Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Uniport.edu.ng
UNIVERSITY OF PORT HARCOURT
LIVING WITH DIABETES IN NIGERIA
The Care, Cure & Prevention
An Inaugural Lecture
PROFESSOR SUNDAY CHINENYE
MBBS (Ibadan),
FWACP (West African College of Physicians),
FACE (American College of Endocrinology),
FNSEM (Nigerian Society of Endocrinology)
Department of Medicine, Faculty of Clinical Sciences,
College of Health Sciences
INAUGURAL LECTURE SERIES
OCTOBER 15TH, 2015
Dedication
This Lecture is first and foremost dedicated to my Late mother who lived very well with diabetes, for about four decades and passed on at the age of 87 years; and to over five million Nigerians living with diabetes mellitus who strive every day of their life to remain healthy, resilient and adherent to treatment.
My special gratitude to my teachers and mentors, most especially Professor C.O. Anah who has remained a father indeed (he guided me in choosing the title, read and edited every section); to Professors O.J. Odia, A.E Ihekwaba, A.C Onwuchekwa, F.S Wokoma and Dr. Mrs. Ngozi Ordu. To all my patients whose treatment and response led to the conceptualization of this lecture; including the experience of serving the Diabetes Association of Nigeria. Special thanks also to my colleagues, resident doctors and medical students for the team work, collaborations, communications, creativity and critical thinking in learning and discharge of our duties. Thanks to my darling wife for her love, encouragements and constructive criticisms. I appreciate my children (my special brothers and sisters) and all other family & community members. All Glory to Almighty God for the vision and wisdom in all my life endeavours.
Table of Content
1. Dedication .ii 2. Acknowledgements .iii 3. Acronyms .v 4. Preamble .1 5. The title of the Lecture .1 6. Endocrinology: Historical Perspectives .2 7. Diabetes Mellitus: Definitions and Historical Perspectives .6 8. Epidemiology of diabetes in Nigeria (Distribution &
Determinants) .10
9. Classification of diabetes mellitus.11 10. Causes of Diabetes .14 11. The Natural History (progression) of Diabetes .14 12. Diagnosis of Diabetes Mellitus: Screening tests and
Confirmation .17 12.1 Dealing with a positive result of diabetes .18
13. Diabetes in Nigeria: Features and Manifestations .18 14. Diabetes Complications .21 15. Burden & Status of Diabetes Care in Nigeria .23
Landmark Studies
16. The Concept of Living Well with a Chronic Disease
17. Diabetes Care and Targets of Control .40 18. Policy and Strategies to achieve Diabetes Care in Nigeria .57
18.1 Challenges to Diabetes Care in Nigeria .57 18.2 Proposed Model for Diabetes Care in Nigeria .59
19. Ways to support Nigerians living with Diabetes .62 20. Prevention of Diabetes .63 21. Milestones in Diabetes Research and Potential for Cure .67 22. Summary of my Academic/Professional contributions .74 23. Concluding Remarks .77
23.1 Summary of Recommendations .77 23.2 Diabetes Epilogue .79
24. References .80
25. Citation .85
ACRONYMS
ADA - American Diabetes Association
AHS - Abuja Heart Study
BMI – Body Mass Index
CBOs - Community Based Organizations
CCM - Chronic Disease Care Model
CHD – Coronary Heart Disease
CHF - Congestive Heart Failure
CVD – Cardiovascular Disease
CKD - Chronic Kidney Disease
CSOs -Civil Society Organizations
CSI - Continuous Subcutaneous Infusion
C/S – Caeserian Section
DAN – Diabetes Association of Nigeria
DM – Diabetes Mellitus
DFU - DM Foot Ulcers
DPP-4 - Dipeptidyl petidase-4
DPN - Diabetic Peripheral Neuropathy
DKA - Diabetic Ketoacidosis
DRS - Diabetes Retinopathy Study
DSME - Diabetes Self-Management Education
ECG - Electrocardiogram
ED – Erectile Dysfunction
ESRD - End-Stage Renal Disease
FBOs - Faith Based Organization
FBG – Fasting Blood Glucose
FBS – Fasting Blood Sugar
FDA – Food and Drug Administration, USA
FGN – Federal Government of Nigeria
FPG – Fasting Plasma Glucose
GDM - Gestational Diabetes or Pregnancy-induced Diabetes
GIP - Gastric Inhibitory Peptide (aka glucose-dependent Insulinotropic
peptide)
GLP-1- Glucagon Like Peptides
2-HrPP -2 Hour Post-Prandial
HbA1c - Glycosylated Haemoglobin
HDL-C – High Density Cholesterol
HE -HyperGlycaemic Emergencies HHS – Hyperosmolar Hyperglycaemic State ICCCF -Innovative Care for Chronic Conditions Framework IDF - International Diabetes Federation IFG - Impaired Fasting Glucose IGT - Impaired glucose tolerance LDL-C- Low Density Cholesterol LOPS - Loss of Peripheral Sensation MDG(s) - Millennium Development Goal (s) MNT - Medical Nutrition Therapy MODY - Maturity-Onset Diabetes in Young MRDM - Malnutrition Related Diabetes Mellitus NAFDAC- National Food Drug Administration and Control NCD(s) - Non-communicable Disease(s) NDLEA -National Drug Law Enforcement Agency NGOs - Non-Governmental Organizations NHIS – National Health Insurance Scheme NICE – National Institute of Clinical Excellence NPDR - Nonproliferative Diabetes Retinopathy NPI - National Programme on Immunization OGTT - Oral Glucose Tolerance Test PAD - Peripheral Arterial Disease PATH - Program for Appropriate Technology in Health PDR - Proliferative Diabetic Retinopathy PLWD – People Living With Diabetes SMBG - Self-Monitoring of Blood Glucose TB - Tuberculosis TCHOL – Total Cholesterol TG- Triglycerides TDHS - Tropical Hand Ulcer TZD - Thiazolidinediones UKPDS - UK Prospective Diabetes Study WHO- World Health Organization WHO FCTC - WHO Framework Convention on Tobacco Control WHA - World Health Assembly
PREAMBLE
Vice Chancellor Sir, I wish to express my gratitude for this opportunity
to deliver the 126thInaugural Lecture of the University of Port Harcourt,
from the Department of Medicine (commonly called Internal Medicine,
the core of medicine).
A historical appraisal of our inaugural lecture series show that Internal
medicine has produced three inaugural lectures as tabulated below:
Table 1:
Topic
Lecturer
Specialty
You and Your Prof. C.O. Anah
Death: Prof. O.J. Odia
The Heart of the Matter
Eat Right, Live Prof. A.E Ihekwaba
Gastroenterology
Right that your Liver
Right
This inaugural lecture today is the 4th from Internal Medicine and the 1st
from the specialty of Endocrinology.
THE TITLE OF THE LECTURE
Vice Chancellor Sir, in a nutshell this title was chosen to bring to the
fore this 21st century pandemic –
Diabetes, which has become a health
scourge in Nigeria. This is to enable our leaders, health decision
makers, academicians, students, patients, relatives and the general
public to be well informed about diabetes in the Nigerian setting as a
basis for good care and health policy formulation to enhance Care and
Support.
The emphasis on Nigeria is deliberate.
By World Health Organization (WHO)/IDF statistics, Nigeria has the
highest number of diabetics in Sub-Saharan Africa with over 5 million
Nigerians living with diabetes.
Therefore, diabetes should be of paramount importance to all Nigerians.
Though diabetes is an ancient and world-wide disease and the protocol
of care is universal, socioeconomic and cultural behaviours to the
disease, its medications, care, support and diet differ from country to
country and these do affect treatment outcomes.
My experiences as Vice President, Diabetes Association of Nigeria
[DAN] and subsequently National President for two tenures each,
coupled with several landmark Nigerian studies we conducted exposed
me to the multi-faceted nature of diabetes in Nigeria. These Nigerian
experiences are what I intend to share with you in this 126thinaugural
lecture today.
Furthermore, local staple foods recommended for diabetics in Europe
and North America are also quite different from those in African
populations. Similarly sociocultural attitudes and illness behaviour
differ from culture to culture, even within Nigeria.
The word "LIVING" in the title was also chosen to emphasize the fact
that diabetes is no longer a death sentence because people can and do
live through life with diabetes and longevity may be unaffected. The
key to living well with diabetes is proper management anchored on
"well informed self-care practices".
Deliberate effort has been made to limit the use of medical terms as
much as possible. Where unavoidable, my apologies, and such medical
term is followed by simplified explanatory clause.
ENDOCRINOLOGY: HISTORICAL PERSPECTIVES
Endocrinology is the study of the endocrine glands and responses to
their secretions, chemical integration and communication within the
body.
Endocrinology is as old as creation because the Almighty God as the
first endocrinologist created Eve out of Adam (Genesis 2:21-22)

through the process of differentiating and putting into compartments their hormonal organs and its secretions.
Fig. 1: The Human Endocrine System

Genitalia
(Anatomic sex)
Genetic sex determines gonadal sex and gonadal sex in turn controls
development of anatomical sex through hormonal secretions.
Time of Sexual Differentiation = 7 – 9 week of gestation
Fig. 2: Human Endocrine Glands
Biblically also, Eunuchs (castrated men) guarded the women's quarters
of Hebrew Kings and Princes (Esther 1:10), probably because they were
incapable of reproduction and could possibly not sexually harass those
beautiful Queens!!!
Professor Charles Brown-Sequard is reputed to be the father of modern endocrinology following the Seminal work he delivered in 1889 to the Societe de Biologie in Paris… titled "Chemical messengers secreted into the blood to exert systemic effects". Born in the British Island of
Mauritius, his father was a sea captain from Philadelphia and his mother was French (Wilson JD 2005).
In 1903 Ernest Starling chose the term "Hormone" to describe all chemical messengers. By this time it was clear that hormones influence almost every function in the body.
The term "hormone" is derived from a Greek phrase meaning "to set in motion, to excite or to arouse" and aptly describes the dynamic actions of hormones as they elicit cellular responses and regulate physiologic processes through feedback mechanisms (Jameson et al 2012).
Hormone development involves a series of stages namely: 1. Identification of the tissue organ that produces the hormone. 2. Development of bioassay methods to identify the hormone. 3. Preparation of active extracts that can be purified using the relevant
4. Isolation, identification of structure and synthesis of the hormone. Three periods can be distinguished in the historical development of endocrinology namely the Descriptive period, the period of Analytical endocrinology and the third, Contemporary period, that of Synthetic endocrinology. Each of these periods is based on certain special directive lines of scientific research, but although they follow each other chronologically in their beginnings there is much overlapping. For instance, even in our times research on the lines of the descriptive period is still being pursued. In endocrinology, the scientific reasoning is that every single tissue and in general, every separate cell of the body secretes certain products (hormones) which are poured into the blood current, and which influence every other cell. In this way solidarity is established among all the cells of the body by means other than the nervous or immune systems.
