs and drugs with anticholinergic activity, is prone to influence cognition
negatively131;132.
Co-morbidity and Alzheimer's disease
AD is associated with metabolic syndrome133, hypertension in midlife134 and increased
cardio- and cerebrovascular disease burden88. Ischemic disease affects 60% to 90% of
AD individuals, with major cerebral infarctions representing one-third of vascular lesions
in autopsy cases108. Arteriosclerosis and reduced cerebral perfusion reinforce cognitive
impairment in AD individuals in an additive or synergistic manner82;135-138. The Cache
study has reported a more rapid AD progression in patients with atrial fibrillation,
hypertension or coronary heart disease139. Deschaintre et al. have reported similar
results140. The number of co-morbid medical illnesses in AD increases with disease
severity128;141. In addition, AD individuals have more serious medical co-morbidities than
comparable persons without cognitive impairment129. Dementia in elderly people is
associated with low blood pressure142, but this could be a confounder, as low blood
pressure by itself may predict death143. Pneumonia, febrile episodes, and eating problems
are frequent complications in patients with advanced dementia, and these complications
are associated with high 6-month mortality rates144.
Inappropriate drugs
Inappropriate medical treatment in the elderly has been an increasing concern in geriatric
practice for years. Few studies have specifically addressed inappropriate treatment in
AD145;146. Increasing the number of drugs increases the risk of adverse reactions and
inappropriate medication131;146-148. Efforts have been made to define suitable guidelines
and treatment criteria in the elderly. Beers´ criteria for inappropriate drugs were the first
guidelines in the field. The criteria defined inappropriate medications in geriatric practice
according to drugs licensed in the USA149 but did not address drug interactions or
inappropriateness with or without specific diagnoses150;151. Rognstad et al. have through a
Delphi process compiled a list of 36 explicit criteria for drugs clinically relevant for
general practice in Norway, and considered potentially inappropriateness for elderly
people (≥ 70 years). This list does not address specific diagnoses either151. The STOPP
criteria define inappropriate drugs according to drug interactions and common geriatric
disorders152 However, Barnett et al. question the validity of the full list of potentially
inappropriate drugs in older people because no significant impact on mortality has been
More serious medical co-morbidities in AD individual may call for more extensive
medical treatment compared to cognitively healthy persons. As a result, AD individuals
have an increased risk of adverse drug reactions and inappropriate drug treatment147;148
8. Purpose of the study
The main aim of this study was to examine the impact of stimulation therapy on cognitive
performance in individuals ≥ 65 years old with a recent diagnosis of mild or moderate
A secondary aim was to examine whether donepezil had an additional effect on cognitive
performance when combined with stimulation therapy.
During the progression of the trial, two additional study aims were adopted to compare:
1. baseline characteristics in AD individuals recruited by two different methods from the
2. the prevalence of co-morbidity and drug burden between AD individuals and
cognitively healthy controls.
9. Methods
9.1 Participants and recruitment methods
In clinical practice
Two hundred participants with a recent diagnosis of AD were expected to be examined
and included in the study by general practitioners in nine rural municipalities in Northern
Norway between January 2006 and December 2007. However, during 2006 only 27 AD
participants were included in the study. By then it was obvious that a presupposed sample
size of 200 participants could not be reached by recruitment in general practice
The participating municipalities were selected from municipalities employing competent
and professional health providers in rural Northern Norway. The general practitioners
were well prepared for scientific studies and engaged in evidence-based medicine.
However, as it came to examining and diagnosing dementia, only 14 of 70 GPs in the
participating municipalities diagnosed and recruited AD patients to the study. This is in
line with experiences from other studies155;156. GPs hesitate to diagnose mild cognitive
impairment or early-stage dementia and cognitive impairment is disregarded both by
relatives and health professionals, although this stage of cognitive impairment gives the
most promising interventional opportunity8;157;158.
Population-based screening
As a consequence of the low inclusion rate by GPs during the first year, the recruitment
method was extended in June 2007 to include a population-based screening of cognitive
impairment by mail. An invitation letter enclosing a questionnaire modified from the
Cambridge Examination for Mental Disorders of the Elderly159 and Strawbridge et al160
was sent to all inhabitants ≥ 65 years old in the participating municipalities. The
questionnaire comprised six questions concentrating on the main cognitive domains
affected in AD (see Postal Questionnaire). To my knowledge this was the first
community-based screening of cognitive impairment in Scandinavia and one of the first
screening procedures by mail presented in the literature47;155.
Postal Questionnaire
1. Do you want to participate in the Dementia study?
2. Has your memory deteriorated?
3. Do you forget where objects were left?
4. Do you have difficulties finding the appropriate words?
5. Do you have difficulties in managing daily activities, which earlier represented no
6. Have you been examined for memory impairment before?
An algorithm was defined, and individuals answering in accordance with it were invited
to undergo cognitive tests and clinical examination (see Algorithm). To reach a sufficient
sample size the recruitment period was extended to March 2008.
Individuals invited to undergo cognitive tests and clinical examination answered
1. "Yes" on question 1, 2, 3, 4, and 5. "No" on question 6
2. "Yes" on question 1, 2, 5 and 3 or 4. "No" on question 6
At the end of the recruitment period, 187 participants were included in the study; 87 were
recruited by GPs and 100 were recruited by population based screening (Flowchart 1).
Because two different recruitment methods were used in the study, it was important to
determine whether baseline characteristics differed across recruitment methods and
whether the two samples were equally distributed in the municipality groups. Other
studies have shown that different recruitment methods could have a significant impact on
study results and reduce validity. The first paper from the study compares baseline
characteristics between the two samples47. The study period was 39 months, 27 of which
were devoted to recruitment.
Cognitively healthy controls
Seven hundred ninety-one individuals answered "Yes" to the question on participation
and "No" to the rest. From this group, 500 individuals were randomly selected by the
Clinical Research Centre at the University Hospital in Northern Norway and invited to a
clinical examination, including cognitive testing, aiming to act as a control group for the
AD participants. Two hundred individuals were confirmed cognitively healthy, and then
included in the study (Flowchart 1). The third paper from this study presents the main
results of the interventional program whereas the second paper compares co-morbidities
and drug use between AD participants and the cognitively healthy controls.
Flowchart 1
Population-based
screening by mail
inclu ded by GPs
Respondents n (%)
Answered NO to all questions
AD individuals included after
concerning cognitive impairment and
screening and examination
YES to the question of participation
Invited to participate in the control group
Confirmed cognitively
included in the study
healthy and included
in the control group
9.2 Two-by-two factorial design
As a consequence of the diversity of design, study duration and number of stimulation
sessions in prior studies of stimulation therapy, we aimed to design a study being able to
cope with these methodological challenges. The study had an open branch consisting of
AD participants receiving stimulation therapy or standard care. All AD participants were
double-blinded randomised to donepezil or placebo in a two-by-two factorial fashion.
This design enabled a number of cross-analyses between subgroups including a head-to-
head comparison between donepezil and stimulation therapy (Flowchart 2). To our
knowledge, no study with the same design has been published in the field of AD
Flowchart 2
Stimulation therapy
Interventional municipality group
Control municipality group
The donepezil group
The placebo group included;
Donepezil + Stimulation
Placebo + Stimulation
Donepezil + Standard care
Placebo + Standard care
9.3 Outcomes
MMSE sum score was defined as the primary outcome. The results of ADAS-Cog and
Clock drawing test were defined as secondary outcomes. Basic activities of daily living
were assessed with the Barthel Index (BI)161, the Neuropsychiatric Inventory (NPI)162
was used to identify psychiatric symptoms whereas depression was assessed with a semi-
structured questionnaire and with the Montgomery and Aasberg Depression Rating Scale
9.4 Organisation and management of the study
The study was administered from a rural municipality, Steigen, in the county of
Nordland. The study centre was situated approximately half-way between the


northernmost and the southernmost points of the participating municipalities. The
distance between these extreme points was 800 km (Map 1).
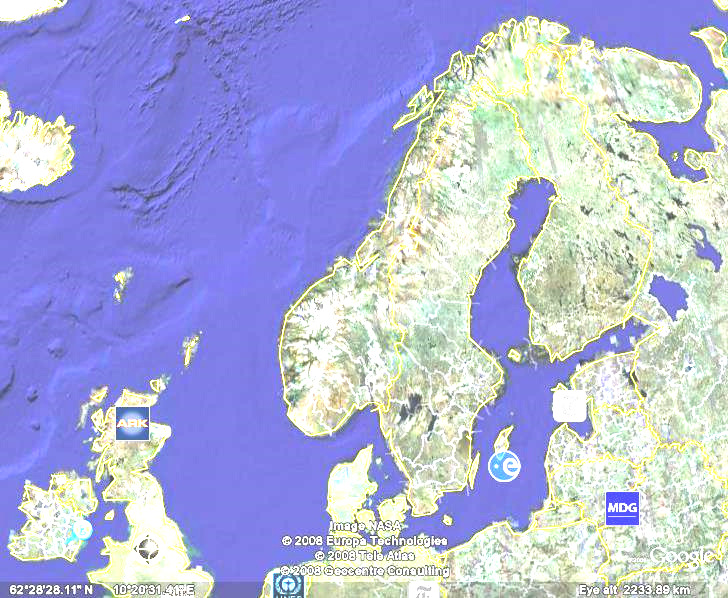
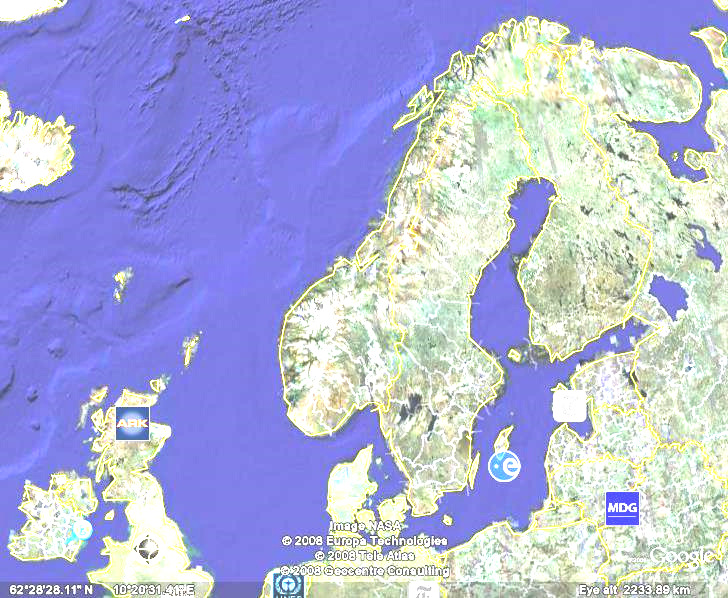
Map 1 showing the participating municipalities
Lenvik in Troms (c) Sortland (i)
Vestvågøy (i)
Steigen (i) Fauske (i)
Brønnøy (c) Sømna (c)
c= control municipality i= Interventional municipality





The staff of the Dementia Study in Northern Norway in front of the research vehicle. From the left hand
side: Herdis Svendsen, Fred Andersen, Merethe Hjertø and Kristin Tverback
The staff consisted of two test technicians, one research nurse and the project leader.