Endocrine science continues to be one of the most dynamic disciplines of medical science; and endocrinology is the most quantitative of the clinical specialties. There is probably no arena of medicine in which collaboration between the clinical and basic sciences has been more rewarding as endocrinology.
Probably the most important impact endocrinology has had is in scientifically designed treatments such as insulin and oral contraceptives, two of the very important therapeutic advances of the twentieth century.
The fact that many advances in Endocrinology have been recognized by the scientific world through award of Nobel Prizes is a source of pride.
Today, endocrinology involves neural science, immunology, genetics,
cell and molecular biology as much as it deals with hormones per se.
Pattern of Endocrine Disorders
The specialty of endocrinology deals with the diagnosis and treatment
of diverse range of hormonal and metabolic disorders. It encompasses a
wide variety of conditions ranging from the most common, Diabetes
Mellitus, (the subject of this lecture), thyroid diseases and to those that
are rare but eminently treatable e.g. pituitary tumours.
Most endocrine conditions are CHRONIC (i.e. slow in progression,
requiring long-term and often life-long treatment).
There is a strong scientific evidence base for the treatment of disorders
encountered within the specialty of endocrinology. Delayed, inadequate
or inappropriate Care leads to poor health, reduced life-span and
increased burden on the health service.
DIABETES MELLITUS: DEFINITIONS AND HISTORICAL
PERSPECTIVES
Definition:
Diabetes is a "chronic" condition that occurs when the body cannot
produce enough or effectively use insulin [IDF Diabetes Atlas, 6th
edition2013].
Insulin is a hormone (chemical messenger) produced by the pancreas
that allows glucose (and other nutrients) from food to enter the body's
cells where it is converted into energy needed by muscles and tissues to
function.
As a result, a person with diabetes does not utilize glucose (and other
nutrients) properly, and glucose stays circulating in the blood
(hyperglycaemia) damaging tissues over time. This damage leads to
life-threatening health complications.
Technically, diabetes is defined as a syndrome of multiple aetiology
(inherited or acquired) characterized by chronic Hyperglycaemia with
disturbances of carbohydrate, fat and protein metabolism due to
deficient action of insulin on target tissues (resulting from inadequate
insulin secretion, insulin resistance or both)WHO, 1999 .
Diabetes mellitus, often simply referred to as Diabetes, is a disorder of
the very engine of life because when the body cells cannot utilize
glucose, a number of vital mechanisms will breakdown with life-
threatening consequences. This high blood sugar produces the classical
symptoms of polyuria (frequent urination), polydipsia (increased thirst)
and polyphagia (increased hunger).

Pancreas
Fig. 3: Picture of the pancreas
Source: Picture of the Pancrease, www.webmd.com(c)2009webMD,LLC.
Front view of the Pancreas
- The pancreas is about 6 inches long (15cm)
- Sits across the back of the abdomen behind the stomach
- The head is on the right side of the abdomen
- The head is connected to the duodenum (the 1st section of the small
intestine) through a small tube called the pancreatic duct.
- The narrow end of the pancreas, called the tail, extends to the left
side of the body.
- The tail end habours the clusters of cells that produce insulin.

Fig. 4: The Pancreas and its Functions
Historically, diabetes is an ancient disease with descriptions dating back
to 3000 years ago in ancient Egyptian writings.
Differences in the clinical features of types 1 and 2 were described by
Charuka & Susruta in India about 400BC.
Diabetes (from ‘diabe' meaning ‘siphon') and mellitus (‘melli' means
‘honey or sweet'), were terms first used by Aretaeus of Cappadocia in
the 2nd century AD (Chinenye et al. Lecture Notes and Essays in
Internal Medicine vol. 1, 2013).
Diabetes Mellitus was a death sentence in the ancient era. Hippocrates,
the father of modern medicine, made not much mention of it because he
felt the disease was incurable. Aretaeus did attempt to treat it but could
not give a prognosis; he commented that "life (with diabetes) is short,
disgusting and painful".

Diabetes mellitus, a non-communicable disease is certainly a scourge in
this millennium. The discovery of insulin by Frederick Banting &
Charles Best in collaboration with two other researchers in 1921 was a
significant landmark in the management of diabetes.
Prior to discovery of insulin in 1921, diabetes was a dreaded disease
and planning for the future was unimportant.
The Islet of Langerhans
These are groups of pancreatic cells secreting insulin and glucagon first
described in 1869 by Paul Langerhans, a German pathologist.
Fig. 5: The Pancreas & Islet of Langerhans
Fig. 6: Islet cell in Health and Disease
EPIDEMIOLOGY OF DIABETES IN NIGERIA
(DISTRIBUTION & DETERMINANTS)
Mirroring the global increase in diabetes prevalence, Nigeria has been
recording rising diabetes prevalence since 1960. See table below
(Chinenye et al. Diabetes Advocacy and Care in Nigeria 2014):
Table 2: DM-Global and Nigerian Landscape
Global Diabetes Landscape
1994 2000 2007 2011 2013 2035
Global DM
(millions)
Nigerian Diabetes Landscape
FMOH PortHarcourt
Prevalence
(%)
Current estimates of DM prevalence are 1-2% in rural adults and 6-10% in
urban dwelling adults in Nigeria. This translates to at least 5 million people living with DM, a
large proportion of which are undiagnosed.
Source: Chinenye et al. Diabetes Advocacy and Care in Nigeria 2014
As Nigeria modernizes and copies western lifestyles, the disease
frequency is on the increase among top executives, politicians,
academicians, civil servants, farmers, traditional rulers, traders,
businessmen, teachers, students, pupils, pre-school children and
pregnant women.
It is obvious that diabetes mellitus touches almost every family and
constitutes a drain on the economy and social life of sufferers and their
families.
CLASSIFICATION OF DIABETES MELLITUS
The classification of Diabetes according to the World Health includes
four classes:
1. Type-1 Diabetes: Usually first diagnosed in children and young
adults, although it can occur at any age. In Type-1 diabetes, the immune system abnormally attacks and destroys the insulin producing beta cells of the pancreas. There is beta cell loss leading to complete insulin deficiency. Thus, it is termed an autoimmune disease where there are anti-insulin or anti-islet cell antibodies present in the blood. The destruction may take time but the onset of the disease is rapid and may occur over a few days to weeks. Type 1 diabetes always require insulin treatment and will not respond to oral glucose-lowering drugs. It accounts for about 3-5% in Nigeria (Chinenye et al. National Clinical Practice Guideline for Diabetes Management in Nigeria 2013; 2nd edition).
2. Type-2 Diabetes: This accounts for 90-95% of diabetes cases in
Nigeria and is usually associated with older age, obesity, physical inactivity, family history of Type-2 diabetes in first, 2nd or 3rd degree family members, or a personal history of gestational diabetes. It typically affects the black race and constitutes the main burden of diabetes in Nigeria. Although Type2 diabetes typically affects individuals older than 40 years, it has been diagnosed in children and adolescents and this emerging scenario is the result of the epidemic of obesity and inactivity in children these days. Type-2 diabetes can be prevented through healthy food choices, physical activity and weight loss. Confirmed cases can be
controlled with these same activities but oral medications or insulin may be necessary in addition.
Obesity and Type 2 Diabetes in Nigeria: Highlights from our
studies
(Ogbera AO, Fasanmade O, Chinenye S, Onyekwere C 2007).
1. Confirmed the association between obesity and Type 2 DM.
2. Earlier onset of Type 2 diabetes is associated with a higher BMI
(weight in kg divided by height m2) of over 25
3. Increasing prevalence of overweight and obesity is the most
important factor in the increasing number of younger people being diagnosed with Type 2 DM.
4. High waist circumference (≥94cm in men and ≥80cm in women)
increases the risk of developing diabetes, independent of the risk reflected by high BMI.
5. Diabetes can be prevented or delayed in people at high risk of
diabetes through a combination of healthy diet/lifestyle and modest weight loss.
Obesity is not because it runs in the family. It is because
NO ONE RUNS (exercises) in the family!!! Anonymous
3. Gestational Diabetes: Is a form of diabetes that is diagnosed only
during pregnancy. It occurs in African women who are obese or have a family history of type-2 diabetes. It requires treatment to bring the maternal blood glucose to normal levels and avoid complications of pregnancy wastage and other complications in the baby.
The outcome of recent Gestational Diabetes Study in UPTH using the new WHO Criteria revealed… that the overall prevalence among antenatal attendees is 15.2% (Chinenye, Akhidue, Ogu. Diabetes In Pregnancy: The Nigerian Perspectives using the new WHO criteria 2014).

Big babies ≥ 4kg
Difficult labour
Still birth
Pregnancy wastage
Maternal death etc.
Fig. 7: Pregnancy-induced Diabetes(source: www.bing.com/images)
4. Other specific types of Diabetes or Secondary Diabetes: It results
from other specific genetic conditions, medications, infections and other hormonal disorders. Secondary type of diabetes account for less than 3% of all diagnosed cases in Nigeria.
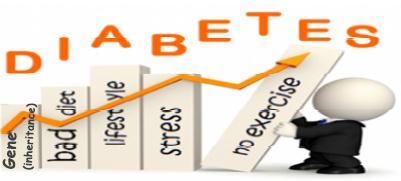
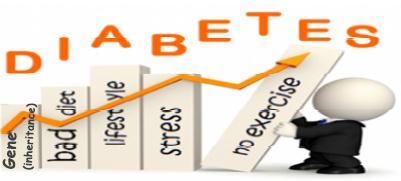
CAUSES OF DIABETES (ESPECIALLY TYPE 2 DIABETES)
Diabetes occurs when there is an imbalance between the demand and production of the hormone insulin due to interplay of genetic and environmental factors.
Fig. 8: Multi-factorial Causes of Diabetes
THE NATURAL HISTORY (PROGRESSION) OF DIABETES
Insulin is the main reason for diabetes. Insulin is a hormone produced
by some special cells of the pancreas, to regulate the level of glucose in
the blood. The special cells of the pancreas are the beta cells. Type 1
diabetes, as earlier stated, results when the beta cells are unable to
produce enough insulin, often because they have been destroyed by the
body's immune system, a process called autoimmune reaction.
Type 2 diabetes on the other hand, is a progressive disease that first results due to the insensitivity of the cells of the body to the actions of insulin, which triggers increased activity of the beta cells to surmount the resistance, resulting in the exhaustion of the beta cells and their loss of function.
It is estimated that patients with Type 2 diabetes have lost about 50-70% of the total stock of their beta cells, by the time they are diagnosed. This loss continues with the disease, at the rate of about 4% every year, such that most patients with Type 2 diabetes are without any functional beta cells, after about ten years with the disease.
Take Home Message
Patients with Type 2 diabetes at this later stage of the disease need insulin
injections, for the control of the disease in addition to the oral drugs.
Beta-cell function progressively declines
HOMA, homeostasis model assessment Lebovitz. Diabetes Reviews 1999; 7:139-53 (data are from the UKPDS population: UKPDS 16. Diabetes 1995; 44:1249-58)
Fig. 9: Beta-cell function progressively decline over time
The injection of insulin for the treatment of diabetes aims to mimic how
insulin is normally released by the beta cells of the pancreas. The beta
cells normally release insulin in two patterns: Small amounts of insulin
are continuously released by the beta cells, to maintain the blood sugar
at the normal level, and to ensure that glucose is continuously pushed
into the cells of the body, as and when the glucose is needed by the
body cells. This continuous release is called basal insulin production.
The beta cells release high doses of insulin, immediately after a meal,
first to stop the liver from pushing out more stored glucose into the
blood, and then to deal with the increased glucose level that follows the
consumption of a meal. This post-meal release of insulin is called
bolus insulin production. The amount of insulin released by the beta
cells is influenced by the carbohydrate content of the meal; the higher
the glycaemic index and the glycaemic load of the meal, the more the
insulin that is released to deal with the carbohydrate content of the
meal.
Insulin is secreted by the pancreas in a glucose-dependent manner continuously
throughout the day, as well as in response to oral carbohydrate loads
Fig. 10: Pattern of natural insulin release visa viz Glucose Level
When insulin is used to treat diabetes, it is injected to meet the basal
insulin need, the bolus or meal-related insulin need, or both. Patients
with type 1 diabetes and those in the late stage of type 2 diabetes need
insulin injections to cover both the basal needs and the bolus needs, due
to the total inability of their beta cells to produce insulin. Doctors refer
to this as basal-bolus insulin treatment.
Patients in the early stage of Type 2 diabetes who require insulin are
given smaller doses, and are not often placed on basal-bolus insulin
treatment, because their beta cells are still producing insulin, and
several of the oral anti-diabetes drugs are still very effective in them.
Insulin is often the drug of last resort, these patients are therefore only
given the insulin that help address the specific problems that could not
be resolved with the other anti-diabetic drugs. For example, patients on
oral anti-diabetes drugs who have problem of high blood sugar level in
the morning (fasting hyperglycaemia) are often given a basal dose of
insulin injection at night to help them deal with the problem; while
those with high blood sugar levels after a meal (post-prandial
hyperglycaemia) are given bolus doses of insulin injection with meals.
The Key Problems in Diabetes
(a) Insufficient production of insulin (either absolutely or relatively to
the body's needs)
(b) Inability of body cells to use insulin properly and efficiently,
leading to hyperglycaemia and diabetes (insulin resistance)
(c) Production of defective insulin (uncommon) (d) Steady decline in number of Beta-cells, adding to the process of
elevated blood sugars.
DIAGNOSIS OF DIABETES MELLITUS: SCREENING TESTS
AND CONFIRMATION
Table 3: Diagnosis of Diabetes Mellitus: Screening tests and
confirmation
WHO: Diagnostic Criteria for Diabetes Mellitus
Plasma Venous Glucose Concentration
Parameter & Year
Diabetes Mellitus
2-h post-load glucoseor
IGT (Impaired Glucose
Fasting* and 2-h post-
≥7.8 and <11.1
≥140 and <200
IFG:(Impaired Fasting
HbA1c >7.0 is call for action
to initiate or change therapy
IFG=impaired fasting glucose; IGT=impaired glucose tolerance; T2DM=type 2
diabetes mellitus; WHO=World Health Organization
*In asymptomatic patients, 2 abnormal fasting values are required for diagnosis
Adapted from World Health Organization.Definition, Diagnosis and Classification of
Diabetes Mellitus and Its Complications. Geneva: WHO; 2006 & 2010.
DEALING WITH A POSITIVE RESULT OF DIABETES
The reactions to a positive result of diabetes are varied; however they
are always powerful.
Emotions may range from shock, disbelieve to even suicidal tendencies.
These emotions are completely normal and have been found to be
similar to the bereavement felt with the death of a loved one.
The emotions come in five stages, as put forward by Elizabeth Kubler-
Ross following her study on terminally ill patients.
The stages and intensity of their expression in a person is as unique as
the person expressing them.
The five stages of the emotions are:
Stage 1: Denial ("I reject it! It's not my portion!!")
Stage 2: Anger
Stage 3: Bargaining
Stage 4: Depression; and
Stage 5: Acceptance
The danger is that in-between Denial and Acceptance many Nigerians
diagnosed with diabetes derail and may die from acute or chronic life-
threatening complications.
DIABETES IN NIGERIA: FEATURES AND MANIFESTATIONS
Diabetes as a chronic condition is characterized by patterns of
symptoms, stages of clinical severity and natural progression and all
these have impact on health and social function.
Symptoms of Type 1 diabetes usually develop quickly over a few days
to weeks and are caused by high blood sugar. At first, symptoms may
be overlooked or mistaken for another illness like malaria or typhoid
etc.
High blood sugar symptoms include:
Urinating a lot (polyuria) which may be more noticeable at
night. The kidneys are trying to get rid of the excess sugar in the blood. To do that, they have to get rid of more water. More water means more urine.
Being very thirsty (polydipsia) – This happens because
urinating so often, you lose much water to become dehydrated.
Losing weight, but not intentionally. This results from loss of
water and sugar (calories) including proteins.
Increased hunger (polyphagia) – They feel hungry because the
cells aren't using the calories they need. Calories leave the body via the urine.
Blurry vision – when sugar builds up in the lens of the eyes, it
sucks extra water into the eyes. This changes the shape of the lens and density of the eye fluids.
Feeling very tired – you aren't using the calories you are
consuming and the body isn't getting the energy it needs. It's like starvation in the midst of ‘wasted' plenty.
The diagnosis of type 2 diabetes is readily recognised when a patient presents with classic symptoms of polyuria, polydipsia, polyphagia and blurring of vision; however as many as 50% of Nigerians with type 2 diabetes are symptomless and their disease remains undiagnosed for many years… that is the danger, so go for screening!!! (Chinenye et al Clinical Practice Guidelines for Diabetes Management in Nigeria 2013).

DIABETES: KNOW THE SYMPTOMS
(Especially during the night)
Fig. 11: Diabetes: Know the Symptoms (source: www.bing.com/images)
Associated Multiple Chronic Conditions
The burden of diabetes is often compounded by multiple chronic
conditions (MCCs) or comorbidities that contribute to worse outcomes,
multiple organ systems involvement, complex treatment approaches and
decreased adherence to treatment (Chinenye et al. Diabetes Advocacy
and Care in Nigeria 2014). The prevalence of MCCs increases
substantially among adults with diabetes over age 45 years.
The difference between older and younger persons with diabetes must
be considered in population-based approaches to living well with
diabetes.
Similarly, the social determinants of health as the context for a population-based approach to living well with diabetes must be recognized.
HEART DISEASE,
(TB Cases= 12.3% DM)
(Without TB= 5.6% DM)
HIV/AIDS
(DM=12.7%
Abnormal
HAART treated)
cholesterol &
other fatty
(Depression, anxiety,
insomnia, cognitive
substances
deficiency)
treated)
Fig. 12: Associated Multiple Chronic Conditions
(Ogbera, Chinenye et al 2007; Uloko, Gezawa, Mohammed et al 2014;
Ogbera, Kapur, Chinenye et al 2014)
DIABETES: COMPLICATIONS
The burden of diabetes lies in the complications of diabetes. The
complications of diabetes are also responsible for much of the ill health
and deaths that results from the disease. How well you are able to deal
with the complications of diabetes would therefore determine how well
you would live with the disease.
The complications of diabetes are of two types – acute and chronic.
Acute complications result from the massive disruptions caused by
diabetes to the proper functioning of the body, which present as medical
emergencies that require immediate medical treatment, to save the life of the patient. Chronic complications on the other are caused by the cumulative damages done to the body, by the tissue starvation and high blood sugar level created by diabetes. Acute diabetic emergencies often present as diabetic coma, but are specifically caused by (Ogbera AO, Chinenye S, Onyekwere A, Fasanmade O 2007):
Diabetic ketoacidosis (toxic metabolic acids builds up from high
Hyperosmolar hyperglycaemic state.
In acute complications, there may be nausea, vomiting, sweet smelling
breath, fast breathing, abdominal pain and irritability.
Although diabetes affects every part of the body, the following chronic
complications have been noted to have more significant effects on
health and wellbeing:
Problems that affects the heart and the blood vessels (cardiovascular
Problems that affects the kidneys (diabetic nephropathy)
Problems that affects the eyes (diabetic retinopathy)
Problems with the nerves of the body (Diabetic Neuropathies)
Problems with the feet (Diabetic foot);
Teeth problems
Sexual problems; and
Problem with infections
Fig. 13: Diabetes Complications (source: www.bing.com/images)
Uncontrolled diabetes results in multiple complications e.g. heart disease, stroke, kidney failure, blood vessel disease, nerve damage, impotence, infertility, difficult labours, intra-uterine deaths, still births, amputations, blindness and even sudden death.
There is no corner of our dear country today that is free of diabetes.
Wherever you live, work or play, someone you know – maybe even you
seated in this auditorium – may be struggling with diabetes and its
complications.
THE BURDEN AND STATUS OF DIABETES CARE IN
NIGERIA
In collaboration with my colleagues, I pioneered some landmark studies
to ascertain the State of Diabetes Care in Nigeria.
Some of these studies are summarized:
(A) The Pattern of Diabetes mellitus in Rivers State, Nigeria: This
was a cross-sectional study of people living with diabetes attending the
local diabetes association meetings and diabetes clinics at the
University of Port Harcourt Teaching Hospital (UPTH) and BMSH over
a five year period [Jan. 2001 to Dec. 2005] (Chinenye et al. The Pattern
of Diabetes mellitus in Rivers State, Nigeria 2008).
They were recruited after ethical approval and obtaining their informed
consent. They were either newly diagnosed or old patients. Physical and
biochemical evaluations were carried out. A total of 10,518 people
living with diabetes were seen during the study period from the 23
Local Governments (LGAs) of Rivers State. There were 5,350 females
(50.9%) and 5,168 males (49.1%) giving F:M ratio of approx 1:1.