They were all employed at the municipality of Steigen, which also offered office facilities
for the study. The test technicians performed all tests in the study, among AD participants
and in cognitively healthy controls. In addition, they acted as monitors of the
interventional program. The monitoring procedures were approved by the Norwegian
Medicine Agency. As the AD participants were diagnosed and included consecutively
and followed up every fourth month for one year, the test technicians had to visit the
participating municipalities regularly during a total study period of three years. The
research nurse conducted the daily administration of the study and scheduled travel for
the test technicians. She also made appointments with the participants and their care-
givers. All participants were examined, tested and monitored at the municipality level,
sometimes in their own homes. All data were collected while the participants were
situated in their own district, and the data were recorded consecutively by the staff at the
study centre. The project leader surveyed and supervised the daily administration.
All participants recruited by screening with and without cognitive impairment were
examined and diagnosed in their own district by the project leader and physicians from
the Geriatric Department at the University Hospital in Northern Norway.
The scientific advisory board at The University of Tromsø, the County Hospital of Bodø
and the Geriatric Department at Karolinska Institutet in Stockholm supervised the study
9.5 Validating study groups
The study was community-based and run on a municipality level. Nine rural
municipalities in Northern Norway with 70000 inhabitants were engaged. The population
in the age group ≥ 65 years was 11807. The participants in five of the municipalities
received stimulation therapy whereas the participants in the remaining four received
standard care (the control municipality group) (Flowchart 1 and 2).
The municipalities were selected for the study and allocated to offer stimulation therapy
or standard care according to some basic criteria including number of inhabitants, age
distribution and ethnic homogeneity. A high professional competence level was required,
and the primary health facilities needed to be organised and developed in accordance
with the principles of good clinical practice and national guidelines. Choosing a
maximum distance and pursuing the least contact between municipalities offering
stimulation therapy or standard care were done to minimise the risk of dilution. These
selection criteria were difficult to comply with at random.
All participants were allocated to donepezil or placebo in a randomised manner, in blocks
of four to six by the Clinical Research Centre at the University Hospital in Northern
Norway. No significant differences in baseline characteristics were found between
participants receiving stimulation therapy or standard care at entry.
Dementia competence
The deficit in professional competence was reflected in an unsustainable organisation of
dementia care in general and a lack of any option for individual therapeutic adjustment
both in nursing homes and amongst outpatients in some of the participating
municipalities. Cognitive impairment amongst the elderly was ignored, or inappropriately
diagnosed and treated by the family physician, the relatives and the patient him/her self.
Nursing homes were only partly set up to take care of dementia patients.
In light of these observations and in order to ensure a professional care and follow-up of
AD participants in the Dementia Study in Northern Norway, the study administration had
to provide competence building and assistance with the construction of a suitable
dementia care in participating municipalities offering stimulation therapy. Health
professionals from all municipalities were invited to 3 main courses dealing with general
knowledge on dementia, diagnostic procedures in particular, but only 14 out of 70 GPs in
the participating municipalities attended these courses. Further more, several teaching
courses were provided at the municipality level.
9.6 Diagnosis
The same diagnostic tools and diagnostic criteria were used independently of recruitment
method. Participants recruited in general practice were examined by the community
health professionals whereas individuals recruited by screening were examined and
diagnosed by physicians from the study visiting each of the participating municipalities.
In both cases, experienced physicians conducted the clinical and neurological
examination and referred the participants to cerebral CT. Cognitive performance was
assessed by MMSE and the clock drawing test. In the present study depression was
assessed through a semi-structured questionnaire and MADRS, and basic activities of
daily living were assessed by BI. NPI identified psychiatric symptoms. Social living,
medical history and current medical use were recorded. A comprehensive number of
biochemical analyses were obtained and recorded from each AD participant. A family
member or a caregiver completed or extended the medical history and described the
impact of the disease on the caregiver's health and social life and on patient´s ADL by
answering the Informant Questionnaire-Cognitive Decline in the Elderly (IQ-CODE)164.
Blood pressure was recorded automatically by DINAMAP165 as mean arterial blood
pressure (MAP) (Appendix 1). Dementia and Alzheimer's disease were diagnosed by
experienced physicians and geriatricians using the ICD-10 and DSM-IV-TR criteria.
Diagnostic discrepancies were discussed with another geriatric colleague (Matti Viitanen)
and solved by consensus using NINCDS-ADRDA criteria for probable AD. Those
complying with the ICD-10, DSM-IV-TR and NINCDS-ADRDA criteria for probable
AD and fulfilling the inclusion/exclusion criteria were asked to participate in the study.
Inclusion criteria
Patients could be included in the study if they had a recent diagnosis of probable AD, had
not received any symptomatic treatment and were not suffering from any co-morbidity
interfering with cognitive testing or ChEI treatment. MMSE sum score needed to be 10
points or more, and age ≥ 65 but <100 years. Each participant signed informed consent
before inclusion. As a majority of the AD participants were anticipated to have reduced
consent competence, the informed consent was also co-signed by a spouse or next to kin
to comply with Norwegian national guidelines and research legislations.
Exclusion criteria
Patients suffering from dementia other than AD, serious brain injuries, infectious diseases
of the central nervous system or serious depression or psychosis were excluded. Patients
with delirium or behavioural disturbances interfering with cognitive or clinical testing,
reluctance to participate, or inability to understand the purpose of the study, or who had
relatives/caregivers who disapproved participation were also excluded.
9.7 Intervention
Stimulation therapy
A panel consisting of psychiatric nurses, university lecturers and members of the
Competence Centre of Dementia in Northern Norway (Kløveråsen) developed a program
of stimulation therapy including physical activities and cognitive, sensory and social
stimulation. A number of activities were recommended within each area (see Proposal for
intervention). This program was adjusted for each participant living in the interventional
municipalities taking functional and educational level and occupational experiences into
consideration. The stimulation was conducted for a minimum of 30 minutes 5 days a
week for one year in close co-operation with the patient and his/her family or with trained
health providers. A weekly log was used to record the daily stimulation activities. Health
professionals conducted the stimulation in nursing homes, while community nurses or
other caregivers guided by the nurses were responsible for the stimulation therapy of
community dwellers living in their own homes. The stimulation program was monitored
and adjusted during the period of intervention. Individuals living in municipalities
offering standard care received ADL support, supervision and sustainable care, as
Proposal for intervention
Physical stimulation
Walking with or without an assistant, preferably outdoors
Other outdoor activities
Training in fitness centre (therapeutic sport)
Sensory stimulation
Music, video
Wheel chair outdoors
Cognitive and social stimulation
Conversation or reminiscence groups
Reading and remembering
Playing card, chess or puzzles
Problem solving or memory training
Combined activities
Training activities of daily living
Learning hand crafts in groups
Visiting museums, farms and similar institutions
All AD participants were randomised double-blinded to donepezil or placebo in blocks of
four to six by the Clinical Research Centre at the University Hospital in Northern
Norway. (Flowchart 2) The randomisation codes were transferred to the pharmacy at the
County Hospital of Nordland, Bodø. Donepezil was prescribed to each AD participant
by their GP according to national guidelines. Then, the pharmacy distributed donepezil or
placebo to the AD participants in accordance with the prescription and the randomisation
Donepezil and placebo were delivered by Pfizer, who had no influence on the study, the
analyses of the results or publications.
9.8 Testing and follow-up
The two test technicians were trained at the Department of Geriatrics at the University
Hospital. To improve intra- and inter-rate reliability they observed and evaluated each
other by testing a number of patients with MMSE, ADAS-Cog, the clock drawing test,
NPI and MADRS. The same test technician followed each participant during the study
period over one year. The same diagnostic procedures were used to test the self-reported
cognitively healthy control group.
During the one-year follow-up period MMSE, the clock drawing test and ADAS-Cog
were performed at baseline and at 4, 8 and 12 months, whereas NPI, MADRS and BI
were performed at baseline and at 12 months.
At the end of the study, blood samples were collected from 152 of the AD participants
and from 200 of the cognitively healthy controls.
10. Ethical considerations
10.1 Consent competence
AD individuals included in a clinical trial have varying degrees of reduced consent
competence and reduced ability to understand oral or written information. In early
disease stages, they usually are able to decide in a rational manner which choices will fit
them best, participating in the study or not. At this stage a stand in should not be allowed
to interfere with the patient's decision. Later on, a spouse or a next of kin should be asked
to take responsibility for the decision-making process on behalf of the patient.
Monitoring patients with impaired cognitive functions who participate in an
interventional clinical trial requires specially awareness. The monitor and caregiver must
observe sign of adverse reactions and any expressed reluctance to participate or inability
to understand the purpose of the study. Signs such as these require immediate exclusion
from the study at any time during follow-up. Participants´ well-being must always be
considered a main concern in any clinical trial, especially when it comes to participants
with cognitive impairment
10.2 Study design
Ethical considerations of randomised placebo-controlled, double-blinded trials with new
drugs for AD have been discussed since 1996166. It has been argued that Phase IV studies
of ChEIs could be unethical according to the modest and statistically significant effect of
the drugs on cognition167;168. However, the contradictory outcome of numerous RCTs on
ChEI in addition to high drug costs and fear of adverse reaction underlay the decision to
perform the present study.
The medical history of chemicals with ChEI effects is scaring and should be considered
carefully, especially as it comes to the development of new drugs aimed to treat
individuals with reduced consent competence (see Appendix).
10.3 Approvals
The present study was approved in advance by national authorities including the Regional
Committee for Medical Research Ethics in Northern Norway, the Privacy Ombudsman
for Research, the Directory of Health and Social Welfare and the Norwegian Medicine
Agency included registration of the study in the EudraCT database (no 2004-002613-37).
Each AD participant gave written informed consent co-signed by a spouse, a close
relative or a guardian. The national authorities listed above approved the consent formula
and the study is also registered as an International Standard Randomized Controlled Trial
within ClinicalTrials.gov (Identifier: NCT00443014). In October 2008 The Norwegian
Medicine Agency conducted an inspection according to the principles of Good Clinical
Practice (GCP) in a randomised clinical trial. All remarks from this assessment, including
monitoring routines were closed and approved. The study was then given a signed
approval by the Norwegian Medicine Agency as a RCT in accordance with the GCP
criteria. All publications from this study comply with the CONSORT statements and the
Uniform Requirements for Manuscripts Submitted to Biomedical Journals169;170.
11. Data and statistics
11.1 Data recording
The demographic characteristics, medical history, clinical examination, cognitive tests
and current medical use of AD participants and cognitively healthy controls were
recorded at study entry. Cognitive tests were registered at four time points during one
year for each AD participant. At the end of the study period the database was assessed,
secured and locked by the Clinical Research Centre at The University Hospital in
11.2 Statistics
Statistical analysis was conducted using SPSS version 15.0 and 16.0(SPSS Inc. Chicago,
IL, USA). Based on the calculation of power, a sample size of 64 in each group was
necessary to detect a 2-point difference in mean MMSE sum score with 80% power,
provided a standard deviation of 4 and a two-sided significance level of 5%. Differences
in demographic characteristics between municipality groups and medicine groups and
between recruitment methods as well as the comparison of co-morbidity and drug use
between AD participants and cognitively healthy controls were assessed by Chi-square
and independent-samples t-tests. Analyses of co-variance (ANCOVA) and logistic
regression were used for age and gender adjustment. Linear mixed models were used to
assess time-trends in cognitive function over four time points and to assess differences in
time-trends between groups of AD participants. Including an unstructured covariance
matrix in the model controlled for possible dependences between repeated observations.
In the municipality groups, time-trend differences in cognitive function were assessed
between the stimulation group and control group, and differences in the medicine groups
were assessed between the donepezil treatment group and the placebo group. Finally, the
subgroup treated by stimulation therapy and donepezil was compared to the subgroup
receiving usual care and placebo. Model assumptions were assessed by means of residual
analyses. The statistical analyses were performed with intention-to-treat, per-protocol and
subgroup analyses in order to estimate the homogeneity and consistency of the data. In
the sensitivity analyses we included municipality as a random effect in the linear mixed
models in order to control for possible clustering of data within the municipalities.
12. Results
12.1 Recruitment methods and baseline characteristics
During the first year 27 AD individuals were included by GPs. After extending the
recruitment method to comprise a population-based postal screening of cognitive function
in individuals ≥ 65 years another 160 participants were included during the next year, 100
by screening and 60 by GPs in clinical practice. In this way the study AD participants
were included by two different recruitment methods (Flowchart 3).
Participants recruited by screening were more frequently male (p< 0.001), younger (p =
0.006), more independent and needed less community support (p< 0.001), as compared to
those recruited by GPs. Also, they had a higher ADL function as assessed by the Barthel
Index (p=0.011) and had a significantly higher MMSE sum score (p=0.001). No
significant differences in neuropsychiatric symptoms (NPI) were found. Participants
recruited by screening had a significantly higher MADRS score compared to participants
recruited in clinical practice (Table 1).
Further analyses revealed that each sample was equally distributed across the main study
groups. No significant differences in age, gender, cognitive function, neuropsychiatric
symptoms or need for ADL support were found between AD participants in the
interventional municipalities compared to AD participants in the control municipalities
Flowchart 3 Population-based screening of self-reported cognitive impairment
Population-based
screening by mail
algorithm n=3329
Invited to examination
Withdrawals n=146
Received cognitive
Withdrawals n=63
Clinical examination
Excluded, not AD
Alzheimer's disease
Withdrawals n=13
Included in the study
Table 1 Comparison of age, gender and MMSE score at baseline between recruitment
methods
Recruitment method
Screening
Clinical practice
MMSE ± SD
Barthel Index ± SD
19.23 ± 2.07
17.96 ± 3.38
8.18 ± 11.50
In need of ADL support n (%)
* Adjusted for age
Table 2 Comparison of baseline characteristics between stimulation therapy and standard
care.
AD participants receiving
Stimulation
Standard care
MMSE ± SD
Barthel Index ± SD
In need of ADL support n (%)
12.2 A cross-sectional comparison of co-morbidities and current medication between
participants with and without AD
Data on past medical history, co-morbidities and current medication was recorded at
study entry. AD participants were older (80.9 ± 7.0 vs 72.5 ± 5.5 p<0.001) and the female
fraction was significant higher (60% vs 43% p<0.001) compared to controls. No
significant age- or gender-adjusted differences in co-morbidities were found between AD
participants stratified on disease stages. However, the total number of drugs was
significantly higher in AD participants compared to controls despite no differences in co-
morbidities. When participants were stratified by ATC group a significant higher use of
drugs with anticholinergic activity, anxiolytics/hypnotics and antidepressants was found
in the AD group compared to the control group. Only four of the AD participants used
antipsychotics. The number of antihypertensive drugs was significantly higher, nearly
doubled, in AD participants compared to controls.
One hundred and forty-two AD participants were living at home, 40 of them received
ADL support from community nurses at least once a week. Forty-five AD participants
lived in nursing homes (1 missing). Nursing home AD residents and the most disabled
community dwellers used significantly more drugs than those living in their own homes
without any regular ADL support. This included both the total number of drugs
(p<0.001), drugs classified as inappropriate according to the STOPP criteria152 (p<0.001),
drugs exhibiting the two highest levels of anticholinergic activity assessed by the
Anticholinergic Risk Scale (ARS) (p=0.001)171, antidepressants (p<0.001) and
anxiolytics/hypnotics (p<0.001) (Table 5).
MAP (Formula 1) adjusted for age and gender was significantly lower in AD participants
compared to controls. A family history of AD was significantly more common in AD
participants compared to controls. Sixty-three per cent of the participants in the control
group had completed ≥ 10 years of education compared to 17% in the AD group.
However, after age and gender adjustment this was not significant (p=0.33).
Table 3 Comparison of drug use between AD participants with and without regular ADL
support
Mean drug number± SD
Inappropriate drugs n(%)
Anticholinergic drugs
Anxiolytics/hypnotics
Antidepressants n (%)
12.3 Symptomatic treatment
The follow-up period of AD individuals included in the study was one year. Cognition
was tested four times at four-month intervals. Forty-one individuals dropped out during
follow-up as a consequence of death (n=7), disease progression (n= 8), co-morbidities
(n= 8) and withdrawal for unknown reason (n=18). One hundred forty-six completed the
program (Flowchart 4). Forty-one AD participants (41.5%) in the stimulation therapy
group completed a total of 200 or more sessions of stimulation therapy as assessed by
approved logs during one-year follow-up whereas 53 AD participants (55.9%) in the
donepezil group completed drug treatment for 42 weeks or more.
No significant time-trend differences in cognitive test performance were found between
AD participants receiving stimulation therapy and standard care as assessed by MMSE
(primary outcome), the clock drawing test and ADAS-Cog (secondary outcome) during
the one-year follow-up. Both AD participants allocated to stimulation therapy and AD
participants allocated to standard care with or without donepezil retained cognitive
function as assessed by the three tests. The results were consistent in the intention-to-treat
and per-protocol analyses (Chart 1). Subgroup analyses of participants with MMSE score
≤25 (Chart 2 and Table 5), and MMSE score ≤ 21 at entry and stratified on recruitment
methods (not in chart) were consistent with the intention-to-treat analyses.
No significant time-trend differences in cognitive function between groups with
donepezil and placebo with or without stimulation therapy were found (Chart 3).
Participants receiving donepezil had significantly more adverse reactions (28%) than
those receiving the placebo (10%) (odds ratio 3.80 95% CI 1.55 to 9.54 p=0.002). A
subgroup analysis comparing the combined effect of stimulation therapy and donepezil
versus standard care and placebo did not reveal any time-trend differences between the
groups regarding cognitive achievements (Chart 4). On Chart 4 the expected decline in
mean MMSE sum score is plotted. Stimulation therapy with placebo compared to
donepezil treatment with standard care (representing a head to head comparison of
stimulation therapy versus donepezil) did not demonstrate any time-trend differences in
cognitive performance (Chart 5). Only small changes in ADL and neuropsychiatric
functions were found after one-year follow-up (Table 4). Intention-to-treat, per-protocol
and the subgroup analyses were consistent across the three independent cognitive tests.
Flowchart 4
Dropouts during follow-up
Test 1 to test 4 n=34
at test 1, n=146
MMSE sum score at test 1, n=34 22.16 ± 4.47
Chart 1 A comparison between stimulation therapy and standard care at each time point
MMSE score. Stimulation therapy versus
standard care
Stimulation therapy
Time point (four-month intervals)
Chart 2 Mean MMSE sum score at each time point for all participants compared to
participants with mean MMSE score < 26 at entry
MMSE score 1-year follow-up
Entry MMSE<26 n=114
Time point (four-month intervals)
Chart 3 Comparison between donepezil and placebo
MMSE score
Donepezil versus placebo at each time point
Time point (four-month intervals)
Chart 4 The extreme limit comparison between donepezil combined with stimulation
therapy and placebo combined with standard care at each time point
MMSE score
Donepezil + Stimulation therapy versus Placebo + standard care
Donepezil + stimuli
Placebo + Control
Expected decline
Time point (four-month intervals)
Chart 5 Head to head comparison of stimulation therapy + placebo versus donepezil +
standard care measured by ADAS-Cog (stimulation n= 50, donepezil n=37)
ADAS-Cog Stimulation versus donepezil
Time points (four-month intervals)
Table 4 Neuropsychiatric symptoms and ADL function at entry and after one-year
follow-up stratified by interventional groups.
Stimulation
Standard
Donepezil
18.64± 2.55 18.64 ± 3.20 18.87±2.12 18.41 ± 3.38
One year 18.41± 2.87 18.25 ± 3.59 18.50±2.45 18.17 ± 3.83
MADRS One year 2.63 ± 3.88 2.09 ± 3.61 2.71 ± 3.95
6.08 ± 9.59 8.49 ± 10.52 7.49±11.14
One year 6.56 ± 9.57 9.61 ± 12.88 7.83±11.32 7.97 ± 11.27
Table 5. Mean cognitive test performances at follow-up time points in AD participants
receiving stimulation therapy compared to standard care, and donepezil compared to
placebo. Patients with entry MMSE ≤ 25 (n=114)
Moments of follow up
*n varies due to dropouts during follow-up. ** Adjusted for gender p=0.37 Adjusted for age p=0.11 †Adjusted for gender p=0.23. Adjusted for age p=0.85 Adjusting for age or gender did not change other p-values in the analyses
13. Discussion
13.1 Recruitment methods and selection bias.
Baseline characteristics differed significantly between AD individuals recruited in
clinical practice and by population-based screening. These findings underscore the
impact of sampling methods aimed to select a representative study sample from the
source population. Baseline characteristics of the AD participants should be similar to or
not differ significantly from, the source population (internal validity). The present study
was community-based with an unselected population of recently diagnosed AD
participants recruited by GPs or by population-based screening (Flowchart 1). The
clinical examinations were performed by experienced general practitioners supervised by
geriatric specialists. The results confirm that different recruitment methods within the
same population provide samples with significant differences in several baseline
characteristics. Similar findings have been reported by Izal et al. who emphasise that
recruitment method can specifically influence the outcomes of studies with elderly people
and limit the generalization of their results9. Population-based recruitment conducted in
the community without stringent inclusion criteria is supposed to come closest to a
representative sample and should achieve the highest external validity99;172.
Assessing internal validity172 in dementia studies is challenging. Dementia is still a
syndrome based on clinical criteria without a golden standard. Few, if any, positive
biomarkers are routinely in use and the current diagnostic tools rely upon questionnaires,
tests and clinical examinations with insufficient accuracy and corresponding low
sensitivity and specificity27;94. Sampling will therefore always be at risk of
misclassification and selection bias. Women are at a higher risk of AD than men in some
studies173;174. It is therefore important that gender distribution in the sample match that of
the study population. According to 2008 Norwegian statistics, the female proportion of
the population 67 - 79 years and 80 years and above are 53.6% and 65.0%,
respectively175. In our study the gender distribution is similar to national statistics (Mean
age 80.9 ± 7.0; 60.4% female).
According to the known incidence rate (2 – 4%)176 and prevalence (10%)71 of AD in the
population 65 years and above, the number of eligible individuals with a recent diagnosis
of AD in the participating municipalities was at least double what we were able to recruit.
The screening program recruited younger and healthier individuals. Older eligible AD
individuals with more advanced disease were possibly not accessible by a postal
questionnaire as some of them were diagnosed earlier or lived in nursing homes. Studies
on elderly may be biased by this healthy participant bias. GPs often hesitate to diagnose
mild cognitive impairment or early-stage of dementia158. Mild to moderate cognitive
impairment in the elderly, including early-stage AD, seems to be disregarded by both
relatives and health professionals, even though this stage of cognitive impairment has the
best response to intervention. Our findings are in accordance with others who reported
that GPs tend to postpone a comprehensive examination of patients who complain of
memory problems. When dementia is mild more than 90.9% of the cases are
overlooked177. When dementia is severe the specificity is greater than 99%157;177;178.
The questionnaire developed from the Cambridge Cognitive Examination and
Strawbridge et al. along with the defined algorithm seemed to be highly valid in selecting
individuals with cognitive impairment. Of 438 individuals selected by the algorithm to
have probable cognitive impairment 229 underwent cognitive testing and clinical
examination. Of these 113 were diagnosed with probable AD representing 2.9% of the
responders (Flowchart 1) and more than one quarter of those selected by the algorithm.