The majority were adults (93.9%) aged 20 years and above (see Table
below). 830 of the newly diagnosed subjects were further evaluated for
clinical/biochemical
characteristics,
complications on initial presentation. These comprised 25 type 1 diabetes (3.0%), 780 type 2 (98.0%), 10 (1.2%) Other specific types and 15 (1.8%) with Gestational diabetes. At diagnosis, the type 2 subjects (780) had the following complications namely: Neuropathy 439 (56.3%), erectile dysfunction 283 (36.3%), nephropathy 72 (9.2%) and retinopathy 57 (7.3%).
Table 4: LGA Distribution of Diabetics seen in Rivers State
No. OF DIABETICS
GOVERNMENT AREA
DIABETICS
OGBA/EGBEMA/NDONI
Table 5: Clinical Features of 830 Diabetics
PARAMETERS
TOTAL NUMBER (n)
%
Positive Family
408 (52.3%)
8 (53.3%)
History OF DM (1ST
Degree)
Polyuria
Blurring Of Vision
Recurrent Carbuncles
Calcification Peripheral Neuropathy
Erectile Dysfunction
283 (36.3%)
*Antedated
106 (13.6%)
5 (33.3 %)
197 (25.3%)
(Mono)Therapy Insulin Therapy
Oral Hypoglycaemic
Agents (OHA) Note: DM – Diabetes Mellitus GDM – Gestational Diabetes Mellitus Erectile Dysfunction (ED): Defined as the inability to achieve and maintain erection sufficiently enough to allow satisfactory sexual intercourse
(B) Nigerian DiabCare Study: In a multicentre study involving seven
teaching hospitals in Nigeria including UPTH, we set out in 2008 under
the auspices of Diabetes Association of Nigeria to assess the clinical
and laboratory profile of Nigerians living with diabetes. This was to
evaluate the quality of care of Nigerian diabetics with a view to
planning improved diabetes care (Chinenye et al. Profile of Nigerians
with diabetes mellitus – Diabcare Nigeria Study: Results of a
multicentre study 2012).
A total of 531 out-patients enrolled, 209 (39.4) males and 322 (60.6%)
females. The mean age of the patients was 57.1 ± 12.3 years with the
mean duration of diabetes of 8.8 ± 6.6 years. Majority (95.4%) had type
2 diabetes mellitus compared to type 1 (4.6%), with p<0.001.
The mean FPG, 2HrPPGlucose and HbA1c were 8.1 ± 3.9mmol/L, 10.6
± 4.6mmol/L and 8.3 ± 2.2% respectively.
Only 170 (32.4%) and 100 (20.4%) patients achieved the ADA and IDF
blood sugar targets respectively.
Most patients (72.8%) did not practise self-monitoring of blood glucose.
High blood pressure (hypertension) was found in 322 (60.9%) of the
subjects.
Diabetic complications found were peripheral neuropathy (59.2%),
retinopathy (35.5%), cataracts (25.2%), stroke (4.7%), diabetic foot
ulcers (16.0%) and nephropathy (3.2%).
This landmark study concluded that Nigerian diabetics have suboptimal
blood sugar control, are hypertensive and have chronic complications.
The study group recommended that improved quality of care and
treatment to target should be implemented to reduce diabetes-related
morbidity and mortality.
Diabcare Nigeria Multi-Centre Study:
Table 6: HbA1c Levels Stratified by Different Guidelines
Guideline
Definition
Proportion of
patients
achieving
target, n (%)
for adults with diabetes
IDF (Type 2) Target
N: number of valid patient data used in the analysis
n (%): number of patients (percent)
(C) The Diabetic Foot
During the Nigeria DiabCare Study, many patients with Diabetic Foot
were recruited from UPTH. Diabetic Foot refers to the variety of
pathological conditions that may affect the foot of persons with diabetes
(Ekere AU, Chinenye S et al. The Diabetic Foot- A Review 2003),
ranging from superficial skin ulcers (sores) to outright foot gangrene
leading to amputation. Currently, Diabetic Foot is the commonest
reason for amputation in most Nigerian hospitals including UPTH.
The burden of Diabetic Foot syndrome is enormous on the patient and
society in general. It consumes a significant proportion of the health
budgets which results in significant loss in economic productivity and
social status.
Pictorial Chart of Diabetic Foot Ulcer in UPTH
Viewer discretion advised!
These plethora of Diabetic Foot consisted of individuals from various social classes
in Nigeria attending UPTH:
Figure 14: Photos of Diabetic foot ulcers in UPTH medical wards
Our studies revealed high prevalence of peripheral neuropathy among
our diabetics (Unachukwu CN, Babatunde S, Chinenye S. Peripheral
Neuropathy and Macroangiopathy in Diabetics with Foot Ulcers in Port
Harcourt 2004) with consequent "loss of foot protective sensations".
Once loss of protective sensation occur, mechanical injury to the foot
can occur without the patient perceiving it as disturbingly painful. It is
in fact this lack of pain that causes the patient to either ignore the
wound or becomes fetish about its origin.
Patients with diabetes are 25 times more likely to have their leg
amputated than people without diabetes.
The amputations unfortunately often do not only result in the loss of
the limb, but sometimes result in the loss of life of the patient.
The treatment for Diabetic Foot is about the most expensive, even
as it does not guarantee the salvation of the leg or life of the patient.
Commonest reason for prolonged hospitalization in UPTH and
elsewhere (15-270 days).
The problem of diabetic foot arises due to the combination of the sensory neuropathy that damages nerves and makes it difficult for the diabetic patient to feel; the blood vessel disease that reduce the supply of blood to the foot, and the reduced immunity caused by diabetes that makes it difficult for the patient to fight infection. These factors make it easier for the diabetic patient to sustain skin ulcers on the foot, and for the ulcers to become infected, and in serious
cases, for the infected ulcer to progress and become gangrenous, and then wither the foot. The patient at this stage often requires the amputation of the affected foot to save his/her life.
Diabetic foot often follows a train of events that starts with the loss
of sensation, as a result of the sensory neuropathy caused by the
disease. The loss of sensation cause the deformation of the foot
(Charcot's joint), as the patient continues to walk on an injured
foot, to the point that it causes the dislocation of the joints.
This dislocation causes the shoes to fit poorly, causing ulcer to
develop. The ulcer easily becomes infected, when the blood sugar level is not properly controlled, because the high sugar content of the blood provides very good nourishment for germs to grow and multiply.
The normal response of the body to the presence of germs is often
not present, because diabetes depresses the body's immune response to the presence of the germs. This is not helped by the fact that the blood vessel disease that often complicate diabetes reduce blood supply to the foot, thereby placing a road block to the mobilization of the body's immune soldiers to fight the infection.
The holdup created by blood vessel disease often eventually
completely cuts off blood supply to the infected limb, resulting in the death of the tissues around the ulcer. This area of dead tissue often grows in size, such that the limb often requires to be amputated as a life-saving measure.
Fig. 15: Diabetic Foot
For early detection and preventive measures, diabetic foot
examination consists of:
o A visual examination of the foot o A lookout for foot deformity o A clinical test for sensory loss o A clinical test for peripheral blood vessel disease. o The examination of the foot wear
Diabetes Foot Care: Dos and Don'ts
Do wear well-fitting shoes. Shoes should be supportive, have low
heels (less than 5 cm high) and should not rub or pinch. Shop at a reputable store with knowledgeable staff who can professionally fit your shoes.
Do elevate your feet when you are sitting. This would help blood to
circulate in the feet, and reduce some of the effects of blood vessel disease
Do wiggle your toes and move your ankles around, for a few
minutes several times a day, to improve blood flow in your feet and legs.
Do exercise regularly and as much as possible. It would help
improve circulation, and reduce the incidence of crampy pains in the legs.
Do inspect your feet daily and in particular, feel for skin
temperature differences between your feet.
Don't wear high heels, pointed-toe shoes, sandals (open-toe or
open-heel) or worn-out shoes.
Don't wear anything tight around your legs, such as tight socks or
Don't ever go barefoot, even indoors. Consider buying a pair of
well-fitting shoes that are just for indoors.
Don't put hot water bottles or heating pads on your feet.
Don't cross your legs for long periods of time.
Don't smoke. Smoking decreases circulation and healing, and
significantly increases the risks of amputation.
Don't have pedicures by non-health care professionals.
We recommend early screening for loss of foot sensation (peripheral
neuropathy), in addition to meticulous foot care and improved blood
sugar control, to reduce the occurrence of foot ulceration (sores) and
gangrene with the attendant human suffering and loss of economic
resources.
(D) Diabetes in the Elderly - Niger Delta experience
This was a cross-sectional study carried out in elderly patients
developing diabetes for the first time (Chinenye et al. Diabetes mellitus
in the elderly 2012). The aim of the study was to assess their common
pattern of presentation and their clinical and biochemical
characteristics.
Methods:
All newly-diagnosed elderly (≥65 years) patients with type2 diabetes
presenting at UPTH, Port Harcourt over a period of 3-6 months were
assessed with interviewer-administered questionnaires. Their BP, BMI
and biochemical parameters including FPG, lipid profile and creatinine
were measured. Kidney, nerve and eye complications were assessed
during the study.
Results:
There were 19 males and 33 females with a mean age of 70.5±4.9 years.
Their presenting symptoms ranged from no symptoms i.e. diagnosed
while being investigated for other illness (46.2%), symptoms of DM
(27%), eye symptoms (9.6%) and symptoms of complications such as
nerve damage, leg swelling and stroke (17.2%). Only 15.4% of the
patients carried out regular exercise at least two times a week. History
of DM in a first degree relative was present in 57.7%. The average BMI
was 26.7±3.8kg/m2, with 42.3% overweight and 21.2% obese.
Hypertension was present in 51.9% of the patients. The average FPG
was 8.3±3.9mmol/L. Good glycaemic control (FPG < 7.2mmol/L) was
present in 42.3%. The average total cholesterol was 190±34.9mg/dl. A
total cholesterol level greater than 200mg/dl was present in 38.5% of
the patients. The average triglyceride was 106.8±35.6mg/dl and 14.9%
had levels ≥ 150mg/dl, while the average bad cholesterol (LDL) was
128.1±34.5mg/dl with 55.8% having LDL ≥ 115mg/dl. Only 29.8% had
good cholesterol (HDL) ≥ 45mg/dl. Complications were present in
30.8% of the patients. 17.3% had nerve damage (neuropathy) at first
diagnosis, 5.8% had eye complications and abnormal kidney function
(GFR) was present in 59.6%.