Seven hundred and ninety-one responders from the screening reported no cognitive
impairment but still wanted to participate in the study. Five hundred individuals from this
group were randomly allocated to the control group, and 200 received cognitive and
clinical examination. All of them were confirmed to be cognitively healthy. In this way
the present postal questionnaire combined with the algorithm was able to identify
individuals with cognitive disabilities corresponding to early AD.
In a large-scale community memory screening by Lawrence et al (2003) community
dwellers were invited through the media to undergo cognitive assessment. Of those
attending the screening program 1.5% had an undiagnosed AD. Considering the
prevalence of dementia, this was lower than expected, and the cost-effectiveness of the
screening procedures could be questioned156. However, in their study the invitation to the
screening program came through media. No preliminary questionnaire specifically
addressing cognitive complains followed the invitation and no algorithm was used. Crew
et al. (2009) also used the media and flyers to recruit participants to be screened for
cognitive impairment and neuropsychiatric symptoms. They found that 24% of the
participants who completed the screening program received follow-up recommendation
secondary to objectively identified age-inappropriate memory impairment. Crew et al.
concluded that there appears to be a critical need for widespread use of screening
programs to identify early age-inappropriate memory impairment155.
According to the experiences of the present study, screening of cognitive impairment by
mail with a preliminary questionnaire covering main cognitive domains followed by
cognitive tests and clinical examination could be a useful tool to identify early stage AD
in the community. However, screening such as this does not comply with a preclinical
dementia stage or dementia risk factors179.
13.2 Co-morbidities and current medication in participants with and without AD
The cross-sectional analyses compared co-morbidities and current medication between
AD participants and a cognitively healthy control group (paper 2). The results reveal an
increased number of daily medications in AD individuals, especially anticholinergic and
psychotropic drugs compared to the control group. Increasing drug consumption was
associated with cognitive deterioration, the need for ADL support and institutionalisation.
Psychotropic drugs exhibit an additional suppression of cognitive abilities in AD131;132.
Adverse drug events increase from 10% with one drug to 75% in patients taking five
drugs180. An increased number of drugs also increases the risk of potentially
inappropriate medication181. In our study 48% of AD participants used five drugs or
more. Nursing home AD residents used nearly seven drugs a day. Fifty-four per cents of
AD participants living in nursing homes or in their own homes with regular ADL support
from community nurses used drugs defined inappropriate according to the STOPP
criteria152. This finding could call for a more extensive adjustment of drug treatment
amongst AD individuals in primary health care or nursing homes. Interruption of
inappropriate drugs may represent a therapeutic option to improve cognitive
performance182, especially when it comes to simultaneous treatment with drugs exhibiting
anticholinergic activities and ChEIs.
AD is associated with cardiovascular risk factors and metabolic syndrome. However, the
comparison of other co-morbidities between individuals with and without dementia has
given ambiguous results82;183-185. In the present study, no age- or gender-adjusted
differences in the number of co-morbidities between individuals with and without AD
were found. This is in line with other studies184;185. However, AD individuals may suffer
from more advanced illnesses186. In our study further analyses revealed a significantly
lower mean arterial blood pressure and more antihypertensive drug use in AD
participants compared to controls. This is in accordance with the findings of Guo et al187.
The combination of reduced blood pressure and increased occurrence of vascular
disorders, especially small-vessel diseases, could have an impact on cerebral perfusion
and reinforce cognitive disabilities in individuals with a neurodegenerative disease108.
When this is added to the heavy burden of inappropriate medical treatment both cognitive
and ADL functions could be further suppressed.
Low education has been identified as a risk factor in AD. Only 17% (33 of 187) of the
AD participants had completed ≥ 10 years of education compared to 63% (126 of 200) of
the control group. The mean age difference between the two study groups was
approximately eight years, and this age difference could be related to differences in
education attainment. At the beginning of World War II (1939/1940), the mean age of the
AD participants in the present study was 12 years. Many inhabitants in Northern Norway
lost several years of education as a consequence of the warfare. The mean age of the
participants in the control group in 1939/1940 was 3 years, and they could easily make up
for delayed school attendance after 1945. In our study, therefore, the difference in
education level between the two study groups could be explained by World War II.
13.3 Symptomatic treatment
The main result of this one year trial was that no differences in cognitive performance
were detected between AD participants receiving stimulation therapy compared to AD
participants receiving standard care. To our surprise both groups retained cognitive
performance during the study period. The results were consistent for three different
cognitive tests. This observation differs from other comparable studies23;125. The inherent
trajectory in AD represents a decline in MMSE sum score of 2-3 points and an increase in
ADAS-Cog score of 6 -12 points per year. The cognitive deterioration depend upon
disease severity at baseline66;67;188. The milder the baseline cognitive impairment, the
slower the disease progression188. Stabilising cognitive performance is an important
outcome in symptomatic treatment of AD38. Previous studies of symptomatic treatment
with various designs have reported a postponement of disease progression for
approximately one year in interventional groups37;125 and a variable cognitive decline in
the control groups16;18;21;125;189. Equal effects, with retention of cognitive performance in
both the interventional as well as the control groups, have to our knowledge not been
reported. In concordance with results of previous studies, stimulation therapy and/or
donepezil treatment in the present study was presumed to delay cognitive deterioration in
the follow-up period. To our surprise, the control group receiving standard care with or
without donepezil retained cognitive performance as well.
Several events and mechanisms may explain the similar cognitive performances between
participants receiving stimulation therapy and standard care. The equal effects on
cognitive test performance in AD participants receiving stimulation therapy compared to
standard care with and without donepezil with preservation of cognitive abilities during
one year could partly be explained by a placebo, expectancy or Hawthorne
effect43;44;190;191. The present study was not designed to evaluate the placebo effect and
the outcomes of the study have to be discussed with caution. However, participation in a
trial like the present study, with frequent monitoring and follow-ups, may create
expectancy192 and act as cognitive stimulation by itself. The test-technicians visited the
municipalities regularly for three years. Their visits were obviously an important event
booth for the AD participants and the caregivers. The question arises whether the placebo
effect of study participation could have provided high expectancy and cognitive
stimulation in all subgroups leaving a possible stimulation and/or donepezil effect
undetectable42;190;193. In a review of stimulation therapy in AD Olazaran et al. (2010)
found that increased attention to the control groups reduced the differences in cognitive
functions between interventional and control groups and could blur study results24. If so,
this could have hampered other trials with symptomatic treatment of AD individuals and
partly explain the contradictory results of many dementia studies. Neuropsychological
mechanisms within the placebo effect could have seriously biased the outcomes.
Benedetti et al found that the placebo effect depends upon preserved frontal lobe
function. Decreasing executive functions were associated with a reduced placebo effect.
In our study, frontal executive functions were not explicitly assessed, and retaining
cognitive function during one-year follow-up was independent of disease stage measured
by MMSE sum score at entry. The subgroup of AD participants with MMSE ≤ 21 at
entry (n=59, mean MMSE sum score 18.4 ± 2.7) preserved cognitive performance during
one-year follow-up as well.
Previous studies of symptomatic treatment have reported a postponement of disease
progression for approximately one year45;194. The stabilising effect on cognitive
performance seems to occur irrespective of what symptomatic treatment was offered,
whether stimulation therapy, symptomatic drug treatment, or stimulation therapy added to
the symptomatic drug treatment (donepezil)125. The maintenance of the cognitive
performances is an important treatment goal in AD. Postponing functional worsening is
favourable for both the patients and their caregivers38 and may delay institutionalisation
for some AD patients18.
Health professionals in both municipality groups attended the same dementia competence
courses; whereas courses that aimed to qualify stimulation therapy providers were
reserved for interventional municipality health professionals. A national campaign on AD
was launched around the time of our study. These concomitant events could have diluted
the municipality differences and influenced standard care in control municipalities. The
stimulation program in our study was developed by experienced dementia therapists,
adjusted individually and provided by trained primary health nursing staff or
caregivers/family members and was designed to be sustainable for months without
extensive costs. So far, no standardised and validated stimulation therapy programmes
are available195. Growing evidence indicates that combining the stimulation benefits of
educational, occupational and mental activities (cognitive reserves) with physical
activities and a healthy life style are the most important modifiable risk factors in AD13;27.
The stimulation program in the present study was in accordance with these
recommendations.
Except for adverse reactions, an effect of donepezil compared to placebo with or without
stimulation therapy was not detectable. Both the donepezil and the placebo group
retained cognitive function during one year follow-up.
Interestingly the main result of the present study is in agreement with the casuistry
described in the introduction.
13.4 Strengths and weaknesses
The present study was community-based with well defined but not too stringent
inclusion/exclusion criteria. The sampling method was designed to recruit a
representative sample of newly diagnosed AD participants from the source population.
The population-based screening program provided in the present study is to, my
knowledge, the only one conducted in Scandinavia. The participants remained in their
own environment, and a significant number of participants completed the one-year
follow-up. Few interventional studies with stimulation therapy have accomplished a one-
year follow-up. A study design such as ours, with a two-by-two factorial design, focusing
on stimulation therapy and donepezil treatment and including a head-to-head comparison,
has previously been advocated by the scientific community10 but has previously not been
accomplished. The control group, consisting of self-reported and clinical confirmed
cognitively healthy individuals, constitutes the only randomly selected control group in
AD research in Norway. In April 2009, after an inspection according to the principles of
GCP in a randomised clinical trial, the study was given signed approval by the
Norwegian Medicine Agency as an RCT conducted in accordance with the GCP criteria.
The participating municipalities were not randomly selected but recruited according to a
number of criteria, including the competence of the health providers, demographic
characteristics of the population and geographic location. Choosing maximum distance
and pursuing the least contact between interventional and control municipalities were
done to minimise the risk of dilution. Such a non-randomised selection could be
considered as a limitation of the study. However, the study population in the participating
municipalities was ethnically and socially homogenous, and the baseline characteristics
did not differ either between AD participants receiving stimulation therapy compared to
standard care or between AD participants receiving donepezil or placebo. In addition, a
sensitivity analysis in order to control for possible clustering of data within the
municipalities did not change the results.
The retention of cognitive function in the present study could have occurred because of
early AD stage at entry with minimal cognitive decline during follow-up188. In a review
by Sevigny et al. (2010) of a 12-month, multicentre, double-blinded RCT, the AD
participants in the placebo group were dichotomised according to baseline MMSE sum
score into mild disease (MMSE 21 – 26) and moderate to severe disease stage (MMSE 14
- 20). The outcome measure was the percentage changes in ADAS-Cog score during the
12-month follow-up. The total rate of cognitive decline in participants with mild AD
according to ADAS-Cog was less than that of participants with moderate to severe AD196.
Although AD participants in our study were examined, diagnosed and followed with a
variety of tests, diagnosing mild AD remains a challenge. The mean MMSE sum score at
baseline was 23.0 ± 3.9, representing the mild AD stage. According to Sevigny et al the
cognitive decline in our study could therefore have been less than expected during
follow-up. However, in the study analysed by Sevigny et al., all AD participants were
treated with ChEI or memantine196, which could have had a different impact on cognitive
decline in participants with mild AD compared to participants with moderate to severe
AD during the 12-month follow-up. In our study, subgroup analyses of AD participants
recruited by GPs (n=87), AD participants with MMSE sum score ≤ 25 at entry (n=121)
and with MMSE sum score ≤ 21 at entry (n=55) were consistent with the intention to
The subgroup analyses of the study cover a wide range of possible interactions between
strata, independent variables and outcomes (Charts 2 and 5). Some of these two-by-two
factorial strata are small and could be at risk of type II error. However, the results of all
analyses were consistent across a number of different comparisons and three cognitive
14. Conclusion
A population-based postal screening of cognitive function with a subsequent clinical
examination is suitable to identify early-stage AD.