The study concluded that diabetes in the elderly is associated with a
high degree of heart-related risk factors, complications and is frequently
detected in the course of other illnesses.
Table 7: Presenting symptoms at detection of diabetes in males and
females
Variables
Female (%)
Total (%)
Classical symptoms
19(36.4)
33(65.4)
Table 8: Complications of diabetes in the elderly patients
Percentage (%)
Neuropathy (nerve damage)
Nephropathy (kidney damage)
Eye complications
Nerve/kidney damage
Eye complications + kidney
(E) Diabetes in Pregnancy: The Nigerian Perspectives
This study was aimed at determining the prevalence of diabetes in
pregnancy (GDM) and associated factors among antenatal women in
Port Harcourt using the new World Health criteria (Chinenye S, Ogu R,
Akhidue K 2015).
Methods
In this study, antenatal women were tested using 75g glucose load and
obtaining fasting (5.1 – 6.9mmol/L), 1hr (≥10.0mmol/L) and 2hr (8.5 –
11.0mmol/L) glucose values; one value being sufficient for diagnosis;
and associated anthropometric and clinical factors including primary
and secondary outcomes.
Results
Results reveal that 26.5% of the subjects had a family history of
Diabetes while 12.9 %, 7.6% and 11.4% were diabetic using the FPG,
1hr-PPG and 2hr-PPG respectively of the new WHO CRITERIA.
The overall prevalence of GDM in the study population was 15.2%. The
outcomes of birth weight, mode of delivery, neonatal hypoglycaemia,
need for Neonatal Intensive Care (NIC) and preeclampsia were
documented.
Conclusion
Diabetes Association of Nigeria has adopted these new World Health
criteria and is translating the recommendations into local practice with
Port Harcourt setting the pace in Nigeria.
(F) Sociocultural factors: Evidence from review studies in Nigeria
underscore the following Sociocultural and economic factors
militating against diabetes care (Chinenye et al. Sociocultural
aspects of diabetes in Nigeria 2013):
1. Low level of health literacy among Nigerian diabetics 2. Erroneous religious beliefs, myths and misconception about
3. Poor adherence to medications 4. Socioeconomic circumstances (poverty etc.) 5. Poor physician-client relationship 6. Low level of family support 7. Westernization with increasing sedentary living, overweight and
8. Inadequate and declining support to diabetic patients 9. Frustration and helplessness among the less privileged persons and
families of diabetics
10. Increasing complications and deaths associated with diabetes
resulting from poverty, fake drugs and poor health services in Nigeria
11. Increasing misinformation about diabetes and the practice of
inappropriate care across Nigeria especially from alternative healthcare providers.
12. Very weak financial status of diabetes advocacy groups e.g. DAN,
at all levels, thereby decreasing performance and output
THE CONCEPT OF LIVING WELL WITH A CHRONIC
DISEASE OR ILLNESS (DIABETES)
A chronic disease or illness, in general terms, is a condition that is slow
in progression, long in duration, and devoid of spontaneous resolution
and if not well treated, often limits the function, productivity and
quality of life of any individual who lives with it [Institute of Medicine,
2012].
Diabetes mellitus is a chronic illness and is also marked by the
experience of long-term bodily or health disturbance such as fatigue,
confusion or social stigma and how people live and cope with
disruption to their daily lives.
Chronic diseases or conditions have emerged in recent decades as the
major cluster of health concerns for the Nigerian people e.g. Diabetes
mellitus, Hypertension, Cancer, Asthma etc.
A chronic illness like Diabetes Mellitus imposes an enormous and
growing burden on individuals, families, communities and the nation as
a whole.
For Nigerians who are living with diabetes, access to suitable disease
treatment programs is uneven, disparities among sections of the country
persist and shortcomings in the quality of care are all too common.
Living and coping with chronic illness is not Nigeria's challenge alone.
On September 19 – 20, 2011, for the 1st time, the United Nations took
up the topic of chronic non-communicable diseases as a principal
agenda at a plenary High level summit. The rising burden of chronic
disease affects countries at every position on the economic spectrum.
Each has much to learn from others, recognising that differences in
culture, conditions and circumstances will demand distinctive solutions.
Diabetes Mellitus: The Bio-psychosocial Perspectives
Hygienic and sanitary advances have greatly prevented many previously
common infectious diseases. Immunizations, clinical and community
interventions have substantially controlled many past causes of chronic
infectious illnesses such as tuberculosis, polio etc though not
completely eliminated.
However, these advances have been compromised by parallel increases
in physical inactivity, unhealthy eating, overweight, obesity, tobacco
and alcohol use, and other chronic disease risk factors including
exposure to environmental pollutants as seen in the Niger Delta region.
Today, virtually every Nigerian family has recorded a case of diabetes
in a 1st, 2nd or 3rd degree family member. Diabetes Association of
Nigeria (DAN) estimates that there are about five million Nigerians
living with Diabetes Mellitus (Chinenye et al. Diabetes Advocacy and
Care in Nigeria 2014) and World Health statistics indicate that Nigeria
has the highest number of people with diabetes in sub-Saharan Africa
(IDF Diabetes Atlas 6thed 2013).
Diabetes and other chronic diseases have now emerged as a major
public health problem and it threatens not only population health but
also social and economic welfare.
Diabetes not only impact the social and economic lives of millions of
Nigerians and their families but also is a major contributor to healthcare
costs.
Diabetes is thus a common public health as well as a clinical problem in
Nigeria. Therefore, a biopsychosocial perspective for understanding
diabetes, developing policies, strategies and interventions to combat it is
critical. A biopsychosocial perspective considers how individuals'
genes, biology and behaviours interact with the social, cultural,
psychological and physical environment around them to influence
health outcome for the entire diabetic population.
Determinants of Diabetes Health
Spectrum of Diabetes Health
cultural
Physical
Environment
Peers and
Patterns of
Impairment
Response
Over the Life
Functional
Behavior
Limitation
Disability
Terminal
Policies and Other Interventions at Individual and Community
Community
Fig. 16: Integrated Bio-psychosocial Model
Note:
Pre-DM: Pre-diabetes, DM: Diabetes Mellitus
Surveillance for diabetes and its outcomes is critical to identifying
needs, setting priorities for action and assessing programmatic
progress.
The principal aim of any diabetes health intervention is to eliminate
mortality or reduce morbidity i.e. managing each affected person and
the population as a whole to "live well" regardless of diabetes or an
individual's current state of disability. Thus, the concept of living well
with diabetes reflects the best achievable state of health that
encompasses all dimensions of physical, mental and social well-being.
Living well with diabetes is determined by the physical, social,
psychological and cultural surroundings and by the effects of diabetes –
not only on the affected individual, but also on family members, friends
and care-givers.
In this way, progress towards living well with diabetes can be achieved
through the combined efforts of both individuals and society to reduce
disability and improve functioning and quality of life regardless of each
unique individual's current health status or the stage of diabetes.
DIABETES CARE AND TARGETS OF CONTROL
The goals in caring for people with diabetes are:
To eliminate symptoms To prevent or at least slow the development of
To improve health and longevity
Diabetes is a multi-faceted disorder and the demands of control parameters are progressive (Chinenye et al. Current Concepts in the Management of Diabetes 2006).
Table 9: Essential Components of Diabetes Care
1. Treatment of High Blood Sugar (Hyperglycaemia; the root of
"all evils" in diabetes)
(a) Non-Pharmacological measures
Education [DSME]
Physical Activities (exercise)
(b) Drug treatment
Oral glucose lowering agents
Insulin [injectable form]
(c) Combination therapies
oral glucose lowering agents plus insulin
2. Treatment of High Blood Pressure (Hypertension) and High
(a) Non-pharmacological
Exercise (physical activity)
(b) Drug treatment
3. Prevention and treatment of acute complications
4. Prevention and treatment of chronic complications
Team-Based Care
Diabetes Care through a team approach is more effective than that from a single provider, and efforts to raise the quality of care by team improvements are more effective on blood glucose and other control parameters.
PRIMARY CARE PROVIDER AS
DIABETES CARE
SPECIALIST /
OTHER TEAM MEMBERS OR CONSULTANTS
EMPLOYERS
DIABETES SUPPORT GROUPS
Fig 17: Diabetes Care Team
Concurrent treatment of secondary factors such as hypertension,
obesity and high cholesterol including smoking cessation are usually
required because these factors drive the development of
complications.
Eye, kidney and nerve complication reduction is accomplished through
control of blood sugar and pressure; heart, brain and blood vessel
complications are reduced through control of blood sugar, cholesterol,
blood pressure, smoking cessation and prevention of clots formation.
Diabetes care requires appropriate goals setting, dietary, exercise and
medications adherence, (very important), appropriate self-monitoring of
blood glucose (SMBG), regular screening for complications, and
recommended laboratory assessment. Others include maintenance of
ideal body weight and optimal blood pressure.
The Use of Insulin in treating Diabetes
The safe use of insulin in the treatment of diabetes would involve
knowledge of:
How insulin works
Indications for insulin use
The available insulin preparations (we have progressed from
Animal → Human Insulin → Insulin analogues)
The common insulin prescription plan
The implementation of the insulin prescription plan
The different types of insulin delivery devices (we have
progressed from syringes and needles → reusable pens → disposable pens with micro fine needles).
How to recognise and deal with the side-effects of insulin use
(hypoglycaemia and weight gain)
Patient-centred, family-centred & community-oriented Care
The components of lifestyle interventions include medical nutrition
counselling, exercise recommendations and comprehensive diabetes
education with the purpose of changing the paradigm of care in diabetes
from provider-focused to patient-centred as depicted below (Chinenye
et al. Patient-centred care in diabetology: sub-Saharan African
Perspectives. AJDM 2014).
PATIENT-CENTRED, FAMILY-CENTRED & COMMUNITY-ORIENTED CARE
PATIENT-CENTRED, FAMILY-CENTRED & COMMUNITY-ORIENTED CARE
(Chinenye et aL. 2014.Patient-centred Care in Diabetology: sub-Sahara African perspective)
(Chinenye et cL. 2014.Patient-centered Care in Diabetology. sub-Saharan African perspective)
Patient factors
Background to
incorporating overt physical,
psychological, emotional, and
social needs of patient
following the patients' path
To be there
Fig. 18: Patient-centred Care in Diabetes
It is the quality of the relationship between the health
professional and the patient that is central to the therapeutic process.
The diabetic patient should no longer be taken as a complex
bio-medical machine.
Rather as an integrated Bio-psychosocial Being at a given stage
of his or her life-cycle.