AD individuals used significantly more medication than controls, and particularly the use
of anticholinergic drugs is worrying. A careful evaluation and interruption of possible
inappropriate drug use in AD individuals at any disease stage may represent a therapeutic
option to improve cognitive performance.
The two-by-two factorial design of The Dementia Study in Northern Norway provides an
opportunity to compare the effects of two different interventional methods on cognitive
performance in AD individuals. The negative effect of symptomatic treatment in AD with
or without donepezil compared to controls, with retention of cognitive abilities in all
groups during a one-year follow-up was a surprise and may have been a consequence of
participants' expectancy and the psychosocial context of the intervention. The possibility
of postponing cognitive deterioration by at least one year in AD individuals with mild to
moderate cognitive impairment was confirmed.
15. Reference list
Reference List
(1) Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical
method for grading the cognitive state of patients for the clinician. J
Psychiatr Res 1975; 12(3):189-198.
(2) Dorland´s Illustrated Medical Dictionary. 28 ed. 1994.
(3) Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M et al.
Global prevalence of dementia: a Delphi consensus study. Lancet 2005;
366(9503):2112-2117.
(4) Goedert M, Spillantini MG. A century of Alzheimer's disease. Science
2006; 314(5800):777-781.
(5) Winblad B, Engedal K, Soininen H, Verhey F, Waldemar G, Wimo A et al.
A 1-year, randomized, placebo-controlled study of donepezil in patients
with mild to moderate AD. Neurology 2001; 57(3):489-495.
(6) Feldman HH, Ferris S, Winblad B, Sfikas N, Mancione L, He Y et al. Effect
of rivastigmine on delay to diagnosis of Alzheimer's disease from mild
cognitive impairment: the InDDEx study. Lancet Neurol 2007; 6(6):501-
512.
(7) Kadir A, Andreasen N, Almkvist O, Wall A, Forsberg A, Engler H et al.
Effect of phenserine treatment on brain functional activity and amyloid in
Alzheimer's disease. Ann Neurol 2008; 63(5):621-631.
(8) Carter RE, Rose DA, Palesch YY, Mintzer JE. Alzheimer's Disease in the
Family Practice Setting: Assessment of a Screening Tool. Prim Care
Companion J Clin Psychiatry 2004; 6(6):234-238.
(9) Izal M, Nuevo R, Montorio I, Perez-Rojo G. Method of recruitment and the
scores of self-report measures: the example of worry in the elderly. Arch
Gerontol Geriatr 2009; 48(1):45-49.
(10) Golden J, Lawlor B. Treatment of dementia in the community. BMJ 2006;
(11) Vaglum P. [The comprehensive summary of doctoral dissertation--what
should it contain?]. Tidsskr Nor Laegeforen 2010; 130(16):1632-1634.
(12) Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on
elderly persons with cognitive impairment and dementia: a meta-analysis.
Arch Phys Med Rehabil 2004; 85(10):1694-1704.
(13) Clare L, Woods RT, Moniz Cook ED, Orrell M, Spector A. Cognitive
rehabilitation and cognitive training for early-stage Alzheimer's disease
and vascular dementia. Cochrane Database Syst Rev 2003;(4):CD003260.
(14) Luijpen MW, Scherder EJ, Van Someren EJ, Swaab DF, Sergeant JA.
Non-pharmacological interventions in cognitively impaired and demented
patients--a comparison with cholinesterase inhibitors. Rev Neurosci 2003;
14(4):343-368.
(15) Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M et al.
Effects of cognitive training interventions with older adults: a randomized
controlled trial. JAMA 2002; 288(18):2271-2281.
(16) Graff MJ, Vernooij-Dassen MJ, Thijssen M, Dekker J, Hoefnagels WH,
Rikkert MG. Community based occupational therapy for patients with
dementia and their care givers: randomised controlled trial. BMJ 2006;
333(7580):1196.
(17) Lautenschlager NT, Cox KL, Flicker L, Foster JK, van Bockxmeer FM,
Xiao J et al. Effect of physical activity on cognitive function in older adults
at risk for Alzheimer disease: a randomized trial. JAMA 2008;
300(9):1027-1037.
(18) Metitieri T, Zanetti O, Geroldi C, Frisoni GB, De LD, Dello BM et al.
Reality orientation therapy to delay outcomes of progression in patients
with dementia. A retrospective study. Clin Rehabil 2001; 15(5):471-478.
(19) Orrell M, Spector A, Thorgrimsen L, Woods B. A pilot study examining
the effectiveness of maintenance Cognitive Stimulation Therapy (MCST)
for people with dementia. Int J Geriatr Psychiatry 2005; 20(5):446-451.
(20) Avila R, Carvalho IA, Bottino CM, Miotto EC. Neuropsychological
rehabilitation in mild and moderate Alzheimer's disease patients. Behav
Neurol 2007; 18(4):225-233.
(21) Chapman SB, Weiner MF, Rackley A, Hynan LS, Zientz J. Effects of
cognitive-communication stimulation for Alzheimer's disease patients
treated with donepezil. J Speech Lang Hear Res 2004; 47(5):1149-1163.
(22) Loewenstein DA, Acevedo A, Czaja SJ, Duara R. Cognitive rehabilitation
of mildly impaired Alzheimer disease patients on cholinesterase inhibitors.
Am J Geriatr Psychiatry 2004; 12(4):395-402.
(23) Spector A, Thorgrimsen L, Woods B, Royan L, Davies S, Butterworth M et
al. Efficacy of an evidence-based cognitive stimulation therapy programme
for people with dementia: randomised controlled trial. Br J Psychiatry
2003; 183:248-254.
(24) Olazaran J, Reisberg B, Clare L, Cruz I, Pena-Casanova J, Del ST et al.
Nonpharmacological therapies in Alzheimer's disease: a systematic review
of efficacy. Dement Geriatr Cogn Disord 2010; 30(2):161-178.
(25) Yamaguchi H, Maki Y, Yamagami T. Overview of non-pharmacological
intervention for dementia and principles of brain-activating rehabilitation.
Psychogeriatrics 2010; 10(4):206-213.
(26) Andrade C, Radhakrishnan R. The prevention and treatment of cognitive
decline and dementia: An overview of recent research on experimental
treatments. Indian J Psychiatry 2009; 51(1):12-25.
(27) Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E.
Alzheimer's disease. Lancet 2011; 377(9770):1019-1031.
(28) Winblad B, Hardy J, Backman L, Nilsson LG. Memory function and brain
biochemistry in normal aging and in senile dementia. Ann N Y Acad Sci
1985; 444:255-268.
(29) Mangialasche F, Solomon A, Winblad B, Mecocci P, Kivipelto M.
Alzheimer's disease: clinical trials and drug development. Lancet Neurol
2010; 9(7):702-716.
(30) Birks JS, Melzer D, Beppu H. Donepezil for mild and moderate
Alzheimer's disease. Cochrane Database Syst Rev 2000;(4):CD001190.
(31) Qaseem A, Snow V, Cross JT, Jr., Forciea MA, Hopkins R, Jr., Shekelle P
et al. Current pharmacologic treatment of dementia: a clinical practice
guideline from the American College of Physicians and the American
Academy of Family Physicians. Ann Intern Med 2008; 148(5):370-378.
(32) Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M et al.
Effectiveness of cholinesterase inhibitors and memantine for treating
dementia: evidence review for a clinical practice guideline. Ann Intern Med
2008; 148(5):379-397.
(33) Trinh NH, Hoblyn J, Mohanty S, Yaffe K. Efficacy of cholinesterase
inhibitors in the treatment of neuropsychiatric symptoms and functional
impairment in Alzheimer disease: a meta-analysis. JAMA 2003;
289(2):210-216.
(34) Wolfson C, Oremus M, Shukla V, Momoli F, Demers L, Perrault A et al.
Donepezil and rivastigmine in the treatment of Alzheimer's disease: a best-
evidence synthesis of the published data on their efficacy and cost-
effectiveness. Clin Ther 2002; 24(6):862-886.
(35) Dillon A. Alzheimer´s disease - donepezil, galantamine, rivastigmine and
memantine (NICE review) http://www.nice.org.uk/TA111. 2007. NICE.
Ref Type: Report
(36) Kaduszkiewicz H, Zimmermann T, Beck-Bornholdt HP, van den BH.
Cholinesterase inhibitors for patients with Alzheimer's disease: systematic
review of randomised clinical trials. BMJ 2005; 331(7512):321-327.
(37) Rogers SL, Friedhoff LT. Long-term efficacy and safety of donepezil in the
treatment of Alzheimer's disease: an interim analysis of the results of a US
multicentre open label extension study. Eur Neuropsychopharmacol 1998;
8(1):67-75.
(38) Tariot PN. Maintaining cognitive function in Alzheimer disease: how
effective are current treatments? Alzheimer Dis Assoc Disord 2001; 15
Suppl 1:S26-S33.
(39) Dumitriu A, Popescu BO. Placebo effects in neurological diseases. J Med
Life 2010; 3(2):114-121.
(40) Benedetti F, Carlino E, Pollo A. How placebos change the patient's brain.
Neuropsychopharmacology 2011; 36(1):339-354.
(41) Miller FG, Colloca L. Semiotics and the placebo effect. Perspect Biol Med
2010; 53(4):509-516.
(42) Colagiuri B. Participant expectancies in double-blind randomized placebo-
controlled trials: potential limitations to trial validity. Clin Trials 2010;
7(3):246-255.
(43) Wolfe F, Michaud K. The Hawthorne effect, sponsored trials, and the
overestimation of treatment effectiveness. J Rheumatol 2010; 37(11):2216-
2220.
(44) Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD,
Shelton RC et al. Antidepressant drug effects and depression severity: a
patient-level meta-analysis. JAMA 2010; 303(1):47-53.
(45) de lF-F, Schulzer M, Stoessl AJ. The placebo effect in neurological
disorders. Lancet Neurol 2002; 1(2):85-91.
(46) Benedetti F, Arduino C, Costa S, Vighetti S, Tarenzi L, Rainero I et al.
Loss of expectation-related mechanisms in Alzheimer's disease makes
analgesic therapies less effective. Pain 2006; 121(1-2):133-144.
(47) Andersen F, Engstad T, Straume B, Viitanen M, Halvorsen DS, Hykkerud
S et al. Recruitment methods in Alzheimer's disease research: general
practice versus population based screening by mail. BMC Med Res
Methodol 2010; 10(1):35.
(48) Reisberg B, Gauthier S. Current evidence for subjective cognitive
impairment (SCI) as the pre-mild cognitive impairment (MCI) stage of
subsequently manifest Alzheimer's disease. Int Psychogeriatr 2008; 20(1):1-
16.
(49) Westoby CJ, Mallen CD, Thomas E. Cognitive complaints in a general
population of older adults: prevalence, association with pain and the
influence of concurrent affective disorders. Eur J Pain 2009; 13(9):970-976.
(50) Reisberg B, Ferris SH, Kluger A, Franssen E, Wegiel J, de Leon MJ. Mild
cognitive impairment (MCI): a historical perspective. Int Psychogeriatr
2008; 20(1):18-31.
(51) Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E.
Mild cognitive impairment: clinical characterization and outcome. Arch
Neurol 1999; 56(3):303-308.
(52) Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV et al.
Current concepts in mild cognitive impairment. Arch Neurol 2001;
58(12):1985-1992.