In the current socio-economic environment, the average
Nigerian with diabetes enjoys better literacy, education, communication and awareness than before.
Family-centred and community-oriented treatment must be
practised, keeping the family and community as interventional units in diabetes care.
Physician/Patient Partnership
Educate continually
Include the family
Provide information about diabetes
Provide training on self-management skills
Emphasize partnership among healthcare providers, the patient
and the patient's family e.g. join the Diabetes Association.
Targets for Diabetes Care
Targets are evidence-based benchmarks in treatment of diabetes with
respect to blood sugar, blood pressure, cholesterol levels etc. Without
some form of targeted control of diabetes, it becomes difficult to
promote care at all.
Achieving and maintaining good blood sugar control by treating-to-
target, is the goal of using guidelines (Chinenye et al. Clinical Practice
Guidelines for Diabetes Management in Nigeria 2013, 2nd edition)
How do we treat-to-target?
Taking control and achieving control.
Taking control – Empowering the diabetic patient to manage
his/her condition in partnership with care givers and loved ones (through Diabetes Self-management education, DSME)
Achieving control – Reducing the impact of diabetes so that
patients can live a normal life (through monitoring, prescribed appropriate and adequate medications, diet and exercise).
Table 10: IDF optimal targets for glycaemic, lipid, blood pressure
and weight control
Biochemical Index:
Capillary blood glucose values (finger-prick)
2-hour post-prandial (post-meal)
Glycated haemoglobin (HbA1c) (%)
Weight BMI (kg/m2)
Blood Pressure (mmHg):
If persistent, dipstick for proteinuria
Total cholesterol
Diabetes Association of Nigeria is a key member of International Diabetes Federation (IDF) IDF is the global umbrella of all diabetes associations and plays the role of a specialized agency of World Health.
STANDARDS OF CARE
Standard Care
Involves:
Maintaining HbA1c below 6.5% which should minimize risk of
developing complications.
Providing lifestyle and education support, and titrate therapies, to
enable people with diabetes achieve HbA1c below 6.5 % (where feasible and desired), or lower if easily attained.
Advising those in whom target HbA1c levels cannot be reached
that any improvement is beneficial.
Raising targets for people on insulin or some tablets whose
attainment of tighter targets may increase the risk of hypoglycaemic episodes, which may present particular problems for people with other physical or mental impairment.
Equivalent target levels for capillary plasma glucose levels are <6.0
mmol/L (<110 mg/dl) before meals, and <9.0 mmol/L (<160 mg/dl) 1-2 h after meals.
Comprehensive Care
The target levels here are as for Standard care, but it may be
possible to devote more resources to achieving lower target levels without adverse impact on health.
Minimal Care
The target levels here are as for Standard care, but may need
to be based on measurement of plasma glucose levels ALONE, especially in rural settings where facilities for HbA1c are not available.
The Relevance of Monitoring in Diabetes Care
(a) Haemoglobin A1c (HbA1c) Test as Monitoring Standard:
HbA1c test is very accurate because the method(s) of measurement is
now well standardized. This test is for long term glucose control (2-
3months) and measures sugar molecules attached to haemoglobin and
the result should be less than 6.5% when diabetes control is optimal.
This is the gold standard for assessing Diabetes Control.
(b) Home Self-monitoring of Blood Glucose (SMBG): This
underscores the following:
o Day-to-day blood sugar variations.
o Core component of effective DM self-management.
o Day-to-day treatment options and adjustments.
o Titrate treatment to prevent ‘hypo' episodes.
Diabetes Self-Management Education
Definition: Diabetes Self-Management Education (DSME) is the on-
going process of facilitating the knowledge, skill and ability necessary
for diabetes self-care (Funnel et al. Diabetes Care 2010).
This process incorporates the needs, goals and life-experience of the
person with diabetes and is evidence-based.
Objectives
Support informed decision-making
Support self-care behaviours
Support problem-solving and active collaboration with the health team
To improve clinical outcomes, health status and quality of life
Diabetes Self Care
The World Health in 2009 defined self-care as "Activities that
individuals, families and communities undertake with the intention of
enhancing health, preventing disease, limiting illness and restoring
health." These activities are derived from knowledge and skills from the
pool of both professional and lay experience. They are undertaken by
sick people on their own behalf, either separately or in participative
collaboration with professionals.
The components of self-care strategies in Diabetes include:
Dietary planning
Physical activities (exercise)
Medication adherence (including self-administration of insulin)
Self-monitoring of blood glucose (SMBG)
Problem solving skills (management of hypo & hyper
Reducing risks (smoking cessation, eye, foot and dental care)
Healthy coping (stress management, psycho-sociocultural
issues, family and social support)
Self-care interventions do not only contribute to prevention of organ damage in diabetes, they are also of proven effectiveness in other chronic conditions e.g. hypertension etc.
Guiding Principles
1. Diabetes education is effective for improving clinical outcomes
and quality of life
2. DMSE has evolved from primarily didactic presentations to
empowerment models
3. DSME programs incorporating behavioural and psychosocial
strategies demonstrate improved outcomes e.g. DAWN Study.
4. Culturally and age-appropriate programs improve outcomes and
group education is effective.
5. On-going support is critical to sustain progress made by
participants during DSME program (Norris SL et al. 2002).
6. Behavioural goal-setting is an effective strategy to support self-
management behaviours (Funnel MM, Brown TL. 2010).
Take Home Message
Unlike other diseases, people with diabetes are responsible for 95% of
their own care. Yet, many are faced with managing this disease –
including making complex daily health decisions – without proper
education regarding their diabetes.
Diabetes Educator
Diabetes Educators are healthcare professionals who focus on helping
people with and at risk for Diabetes and related conditions achieve
behaviour change goals which in turn lead to better clinical outcomes
and improved health status.
Certified Diabetes Educator
Qualified healthcare professionals including, but not limited to:
- Physicians, especially endocrinologists
- Registered Nurses
- Registered Dieticians
- Mental health professionals
- Physiotherapists
They help clients learn how to manage their diabetes.
Table 11: Roles and Functions of the Diabetes Educator
Help PLWD develop
Effective coping strategies
effective coping strategies
Identify psychological and social
for the variety of health-
barriers that affect your health
related situations that arise
because of Diabetes
Teaching the importance
Quitting smoking
of Self-care Behaviour
Having regular eye and foot
Monitoring blood sugar, blood
pressure &cholesterol
Keeping personal care records
How your medicines work
Adherence Counsellor
Taking medicines
Potential side-effects of your
Timing and frequency of
What happens if you don't adhere to
Self-administration of insulin
Proper use of the monitoring
Relevance of Monitoring
information about
How often and when you should test
blood sugar, blood
What appropriate target ranges are
pressure and other
How to interpret test results
diabetes monitoring equipment.
The effects of food on blood sugar
Healthy Eating Education
Sources of carbohydrate, fat and
Effective meal planning Resources that you can use to make
wise food choices
Develop a physical activity plan
Physical Activity
Discuss about ways to overcome
Education
common barriers to increased physical activity
Education should be provided at a level appropriate to the patient understanding and targeting erroneous beliefs and attitudes about diabetes.
"I do not run like a man running aimlessly; I do not fight like a man beating the
air. No, I beat my body and make it my slave (to achieve my aim, for a long and
healthy life!!!) 1 Corinthians 9:26-27
LIVING TO A GRAND OLD AGE WITH DIABETES – A STEP-
BY-STEP GUIDE
The Holy Land, Jerusalem, operates on the principle that "Medical
Healing and Divine Healing are complimentary!"
– The Holy Land Injunction
This is summarized as follows:
Step One: Take time off, to tell your God and yourself why you must
live well, in spite of the Disease (diabetes).
Step Two: Learn as much as possible about diabetes
"My people perish for lack of knowledge…" (Hosea 4:6).
"…the excellence of knowledge is that it giveth life to them that have
it". Ecclesiastes 7:12
Step Three: Have a Health Plan with Life-style Modification
Joel Ostein wrote a book titled "Become a better you"
"It is not the strongest of the species that survives, nor the most
intelligent, but the one most responsive to change"- Charles
Step Four: Build a Support Team e.g. Join the Diabetes Association of
Step Five: Commence your Health Plan immediately
Step Six: Religiously follow the Health Plan
Step Seven: Regularly look out for Complications
Step Eight: Go for regular Health Checks e.g. always keep your
hospital appointments.
"Knowing is not enough; we must apply. Willing is not enough; we
must do." - Johann von Goette [German writer & statesman]
The Dietary Management of Diabetes
No matter the type, stage or severity of diabetes, dietary management
otherwise called Medical Nutrition Therapy, is a very crucial aspect of
the overall management of diabetes which may involve Diet alone, Diet
with oral glucose-lowering agents or Diet with insulin.
The type and amount of food consumed is a fundamental determinant of
diabetes health.
In the Nigerian setting, there is no scientific reason why our diabetic patients should be restricted to a diet of unripe plantain and beans. This is unacceptable and is hereby condemned!!! Diet used for controlling blood sugar should meet the following criteria (Umeadi M, Chinenye S. Dietary Management of Diabetes in Nigeria 2014): (a) Should provide a balanced diet. A diet is said to be balanced if it is
able to supply all the essential nutrients, in the right quantities.
(b) Should be prepared from the traditional varieties, using food items
that can easily be found in the local environment. This is to ensure that the diet does not look or taste strange.
(c) Should maintain the pleasure that comes from eating food, so that
the person living with diabetes would enjoy it all the days of his/her life and not just for a brief period.
Diabetes Food Pyramid: The Diabetes Association of Nigeria,
American Diabetes Association, International Diabetes Federation and
other expert diabetes organizations specifically advise the following:
Fig. 19: Diabetes Food Pyramid
Carbohydrate: Carbohydrates should make up 45 - 55% of the total
calories content of the meal.
Total fat: The fat content of the diet should not provide more than 30%
of the total calories, preferably distributed into 5% saturated fatty acids,
15% monounsaturated fatty acids, and 10% polyunsaturated fatty acids.
Cholesterol: The total cholesterol in all the meals consumed in a single
day should not be more than 300 mg.
Protein: Protein should provide not more than 15% of the total calories
of the diet, and should preferably be derived from plant sources and/or
lean sources of animal protein.
Sodium chloride (salt): The salt content of all the meals eaten in a
single day should not be more than 100 mmol (approximately 5g of
salt).
Calcium: The diet should be able to provide 1,000 to 1,500 mg of
calcium in a day.
Fiber: The diet should contain a minimum total of 20 to 30g of fibre in
the meals consumed per day.