(53) Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO et
al. Mild cognitive impairment--beyond controversies, towards a consensus:
report of the International Working Group on Mild Cognitive Impairment.
J Intern Med 2004; 256(3):240-246.
(54) Stephan BC, Matthews FE, McKeith IG, Bond J, Brayne C. Early cognitive
change in the general population: how do different definitions work? J Am
Geriatr Soc 2007; 55(10):1534-1540.
(55) Jak AJ, Bondi MW, ano-Wood L, Wierenga C, Corey-Bloom J, Salmon DP
et al. Quantification of five neuropsychological approaches to defining mild
cognitive impairment. Am J Geriatr Psychiatry 2009; 17(5):368-375.
(56) Dawe B, Procter A, Philpot M. Concepts of mild memory impairmentin the
elderly and their relationship to dementia: a review. Int J Geriatr Psyciatry
1992;(7):473-479.
(57) Defranceso M, Schocke M, Messner HJ, Deisenhammer EA, Hinterhuber
H, Marksteiner J et al. [Conversion from MCI (Mild Cognitive
Impairment) to Alzheimer's disease: diagnostic options and predictors].
Neuropsychiatr 2010; 24(2):88-98.
(58) Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JP, Mayeux R.
Frequency and course of mild cognitive impairment in a multiethnic
community. Ann Neurol 2008; 63(4):494-506.
(59) Marcos A, Gil P, Barabash A, Rodriguez R, Encinas M, Fernandez C et al.
Neuropsychological markers of progression from mild cognitive
impairment to Alzheimer's disease. Am J Alzheimers Dis Other Demen
2006; 21(3):189-196.
(60) Amieva H, Jacqmin-Gadda H, Orgogozo JM, Le CN, Helmer C, Letenneur
L et al. The 9 year cognitive decline before dementia of the Alzheimer type:
a prospective population-based study. Brain 2005; 128(Pt 5):1093-1101.
(61) Reisberg B, Shulman MB, Torossian C, Leng L, Zhu W. Outcome over
seven years of healthy adults with and without subjective cognitive
impairment. Alzheimers Dement 2010; 6(1):11-24.
(62) Mayeux R. Clinical practice. Early Alzheimer's disease. N Engl J Med
2010; 362(23):2194-2201.
(63) Loewenstein DA, Acevedo A, Agron J, Issacson R, Strauman S, Crocco E et
al. Cognitive profiles in Alzheimer's disease and in mild cognitive
impairment of different etiologies. Dement Geriatr Cogn Disord 2006;
21(5-6):309-315.
(64) Burch EA, Jr., Andrews SR. Comparison of two cognitive rating scales in
medically ill patients. Int J Psychiatry Med 1987; 17(2):193-200.
(65) Roselli F, Tartaglione B, Federico F, Lepore V, Defazio G, Livrea P. Rate
of MMSE score change in Alzheimer's disease: influence of education and
vascular risk factors. Clin Neurol Neurosurg 2009; 111(4):327-330.
(66) Stern RG, Mohs RC, Davidson M, Schmeidler J, Silverman J, Kramer-
Ginsberg E et al. A longitudinal study of Alzheimer's disease:
measurement, rate, and predictors of cognitive deterioration. Am J
Psychiatry 1994; 151(3):390-396.
(67) Suh GH, Ju YS, Yeon BK, Shah A. A longitudinal study of Alzheimer's
disease: rates of cognitive and functional decline. Int J Geriatr Psychiatry
2004; 19(9):817-824.
(68) Kukull WA, Ganguli M. Epidemiology of dementia: concepts and overview.
Neurol Clin 2000; 18(4):923-950.
(69) Erkinjuntti T, Ostbye T, Steenhuis R, Hachinski V. The effect of different
diagnostic criteria on the prevalence of dementia. N Engl J Med 1997;
337(23):1667-1674.
(70) Wancata J, Borjesson-Hanson A, Ostling S, Sjogren K, Skoog I. Diagnostic
criteria influence dementia prevalence. Am J Geriatr Psychiatry 2007;
15(12):1034-1045.
(71) Evans DA, Funkenstein HH, Albert MS, Scherr PA, Cook NR, Chown MJ
et al. Prevalence of Alzheimer's disease in a community population of older
persons. Higher than previously reported. JAMA 1989; 262(18):2551-2556.
(72) Berr C, Wancata J, Ritchie K. Prevalence of dementia in the elderly in
Europe. Eur Neuropsychopharmacol 2005; 15(4):463-471.
(73) Hebert LE, Scherr PA, Beckett LA, Albert MS, Pilgrim DM, Chown MJ et
al. Age-specific incidence of Alzheimer's disease in a community
population. JAMA 1995; 273(17):1354-1359.
(74) Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB
et al. Prevalence of dementia in the United States: the aging, demographics,
and memory study. Neuroepidemiology 2007; 29(1-2):125-132.
(75) Corbo RM, Scacchi R. Apolipoprotein E (APOE) allele distribution in the
world. Is APOE*4 a 'thrifty' allele? Ann Hum Genet 1999; 63(Pt 4):301-
310.
(76) Singh PP, Singh M, Mastana SS. APOE distribution in world populations
with new data from India and the UK. Ann Hum Biol 2006; 33(3):279-308.
(77) Christensen DD, Lin P. Practical treatment strategies for patients with
Alzheimer's disease. J Fam Pract 2007; 56(12 Suppl New):S17-S23.
(78) EU Commission. News Alert: Commission steps up action on Alzheimer´s
disease and other neurodegenerative conditions, 22 July 2009. 2009.
Ref Type: Report
(79) Trojanowski JQ, Arnold SE, Karlawish JH, Brunden K, Cary M,
Davatzikos C et al. Design of comprehensive Alzheimer's disease centers to
address unmet national needs. Alzheimers Dement 2010; 6(2):150-155.
(80) Wimo A, Prince M. World Alzheimer Report 2010 Executive summary. 2-
8. 2010. Alzheimer s Disease International.
Ref Type: Report
(81) Hort J, O'Brien JT, Gainotti G, Pirttila T, Popescu BO, Rektorova I et al.
EFNS guidelines for the diagnosis and management of Alzheimer's disease.
Eur J Neurol 2010; 17(10):1236-1248.
(82) de Toledo Ferraz Alves TC, Ferreira LK, Wajngarten M, Busatto GF.
Cardiac disorders as risk factors for Alzheimer's disease. J Alzheimers Dis
2010; 20(3):749-763.
(83) Rocchi A, Pellegrini S, Siciliano G, Murri L. Causative and susceptibility
genes for Alzheimer's disease: a review. Brain Res Bull 2003; 61(1):1-24.
(84) Tanzi RE. A genetic dichotomy model for the inheritance of Alzheimer's
disease and common age-related disorders. J Clin Invest 1999; 104(9):1175-
1179.
(85) Sando SB, Melquist S, Cannon A, Hutton ML, Sletvold O, Saltvedt I et al.
APOE epsilon 4 lowers age at onset and is a high risk factor for
Alzheimer's disease; a case control study from central Norway. BMC
Neurol 2008; 8:9.
(86) Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC,
Small GW et al. Gene dose of apolipoprotein E type 4 allele and the risk of
Alzheimer's disease in late onset families. Science 1993; 261(5123):921-923.
(87) Arab L, Sabbagh MN. Are certain lifestyle habits associated with lower
Alzheimer's disease risk? J Alzheimers Dis 2010; 20(3):785-794.
(88) Luchsinger JA, Reitz C, Honig LS, Tang MX, Shea S, Mayeux R.
Aggregation of vascular risk factors and risk of incident Alzheimer disease.
Neurology 2005; 65(4):545-551.
(89) Mehta KM, Stewart AL, Langa KM, Yaffe K, Moody-Ayers S, Williams
BA et al. "Below average" self-assessed school performance and
Alzheimer's disease in the Aging, Demographics, and Memory Study.
Alzheimers Dement 2009; 5(5):380-387.
(90) Wilson RS, Hebert LE, Scherr PA, Barnes LL, Mendes de Leon CF, Evans
DA. Educational attainment and cognitive decline in old age. Neurology
2009; 72(5):460-465.
(91) Caamano-Isorna F, Corral M, Montes-Martinez A, Takkouche B.
Education and dementia: a meta-analytic study. Neuroepidemiology 2006;
26(4):226-232.
(92) Hooshmand B, Solomon A, Kareholt I, Leiviska J, Rusanen M, Ahtiluoto S
et al. Homocysteine and holotranscobalamin and the risk of Alzheimer
disease: a longitudinal study. Neurology 2010; 75(16):1408-1414.
(93) Morris JC, Nagy Z. Alzheimer´s disease. In: Esiri M, Lee VMY,
Trojanowski JQ, editors. The Neuropathology of Dementia. Second ed.
2004. 161-206.
(94) Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P,
Cummings J et al. Research criteria for the diagnosis of Alzheimer's
disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 2007;
6(8):734-746.
(95) Karow DS, McEvoy LK, Fennema-Notestine C, Hagler DJ, Jr., Jennings
RG, Brewer JB et al. Relative capability of MR imaging and FDG PET to
depict changes associated with prodromal and early Alzheimer disease.
Radiology 2010; 256(3):932-942.
(96) Kukull WA, Larson EB, Teri L, Bowen J, McCormick W, Pfanschmidt
ML. The Mini-Mental State Examination score and the clinical diagnosis of
dementia. J Clin Epidemiol 1994; 47(9):1061-1067.
(97) Sunderland T, Hill JL, Mellow AM, Lawlor BA, Gundersheimer J,
Newhouse PA et al. Clock drawing in Alzheimer's disease. A novel measure
of dementia severity. J Am Geriatr Soc 1989; 37(8):725-729.
(98) Kirk A. Target symptoms and outcome measures: cognition. Can J Neurol
Sci 2007; 34 Suppl 1:S42-S46.
(99) van Uffelen JG, Chin APM, Klein M, van MW, Hopman-Rock M.
Detection of memory impairment in the general population: screening by
questionnaire and telephone compared to subsequent face-to-face
assessment. Int J Geriatr Psychiatry 2007; 22(3):203-210.
(100) Smeeth L, Fletcher AE, Stirling S, Nunes M, Breeze E, Ng E et al.
Randomised comparison of three methods of administering a screening
questionnaire to elderly people: findings from the MRC trial of the
assessment and management of older people in the community. BMJ 2001;
323(7326):1403-1407.
(101) Naik M, Nygaard HA. Diagnosing dementia -- ICD-10 not so bad after all:
a comparison between dementia criteria according to DSM-IV and ICD-10.
Int J Geriatr Psychiatry 2008; 23(3):279-282.
(102) Bebbington P. Welcome to ICD-10. Soc Psychiatry Psychiatr Epidemiol
1992; 27(6):255-257.
(103) McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM.
Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA
Work Group under the auspices of Department of Health and Human
Services Task Force on Alzheimer's Disease. Neurology 1984; 34(7):939-
944.
(104) Brunnstrom H, Englund E. Clinicopathological concordance in dementia
diagnostics. Am J Geriatr Psychiatry 2009; 17(8):664-670.
(105) Carter MD, Simms GA, Weaver DF. The development of new therapeutics
for Alzheimer's disease. Clin Pharmacol Ther 2010; 88(4):475-486.
(106) Galimberti D, Scarpini E. Treatment of Alzheimer's disease: symptomatic
and disease-modifying approaches. Curr Aging Sci 2010; 3(1):46-56.
(107) Grill JD, Cummings JL. Current therapeutic targets for the treatment of
Alzheimer's disease. Expert Rev Neurother 2010; 10(5):711-728.
(108) Querfurth HW, LaFerla FM. Alzheimer's disease. N Engl J Med 2010;
(109) Merrill DA, Small GW. Prevention in psychiatry: effects of healthy lifestyle
on cognition. Psychiatr Clin North Am 2011; 34(1):249-261.
(110) Flicker L. Life style interventions to reduce the risk of dementia. Maturitas
2009; 63(4):319-322.
(111) Craik FI, Bialystok E, Freedman M. Delaying the onset of Alzheimer
disease: bilingualism as a form of cognitive reserve. Neurology 2010;
75(19):1726-1729.
(112) Stewart R, Xue QL, Masaki K, Petrovitch H, Ross GW, White LR et al.
Change in blood pressure and incident dementia: a 32-year prospective
study. Hypertension 2009; 54(2):233-240.
(113) Ligthart SA, Moll van Charante EP, van Gool WA, Richard E. Treatment
of cardiovascular risk factors to prevent cognitive decline and dementia: a
systematic review. Vasc Health Risk Manag 2010; 6:775-785.
(114) Adlard PA, Perreau VM, Pop V, Cotman CW. Voluntary exercise
decreases amyloid load in a transgenic model of Alzheimer's disease. J
Neurosci 2005; 25(17):4217-4221.
(115) Rogers SL, Friedhoff LT. The efficacy and safety of donepezil in patients
with Alzheimer's disease: results of a US Multicentre, Randomized,
Double-Blind, Placebo-Controlled Trial. The Donepezil Study Group.
Dementia 1996; 7(6):293-303.
(116) Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT. A 24-week,
double-blind, placebo-controlled trial of donepezil in patients with
Alzheimer's disease. Donepezil Study Group. Neurology 1998; 50(1):136-
145.
(117) Arkin SM. Student-led exercise sessions yield significant fitness gains for
Alzheimer's patients. Am J Alzheimers Dis Other Demen 2003; 18(3):159-
170.
(118) Teri L, Gibbons LE, McCurry SM, Logsdon RG, Buchner DM, Barlow
WE et al. Exercise plus behavioral management in patients with Alzheimer
disease: a randomized controlled trial. JAMA 2003; 290(15):2015-2022.
(119) Hogan DB, Bailey P, Black S, Carswell A, Chertkow H, Clarke B et al.
Diagnosis and treatment of dementia: 5. Nonpharmacologic and
pharmacologic therapy for mild to moderate dementia. CMAJ 2008;
179(10):1019-1026.
(120) Tinklenberg JR, Kraemer HC, Yaffe K, Ross L, Sheikh J, Ashford JW et
al. Donepezil treatment and Alzheimer disease: can the results of
randomized clinical trials be applied to Alzheimer disease patients in
clinical practice? Am J Geriatr Psychiatry 2007; 15(11):953-960.
(121) Schneider LS, Olin JT, Lyness SA, Chui HC. Eligibility of Alzheimer's
disease clinic patients for clinical trials. J Am Geriatr Soc 1997; 45(8):923-
928.
(122) Holmes C, Burns A, Passmore P, Forsyth D, Wilkinson D. AD2000: design
and conclusions. Lancet 2004; 364(9441):1213-1214.
(123) Hansen RA, Gartlehner G, Lohr KN, Kaufer DI. Functional outcomes of
drug treatment in Alzheimer's disease: A systematic review and meta-
analysis. Drugs Aging 2007; 24(2):155-167.
(124) Ito K, Ahadieh S, Corrigan B, French J, Fullerton T, Tensfeldt T. Disease
progression meta-analysis model in Alzheimer's disease. Alzheimers
Dement 2010; 6(1):39-53.
(125) Requena C, Maestu F, Campo P, Fernandez A, Ortiz T. Effects of
cholinergic drugs and cognitive training on dementia: 2-year follow-up.
Dement Geriatr Cogn Disord 2006; 22(4):339-345.
(126) Roberts RO, Geda YE, Knopman DS, Cha RH, Pankratz VS, Boeve BF et
al. The Mayo Clinic Study of Aging: design and sampling, participation,
baseline measures and sample characteristics. Neuroepidemiology 2008;
30(1):58-69.
(127) Green LW, Glasgow RE. Evaluating the relevance, generalization, and
applicability of research: issues in external validation and translation
methodology. Eval Health Prof 2006; 29(1):126-153.
(128) Doraiswamy PM, Leon J, Cummings JL, Marin D, Neumann PJ.
Prevalence and impact of medical comorbidity in Alzheimer's disease. J
Gerontol A Biol Sci Med Sci 2002; 57(3):M173-M177.
(129) Lyketsos CG, Toone L, Tschanz J, Rabins PV, Steinberg M, Onyike CU et
al. Population-based study of medical comorbidity in early dementia and
"cognitive impairment, no dementia (CIND)": association with functional
and cognitive impairment: The Cache County Study. Am J Geriatr
Psychiatry 2005; 13(8):656-664.
(130) Malone DC, McLaughlin TP, Wahl PM, Leibman C, Arrighi HM, Cziraky
MJ et al. Burden of Alzheimer's disease and association with negative
health outcomes. Am J Manag Care 2009; 15(8):481-488.
(131) Deschenes CL, McCurry SM. Current treatments for sleep disturbances in
individuals with dementia. Curr Psychiatry Rep 2009; 11(1):20-26.
(132) Konishi K, Hori K, Uchida H, Watanabe K, Tominaga I, Kimura M et al.
Adverse effects of anticholinergic activity on cognitive functions in
Alzheimer's disease. Psychogeriatrics 2010; 10(1):34-38.
(133) Joseph J, Svartberg J, Njolstad I, Schirmer H. Risk factors for type 2
diabetes in groups stratified according to metabolic syndrome: a 10-year
follow-up of The Tromso Study. Eur J Epidemiol 2010.
(134) Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association
between midlife blood pressure levels and late-life cognitive function. The
Honolulu-Asia Aging Study. JAMA 1995; 274(23):1846-1851.
(135) Breteler MM. Vascular risk factors for Alzheimer's disease: an
epidemiologic perspective. Neurobiol Aging 2000; 21(2):153-160.
(136) Chui HC, Zarow C, Mack WJ, Ellis WG, Zheng L, Jagust WJ et al.
Cognitive impact of subcortical vascular and Alzheimer's disease
pathology. Ann Neurol 2006; 60(6):677-687.
(137) Nagai M, Hoshide S, Kario K. Hypertension and dementia. Am J
Hypertens 2010; 23(2):116-124.
(138) Staessen JA, Richart T, Birkenhager WH. Less atherosclerosis and lower
blood pressure for a meaningful life perspective with more brain.
Hypertension 2007; 49(3):389-400.
(139) Mielke MM, Rosenberg PB, Tschanz J, Cook L, Corcoran C, Hayden KM
et al. Vascular factors predict rate of progression in Alzheimer disease.
Neurology 2007; 69(19):1850-1858.
(140) Deschaintre Y, Richard F, Leys D, Pasquier F. Treatment of vascular risk
factors is associated with slower decline in Alzheimer disease. Neurology
2009; 73(9):674-680.
(141) Malone DC, McLaughlin TP, Wahl PM, Leibman C, Arrighi HM, Cziraky
MJ et al. Burden of Alzheimer's disease and association with negative
health outcomes. Am J Manag Care 2009; 15(8):481-488.
(142) Guo Z, Viitanen M, Fratiglioni L, Winblad B. Low blood pressure and
dementia in elderly people: the Kungsholmen project. BMJ 1996;
312(7034):805-808.
(143) Moretti R, Torre P, Antonello RM, Manganaro D, Vilotti C, Pizzolato G.
Risk factors for vascular dementia: hypotension as a key point. Vasc
Health Risk Manag 2008; 4(2):395-402.
(144) Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG et
al. The clinical course of advanced dementia. N Engl J Med 2009;
361(16):1529-1538.
(145) Carriere I, Fourrier-Reglat A, Dartigues JF, Rouaud O, Pasquier F,
Ritchie K et al. Drugs with anticholinergic properties, cognitive decline,
and dementia in an elderly general population: the 3-city study. Arch
Intern Med 2009; 169(14):1317-1324.
(146) Jessen F, Kaduszkiewicz H, Daerr M, Bickel H, Pentzek M, Riedel-Heller S
et al. Anticholinergic drug use and risk for dementia: target for dementia
prevention. Eur Arch Psychiatry Clin Neurosci 2010; 260 Suppl 2:S111-
S115.
(147) Brauner DJ, Muir JC, Sachs GA. Treating nondementia illnesses in
patients with dementia. JAMA 2000; 283(24):3230-3235.
(148) Tjia J, Rothman MR, Kiely DK, Shaffer ML, Holmes HM, Sachs GA et al.
Daily medication use in nursing home residents with advanced dementia. J
Am Geriatr Soc 2010; 58(5):880-888.
(149) Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC.
Explicit criteria for determining inappropriate medication use in nursing
home residents. UCLA Division of Geriatric Medicine. Arch Intern Med
1991; 151(9):1825-1832.
(150) Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH.
Updating the Beers criteria for potentially inappropriate medication use in
older adults: results of a US consensus panel of experts. Arch Intern Med
2003; 163(22):2716-2724.
(151) Rognstad S, Brekke M, Fetveit A, Spigset O, Wyller TB, Straand J. The
Norwegian General Practice (NORGEP) criteria for assessing potentially
inappropriate prescriptions to elderly patients. A modified Delphi study.
Scand J Prim Health Care 2009; 27(3):153-159.
(152) Levy HB, Marcus EL, Christen C. Beyond the beers criteria: A
comparative overview of explicit criteria. Ann Pharmacother 2010;
44(12):1968-1975.
(153) Barnett K, McCowan C, Evans JM, Gillespie ND, Davey PG, Fahey T.
Prevalence and outcomes of use of potentially inappropriate medicines in
older people: cohort study stratified by residence in nursing home or in the
community. Qual Saf Health Care 2011; 20(3):275-281.
(154) Uusvaara J, Pitkala KH, Kautiainen H, Tilvis RS, Strandberg TE.
Association of anticholinergic drugs with hospitalization and mortality
among older cardiovascular patients: A prospective study. Drugs Aging
2011; 28(2):131-138.
(155) Crews WD, Jr., Harrison DW, Keiser AM, Kunze CM. The memory
screening outreach program: findings from a large community-based
sample of middle-aged and older adults. J Am Geriatr Soc 2009;
57(9):1697-1703.
(156) Lawrence JM, Davidoff DA, Katt-Lloyd D, Connell A, Berlow YA, Savoie
JA. Is large-scale community memory screening feasible? Experience from
a regional memory-screening day. J Am Geriatr Soc 2003; 51(8):1072-1078.
(157) Vernooij-Dassen MJ, Moniz-Cook ED, Woods RT, De LJ, Leuschner A,
Zanetti O et al. Factors affecting timely recognition and diagnosis of
dementia across Europe: from awareness to stigma. Int J Geriatr
Psychiatry 2005; 20(4):377-386.
(158) Woods RT, Moniz-Cook E, Iliffe S, Campion P, Vernooij-Dassen M,
Zanetti O et al. Dementia: issues in early recognition and intervention in
primary care. J R Soc Med 2003; 96(7):320-324.
(159) Lolk A, Nielsen H, Andersen K, Andersen J, Kragh-Sorensen P. CAMCOG
as a screening instrument for dementia: the Odense study. Cambridge
Cognitive Examination. Acta Psychiatr Scand 2000; 102(5):331-335.