Glycaemic Index (GI) and the Glycaemic Load (GL) of foods: The
Glycaemic Index is a measure of the quality of carbohydrates contained
in the food, while the Glycaemic Load is a measure of both the quality
and the quantity of carbohydrates in the meal (consult the book titled:
Dietary Management of Diabetes 2014.)
Diet is individualized and depending on your age, weight, occupation,
food habits etc., your physician will prescribe your daily calorie
requirement while the dietician prepares the meal plan.
Physical Activity for Better Diabetes Control
In diabetes, you must increase your physical activity to give yourself
every chance to live a long and healthy life.
Increased physical activity is recommended for every diabetic patient
and various studies have found it to be very effective (Chinenye et al.
Diabetes Advocacy and Care in Nigeria 2014)
Physical activity is defined as any bodily movement produced by
muscles that result in energy expenditure which can be measured,
usually in kilocalories (Casperon et al 1985).
Physical activity in daily life is categorized into occupational, sports,
conditioning, household or other activities.
Exercise is defined as a subset of physical activity that is planned,
structured and repetitive and has a final or an intermediate health or
skill-related objective. Thus in exercise, the bodily movements are planned, structured, repetitive and with a health or skill-related objective. However, physical activity and exercise are often used interchangeably. Physical Activities (Exercises) are generally grouped into three categories: -
Aerobic exercises such as walking, cycling, jogging, running,
hiking, playing tennis etc. These have beneficial Diabetes and cardiovascular effects.
Anaerobic or Resistance exercise such as weight training. These
increase short-term muscle strength.
Flexibility exercises such as stretching. These improve range of
motion of muscles and the joints.
Health Benefits of Physical Activity
1. It improves the sensitivity of the cells of the body to insulin 2. Physical activity improves the body's metabolism – it is
3. It works to improve the body's lipid profile/cholesterol 4. Physical activity improves cardio-respiratory health through its
effects on the lungs and heart
5. Improves musculoskeletal health, through increased metabolism
and greater use of the bones, muscles and joints of the body.
Physical Activity Prescription for the Control of Diabetes
A minimum of 150 minutes of moderate to vigorous intensity aerobic
exercise each week, spread over at least 3 days of the week, with no
more than 2 consecutive days without exercise!
Diabetes Physical Activity Poem
Physical Activity improves Diabetes Health
Every little bit counts, but more is
even better – everyone can do it!
Get active your own way…
Build physical activity into your daily life
…at home
…at school
…at work
…at play
…on the way
That's Active Living!!!
POLICY AND STRATEGIES TO ACHIEVE DIABETES CARE
IN NIGERIA
Challenges to Diabetes Care in Nigeria
Most diabetes care in Nigeria is done by primary care providers.
Less than 20% of Nigerians living with diabetes ever see an
endocrinologist (core diabetes specialist) and there are not enough
endocrinologists to handle the ever increasing number of people with
diabetes in Nigeria.
The vast majority of diabetes management should still be, in the hands
of Primary care physicians who must strive to update their knowledge
and skill. One may ask, what is the current state of diabetes care and
why should we worry about doing better?
The sad fact is that health care providers – government in particular and
primary care providers – are not managing diabetes as well as it should
be!!!
The Nigerian Diabcare Study (2008) put the average Haemoglobin A1c
(HbA1c) of Nigerians living with diabetes at 8.3% which is clearly
unacceptable! Diabetes remains an enormous contributor to heart-
related disorders, as well as the most common cause of working-age
blindness, end-stage-kidney disease and limb amputations.
It is especially alarming that the grim statistics remain despite
incontrovertible evidence that overall diabetes management matters –
not just blood glucose control alone.
It is imperative to think beyond the day-to-day treatment options and
adjustments and consider our entire healthcare system and how best to
deliver especially primary care to Nigerians living with Diabetes
(Chinenye et al. Diabetes Advocacy and Care in Nigeria 2014).
The tools needed for good diabetes care are affordable as long as there
is political will and adopting the right model for implementation is
worth the effort (Chinenye et al. Diabetes and related diseases in
Nigeria: Need for improved primary care in rural communities 2014).
The assessment tools available for diabetes care are accurate and easy to
use even at the primary level.
In Nigeria, a functional National Health Insurance Scheme (NHIS) is
essential to the proper delivery of primary care to people living with
diabetes; thus the current dysfunctional NHIS with poor coverage needs
serious overhauling.
High out-of-pocket expenses and lack of access to quality healthcare,
drugs and facilities are critical barriers confronting diabetes and other
Non-communicable Diseases (NCDs) care in Nigeria.
Current Facilities in Nigeria that provide Diabetes Care
1. Primary Health Centres (PHCs): At the Local Government Areas
where there is virtually no diabetes care initiative. These PHCs mainly carry out immunizations, treat malaria etc. They lack capacity to manage diabetes; thus there is poor detection rate and ineffective referral.
There is a compelling need to integrate diabetes care into our existing PHCs because ≈60% of our populace who live in rural areas patronize PHC services. (Chinenye et al. Diabetes and related Diseases in Nigeria: Need for improved primary care in rural communities 2014) 2. Secondary Health Care Facilities: These include General Hospitals
and private medical centres. There is diabetes care in some of them, but capacity is inadequate; thus they mainly refer at a late stage.
3. Tertiary Health Care Facilities: These include Teaching Hospitals,
Federal Medical Centres and Specialist Hospitals. Most of these centres run diabetes clinic which are usually overwhelmed by a large number of diabetic patients.
Objectives of Proposed Diabetes Primary Care Model
1. To enable effective opportunistic screening for diabetes (≥40yrs,
overweight/obese)
2. Diagnosis, treatment and follow-up for patients with Diabetes and
3. Prevent and/or identify complications early. 4. When to refer patients to a specialist/tertiary centre. 5. Referral back to the nearest PHC for follow-up care for non-
6. Education of patients about lifestyle measures and specific
treatment so that individuals can take responsibility for their own care in collaboration with health professionals.
7. Usage at the:
o Primary Health Centre o Out-patient clinics of secondary health facilities o Private Clinics
Proposed Diabetes Care Model
This model has four parts as follows:
1. Consultation: This involves assessing and investigating the patient,
treating or referring them where necessary and completing a register and treatment card.
2. Lifestyle Education: This involves diabetes specific education,
support for medication adherence and setting up a treatment plan (on the 1st consultation).
3. Follow-up: This involves assessing the patient at a follow-up
appointment, 1-3 month intervals and addressing their concerns and questions.
4. Counselling: This can be done by the doctor and then with a health
educator/counsellor if available. Counselling can occur less frequently after a few consultations.
Primary Diabetes Clinic Model
Most of the burden of diabetes fall close to people's homes at primary
care level and appropriate health programmes for delivering care to
people living with diabetes in this situation are required.
A few basic principles will guide this primary diabetes clinic model (Chinenye et al. Diabetes and related diseases in Nigeria: Need for improved primary care in rural communities 2014): 1.
The primary care model should be appropriate to the local situation and resources.
2. Well supported decentralization of human and physical resources is
a priority in order to improve access to healthcare and sustain uptake of long term treatment.
3. Clear guidelines and protocols for diagnosis, risk-factor assessment
and management should be developed and adopted.
Diagnosis, treatment and education can be delivered to the patient either by professional health staff at a clinic or, once the condition is stable, continued via community or village health workers.
5. Diagnosis and initial stabilisation of the patient requires the input
of trained staff especially medical officers and nurses.
6. A dedicated diabetes clinic improves the introduction and
standardised use of protocols, increases the exposure of patients to appropriate health information, and aids routine drug ordering.
7. Protocols for diagnosis, management, assessment of complications
and clear indications for referral should be developed.
8. This clinic will not function optimally in isolation from other
healthcare services. Eventually it needs to be clearly and firmly placed within the national healthcare system and linked horizontally and vertically within the primary healthcare (PHC) programme.
9. Many Local Government Areas (LGAs) in Nigeria do not yet
have a strong diabetes care initiative, but do manage PHC services, and it will be more feasible to focus on integrating the diabetes clinic within these PHC services.
10. Where medical officers are lacking, the primary diabetes clinic
should be nurse-led with back-up as available from medical officers.
11. Health workers in PHC and their colleagues in referral institutions
should be trained together in the clinic's functioning and protocol usage. This will enhance cooperation and standardisation of care for people with diabetes.
12. One area key to the good functioning of this clinic model is drug
supply to the clinics and also to the village health personnel. Nothing discourages a patient faster from taking treatment than not finding it available!
13. The shorter the list of medications and the cheaper or more
commonly available they are, the more likely ordering is to be timely and successful. This means staying within the Nigerian essential diabetes medicines' list and limiting the number of drugs in each protocol. Although this may not give the flexibility of management some clinicians would wish for, it will at least ensure an acceptable base-line of treatment options.
Diabetes Clinic:Primary Care Model
Diagnosis of DM according to
protocol (nurse/doctor)
Provide information
about DM and its risk
factors (awareness
program)
Visit to PHC
Assess for complications/risk factors and start
treatment according to protocols
Change treatment
Nurse-led monthly follow-up and
according to protocol
treatment (unless condition is
Only if adherent with
At every clinic visit:
management
Check signs and symptoms of DM (incl. BP,
weight) Assess adherence using tablet
charts Side-effects from medication Risk
factors/behaviour change
Assess what treatment adherence
and dietary modification has been
achieved
DM controlled?
Adherent with treatment?
No side-effects?
Issue 1-3 month drug-ticket
NB: Patient can be referred
Patient or relative collects treatment monthly
for doctor's review at any
from clinic or local health worker
time
Patient review at any time if signs or symptoms
PHC = Primary Health
Clinical review 1-3
Fig. 20: Primary Care Diabetes Model
So what further can be done to help the primary care providers
succeed in caring for patients with diabetes in Nigeria?
The Diabetes Association of Nigeria [DAN] is committed to being the most accessible and reliable source of information about diabetes in Nigeria.
First, there is the DAN website, offering
easy access to information and useful references for healthcare
professionals.
Another extremely helpful source of information is the DAN's Clinical
Practice Guidelines for Diabetes Management in Nigeria which is
regularly updated.
The Association also offers many professional workshops for diabetes
care providers.
Because good diabetes care depends on a good patient self-care,
Nigerians living with diabetes must know a great deal about their own
condition and its management in order to achieve the goals.
DAN offers a number of books, publications and other information
resources for people with diabetes as well as information in culturally
appropriate formats for some ethnic groups – Ibo, Hausa, Yoruba etc.