(160) Strawbridge WJ, Shema SJ, Balfour JL, Higby HR, Kaplan GA.
Antecedents of frailty over three decades in an older cohort. J Gerontol B
Psychol Sci Soc Sci 1998; 53(1):S9-16.
(161) Stone SP, Ali B, Auberleek I, Thompsell A, Young A. The Barthel index in
clinical practice: use on a rehabilitation ward for elderly people. J R Coll
Physicians Lond 1994; 28(5):419-423.
(162) Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA,
Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of
psychopathology in dementia. Neurology 1994; 44(12):2308-2314.
(163) Dratcu L, da Costa RL, Calil HM. Depression assessment in Brazil. The
first application of the Montgomery-Asberg Depression Rating Scale. Br J
Psychiatry 1987; 150:797-800.
(164) Jorm AF, Jacomb PA. The Informant Questionnaire on Cognitive Decline
in the Elderly (IQCODE): socio-demographic correlates, reliability,
validity and some norms. Psychol Med 1989; 19(4):1015-1022.
(165) Reinders A, Reggiori F, Shennan AH. Validation of the DINAMAP
ProCare blood pressure device according to the international protocol in
an adult population. Blood Press Monit 2006; 11(5):293-296.
(166) Whitehouse PJ. Future prospects for Alzheimer's disease therapy: ethical
and policy issues for the international community. Acta Neurol Scand
Suppl 1996; 165:145-149.
(167) Doody RS, Dunn JK, Clark CM, Farlow M, Foster NL, Liao T et al.
Chronic donepezil treatment is associated with slowed cognitive decline in
Alzheimer's disease. Dement Geriatr Cogn Disord 2001; 12(4):295-300.
(168) Kawas CH, Clark CM, Farlow MR, Knopman DS, Marson D, Morris JC et
al. Clinical trials in Alzheimer disease: debate on the use of placebo
controls. Alzheimer Dis Assoc Disord 1999; 13(3):124-129.
(169) Drazen JM, Van der Weyden MB, Sahni P, Rosenberg J, Marusic A, Laine
C et al. Uniform format for disclosure of competing interests in ICMJE
journals. N Engl J Med 2009; 361(19):1896-1897.
(170) Moher D, Schulz KF, Altman D. The CONSORT Statement: revised
recommendations for improving the quality of reports of parallel-group
randomized trials 2001. Explore (NY) 2005; 1(1):40-45.
(171) Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic
risk scale and anticholinergic adverse effects in older persons. Arch Intern
Med 2008; 168(5):508-513.
(172) Carneiro AV, Costa J. Cardiac disease outcomes in clinical trials. Rev Port
Cardiol 2002; 21(11):1349-1360.
(173) Hebert LE, Bienias JL, Aggarwal NT, Wilson RS, Bennett DA, Shah RC et
al. Change in risk of Alzheimer disease over time. Neurology 2010;
75(9):786-791.
(174) Vina J, Lloret A. Why women have more Alzheimer's disease than men:
gender and mitochondrial toxicity of amyloid-beta peptide. J Alzheimers
Dis 2010; 20 Suppl 2:S527-S533.
(175) Norwegian Bank of Statistics. Public health statistics. 2010.
Ref Type: Report
(176) Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life
on risk of incident Alzheimer disease and mild cognitive impairment in
community-dwelling older persons. Arch Gen Psychiatry 2010; 67(3):304-
310.
(177) Valcour VG, Masaki KH, Curb JD, Blanchette PL. The detection of
dementia in the primary care setting. Arch Intern Med 2000; 160(19):2964-
2968.
(178) Lopponen M, Raiha I, Isoaho R, Vahlberg T, Kivela SL. Diagnosing
cognitive impairment and dementia in primary health care -- a more active
approach is needed. Age Ageing 2003; 32(6):606-612.
(179) Stephan BC, Kurth T, Matthews FE, Brayne C, Dufouil C. Dementia risk
prediction in the population: are screening models accurate? Nat Rev
Neurol 2010; 6(6):318-326.
(180) Caughey GE, Vitry AI, Gilbert AL, Roughead EE. Prevalence of
comorbidity of chronic diseases in Australia. BMC Public Health 2008;
8:221.
(181) Lau DT, Mercaldo ND, Harris AT, Trittschuh E, Shega J, Weintraub S.
Polypharmacy and potentially inappropriate medication use among
community-dwelling elders with dementia. Alzheimer Dis Assoc Disord
2010; 24(1):56-63.
(182) Campbell N, Boustani M, Limbil T, Ott C, Fox C, Maidment I et al. The
cognitive impact of anticholinergics: a clinical review. Clin Interv Aging
2009; 4:225-233.
(183) Malone DC, McLaughlin TP, Wahl PM, Leibman C, Arrighi HM, Cziraky
MJ et al. Burden of Alzheimer's disease and association with negative
health outcomes. Am J Manag Care 2009; 15(8):481-488.
(184) Schubert CC, Boustani M, Callahan CM, Perkins AJ, Carney CP, Fox C et
al. Comorbidity profile of dementia patients in primary care: are they
sicker? J Am Geriatr Soc 2006; 54(1):104-109.
(185) Zekry D, Herrmann FR, Grandjean R, Meynet MP, Michel JP, Gold G et
al. Demented versus non-demented very old inpatients: the same
comorbidities but poorer functional and nutritional status. Age Ageing
2008; 37(1):83-89.
(186) Polidori MC, Mariani E, Mecocci P, Nelles G. Congestive heart failure and
Alzheimer's disease. Neurol Res 2006; 28(6):588-594.
(187) Guo Z, Viitanen M, Fratiglioni L, Winblad B. Low blood pressure and
dementia in elderly people: the Kungsholmen project. BMJ 1996;
312(7034):805-808.
(188) Ito K, Ahadieh S, Corrigan B, French J, Fullerton T, Tensfeldt T. Disease
progression meta-analysis model in Alzheimer's disease. Alzheimers
Dement 2010; 6(1):39-53.
(189) Matsuda O. Cognitive stimulation therapy for Alzheimer's disease: the
effect of cognitive stimulation therapy on the progression of mild
Alzheimer's disease in patients treated with donepezil. Int Psychogeriatr
2007; 19(2):241-252.
(190) McCarney R, Warner J, Iliffe S, van HR, Griffin M, Fisher P. The
Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol
2007; 7:30.
(191) Waldron CA, Gallacher J, van der WT, Newcombe R, Elwyn G. The effect
of different cardiovascular risk presentation formats on intentions,
understanding and emotional affect: a randomised controlled trial using a
web-based risk formatter (protocol). BMC Med Inform Decis Mak 2010;
10:41.
(192) Kong J, Kaptchuk TJ, Polich G, Kirsch I, Vangel M, Zyloney C et al.
Expectancy and treatment interactions: a dissociation between
acupuncture analgesia and expectancy evoked placebo analgesia.
Neuroimage 2009; 45(3):940-949.
(193) Oken BS, Flegal K, Zajdel D, Kishiyama S, Haas M, Peters D. Expectancy
effect: impact of pill administration on cognitive performance in healthy
seniors. J Clin Exp Neuropsychol 2008; 30(1):7-17.
(194) Rogers SL, Friedhoff LT. The efficacy and safety of donepezil in patients
with Alzheimer's disease: results of a US Multicentre, Randomized,
Double-Blind, Placebo-Controlled Trial. The Donepezil Study Group.
Dementia 1996; 7(6):293-303.
(195) Jean L, Bergeron ME, Thivierge S, Simard M. Cognitive intervention
programs for individuals with mild cognitive impairment: systematic
review of the literature. Am J Geriatr Psychiatry 2010; 18(4):281-296.
(196) Sevigny JJ, Peng Y, Liu L, Lines CR. Item analysis of ADAS-Cog: effect of
baseline cognitive impairment in a clinical AD trial. Am J Alzheimers Dis
Other Demen 2010; 25(2):119-124.
(197) Ravin JG, Higginbotham EJ. The story of Percy Lavon Julian: against all
odds. Arch Ophthalmol 2009; 127(5):690-692.
(198) Michael E.Scharf. Neurological Effects of Insecticides. Encyclopedia of Pest
Management. 2003.
(199) Pepeu G, Giovannini MG. Cholinesterase inhibitors and beyond. Curr
Alzheimer Res 2009; 6(2):86-96.
16. Appendix
Appendix 1 Mean arterial pressure (MAP)
MAP = (Diastolic blood pressure x 2) + Systolic blood pressure
Appendix 2
The history of cholinesterase inhibitors (ChEI)
The comprehensive neurological and toxicological effects of ChEIs have gradually been
revealed in biological and medical literature over approximately 135 years, beginning
with the discovery of physostigmine. The natural source of physostigmine was the calara
bean from tropical West Africa which was brought to England in 1875. The effect was
first described in the ophthalmology literature by Laqueur in 1876 and in 1936 the drug
was synthesised by Percy Lavon Julian197. ChEIs play still a significant role in modern
medicine as an important therapeutic option in ophthalmology and in the treatment of
myasthenia gravis.
The history of nerve gases began on 23 December, 1936, when Gerhard Schrader first
prepared tabun which exhibits a strong non-competitive inhibition of acetyl
cholinesterase. He continued to prepare new forms of tabun and observed the toxic effect
of vaporised tabun on him self and his laboratory assistant. In 1939 a pilot factory for
vaporised tabun production was set up at Munster-Lager, and the history of Nazi gas
chambers was initiated (Paxman J et al: A higher Form of Killing: The Secret Story of
Chemical and Biological Warfare, 1982).
The vast majority of pesticides and herbicides have their main impact on
neurotransmission. Some of the most neurotoxic chemicals, such as organophosphate and
carbamate, are highly potent non-competitive ChEIs198 and may produce serious toxic
reactions in mammals.
Most health professionals are well aware of the biological mechanisms behind ChEIs,
their toxicity and their antidotes. During my own military service in the medical corps of
the Norwegian Air Force I gave lectures about the disaster caused by chemical weapons
including nerve gases, many of which have cholinesterase inhibition properties. Later on
as a general practitioner, I taught farmers about the risks of pesticides, herbicides and
insecticides for the farmer him/herself, the environment and the consumers.
This brief review summarises the well-known physiological effect and toxicity of ChEIs.
The possibility of adverse reactions to any chemicals with a ChEI effect must always be
considered. Their conflicting and dramatic history in combination with their potential
impact on vital neural and neuromuscular transmission in any creature makes the
preparing of new ChEI derivatives for neurological purposes an ethical question,
especially when it comes to "improving memory and learning in healthy subjects"199 and
in studying and treating individuals with reduced consent competence.
ISBN xxx-xx-xxxx-xxx-x
Source: http://dsnn.no/files/dokumentbase/hovedstudien/thesis_dsnn.pdf
Contents lists available at Energy Storage Materials journal homepage: Latest development of nanostructured Si/C materials for lithium anodestudies and applications Miao Zhang Tengfei Zhang , Yanfeng Ma Yongsheng Chen a Centre for Nanoscale Science and Technology, Collaborative Innovation Center of Chemical Science and Engineering (Tianjin), School of Materials Scienceand Engineering, Nankai University, Tianjin 300071, Chinab Key Laboratory of Functional Polymer Materials and the Institute of Polymer Chemistry, College of Chemistry, Nankai University, Tianjin 300071, China
BLUE Review Issue 6 – 2008 • November/December Blue Review going paperless in 2009 As a part of our corporate "Blue Goes Green" initiative, To sign up for Blue Review via e-mail, click the Update we are collecting e-mail addresses of the more than Your Contact Information button at bcbsnm.com 10,500 contracting providers in our networks.* We will