Diabetes Association of Nigeria (DAN) as a strong and credible
member of International Diabetes Federation (IDF) that works closely
with World Health has international goodwill. This goodwill can be
harnessed by Nigerian government to expand and strengthen our
healthcare as part of our march towards achieving Universal Health
Coverage (UHC).
Country ownership and developing the capacity to create better and
stronger health system should be our main focus.
WAYS TO SUPPORT NIGERIANS LIVING WITH DIABETES
You can do a lot to support your friend, relative or spouse as they
manage their diabetes.
Encourage them. It is challenging to be afflicted with diabetes.
Treatment is life-long, thus support is essential. 1. You will need to learn the symptoms of low blood sugar
(hypoglycaemia) and high blood sugar (hyperglycaemia) and what to do about them.
2. Experts agree that nearly all diabetic patients should be on
cholesterol-lowering drugs in addition to their main anti-diabetic drugs (to prevent heart disease)
3. Remind them to check their blood sugar levels on time using
4. Offer to keep a record of their symptoms or other concerns and
agree to accompany them discuss about it with their doctor.
5. Together plan how to handle a diabetes-related emergency or
6. Support them in making good food choices and prepare healthy
7. Go with them to a diabetes support group meetings e.g. DAN. 8. Help manage medications:
People with diabetes need to take their medicines as prescribed
Sometimes, they may need a little help with that.
Make sure the person is able to self-administer the medications
Keep all their diabetes supplies in a convenient place.
9. Make Diabetes Health Services available, affordable and accessible
PREVENTION OF DIABETES
Preventive measures can be applied at any stage along the spectrum of
diabetes health with the goal of preventing development or further
progression of diabetes.
Primordial prevention: This consists of actions to minimize hazards to
health, inhibit the establishment of factors (environmental, economic,
social, behavioural, cultural) known to increase the risk of diabetes.
It addresses broad health determinants rather than preventing personal
exposure to risk factors. In other words, primordial prevention deals
with prevention of development of risk factors.
Examples include:
Establishing healthy communities.
Promoting a healthy lifestyle in childhood.
Prenatal nutrition programs.
Subsidizing fitness programmes at the sports centre
Increasing sports programmes in schools which may help
reduce obesity in the subsequent generations.
Primary Prevention
This seeks to prevent the biologic onset of diabetes via risk reduction by
altering behaviours or lifestyles that can lead to diabetes.
Examples include obesity reduction, increased physical activity,
avoiding unhealthy diet, smoking cessation etc.
Essentially, primary prevention is concerned with interventions
designed to modify adverse levels of risk factors once they are present
with the goal of preventing an initial development of diabetes.
The ultimate goal is to increase the number of years that people can
enjoy quality life and compress the time that people experience diabetes
and disability.
Secondary Prevention
This includes procedures that detect and treat pre-clinical diabetes and
thereby control disease progression. Screening procedures are often the
first step, leading to early interventions that are more cost-effective than
intervening once symptoms appear. Diabetes has a pre-clinical phase
that is not benign.
Examples – routine blood sugar testing for people over 35 years to
detect type 2 DM at the level of doctor-patient encounters or via public
health screening programs.
Tertiary Prevention
This seeks to soften the impact of diabetes on the patient's function,
longevity and quality of life.
Examples include: prosthetic rehabilitation after amputation, eye
examinations to check for possible adverse outcomes of diabetes.
Tertiary prevention assists the patient to accommodate his/her
disability.
LEVELS OF PREVENTION
Whole population
Awareness of
selected groups
through public
and healthy
High risk patients
health policy
TERTIARY
SECONDARY
PREVENTION
QUARTERNARY
PRIMORDIAL
PREVENTION
PREVENTION
PREVENTION
from unnecessary
quality of life.
Avoiding tight glucose
Advocacy for social
Interventions designed to
control in certain groups
change to make physical
modify adverse levels of
after amputation,
(elderly & children) and
activity easier.
risk factors once they are
Blood sugar testing for
watching for unnecessary
Deals with prevention of
present with the goal of
people >35years to
development of risk
preventing an initial
detect type 2 DM
fac tors before their
development of diabetes.
↑Physical activity ↓Unhealthy diet etc.
Fig. 21: Levels of Diabetes Prevention
Fig. 22: Stages of Diabetes Prevention
Pre-diabetes
Definition: This is the "grey-area" in the march towards development
of diabetes whereby the blood sugar is higher than the upper limit of
normal but not high enough as to be classified as full blown diabetes.
Those with pre-diabetes are at increased risk of developing type 2
diabetes within a decade unless they adopt a healthier lifestyle that
includes weight loss and increased physical activity.
Getting diagnosed with pre-diabetes is a serious wake-up call but it
doesn't mean one will definitely develop diabetes.
There is still time to turn things around. It is an opportunity to initiate
lifestyle changes or treatments and potentially retard progression to
diabetes or even prevent it.
The following changes in one's daily habit are a good way to start
preventing diabetes, namely:
1. Move more (life is movement)!!!
Becoming more active is one of the best things we can do to make diabetes less likely. Physical activity is an essential part of the treatment plan for pre-diabetes because it lowers blood glucose levels and decreases body fat. Ideally, one should exercise at least 30 minutes a day, five days a week. Let your doctor know about your exercise plans and ask if you have any limitations.
2. Weight reduction.
Even 5-7% weight loss can make a significant difference.
3. See your doctor often for review
- Patients like some tangible evidence of success or failure
4. Eat healthy foods
- Load up on vegetables especially less starchy types
- Add more high-fibre foods into your daily menu
- Enjoy fruits in moderation: 1-3 servings per day
- Choose whole grain foods instead of processed grains e.g.
brown rice instead of white rice
5. Make sleep a priority
- Not getting enough sleep regularly makes weight loss harder
- A sleep short-fall makes it harder for the body to use insulin
effectively, thereby enhancing probability of developing diabetes
- Set good sleep habit
- Avoid caffeine after lunch if you have difficulty sleeping
- Don't watch TV or use your PC or smartphone when you are
trying to fall asleep
- Join gym clubs
- Join Diabetes Association
7. Choose and Commit
- Having the right mind-set can help
- Accept that you won't do things perfectly everyday but pledge
to do your best most of the time
- Make a conscious choice to be consistent with everyday
activities that are in the best interest of your health.
- Make small changes overtime
MILESTONES IN DIABETES RESEARCH AND POTENTIAL
"Taking time to look back is a foundation on course to
build a stable future" – Unarine Ramaru (South African writer).
1. Discovery and characterization of Islet cells by Paul Langerhans
in 1869 in Germany.
2. Discovery of insulin in 1921 by Fredrick Banting, James Macleod,
Charles Best and James Collip in University of Toronto, Canada.
3. April 2007: New type 2 diabetes genes identified.
This discovery dramatically boosted scientists' understanding of
risk factors for diabetes. Since then, researchers have spotted more
than 70 gene variants that raise diabetes risk by up to 30%
(WebMD 2015: . Most of these affect the
release of insulin, the hormone that controls blood sugar levels.
4. Pancreas transplantation
- An organ donor's pancreas is transplanted into someone with
- In some patients, a pancreas transplant cures diabetes.
5. Islet cell Transplantation
- Insulin-producing cells are harvested from an organ donor's
pancreas and transplanted into someone with type 1 diabetes.
- This is still an experimental treatment but can potentially cure type 1
6. Herbal (Alternative) treatment
There are lots of herbal agents claimed to control and treat diabetic
patients, but total cure from diabetes has not been reported or confirmed
till date using Herbs.
In addition to side-effects (adverse effects), drug treatment have limitations in maintaining normal blood sugar and preventing late stage diabetic complications.
Several medicinal plants have been investigated for their beneficial effects in different types of diabetes e.g. vernonia amygdalina (Bitter leaf), Galega officinalis (Goat's rue or botanical root of metformin) etc. Over 800 plants have been reported to have anti diabetic properties but none has sustainable effects and currently are not useful in lowering the blood sugar to the optimal extent as insulin and other proven anti-diabetic drugs (Chinenye et al, Diabetes Advocacy and Care in Nigeria: Herbal medicine as potential source for anti-diabetic drugs 2014).
Chemical constituents of Anti-Diabetic Herbs
These are (Gupta et al 2012):
1. Sesquiterpene (Bitters) 2. Mormordicin 3. Lectin 4. Glycosides 5. Terpenoids 6. Cytotoxic momorcharin and momordin 7. Beta-carotene 8. Flavonoids (apigenin) 9. Taraxacin
10. Alkaloids e.g. lutein, luteoline, galegine. 11. Galegine study ultimately led to discovery of metformin
(Glucophage) in the 1950s.
12. Anthocyanoside (myrtillin)
Plants have always been an important source for finding new medicines for human diseases. Among the hundreds of plants that have been tested for diabetes, only small fractions have been tested in animal studies and no phase 4 or 5 Human Studies.
Although an array of plants have been claimed to have blood sugar
lowering effects, it is better to allow science guide us i.e until scientific
evidence are available to support their anti-diabetic effects devoid of
toxicity.
Proposed Recommendation before Diabetes Association of Nigeria:
"If there is proven clinical evidence for anti-diabetic effects of Nigerian
Herbs, should physicians rely on these herbs, at least as complementary
therapeutic agents, along with current orthodox anti-diabetic drugs to
improve management of diabetic patients"? (Oputa RN, Chinenye S.
Diabetes in Nigeria – a translational medicine approach 2015)
Isolation and identification of active constituents from Nigerian herbs, preparation of standardized dose and dosage regimen can play a significant role in improving Diabetes management (Chinenye S, Abo K, Suleiman M. Chike P, Siminialayi IM. Anti-diabetic Research Using African Medicinal Plants - work in progress)
7. Bariatric Surgery versus Cure for Diabetes
Despite what experts are calling remarkable results, they are not saying
weight loss surgery is a cure.
Bariatric surgery is not for everyone with diabetes. The patients must be selected by the physicians.
Remission is said to occur when a person with type 2 diabetes achieves blood sugar levels no longer in the diabetes range without medications for at least 1 year.
Bariatric Surgery: Pros and Cons
The surgery works if post-surgery clients still practise lifestyle changes such as healthier diet and exercise.
Even after substantial weight loss, diabetes does not remit if diabetes duration is more than 4 years. a. Cells in the pancreas called the beta cells that make insulin
die off over time and cannot be replaced.
b. If a large chunk of the beta cell population has been lost,
benefit from bariatric surgery cannot be guaranteed.
The average cost of weight loss surgery ranges from $11,500 - $26,500 which makes it expensive.
Three procedures are common: - Bypass
- Gastric sleeve
Side-effects of bariatric surgery are weight regain, malnutrition, nausea, bloating, vomiting, gall stones and lack of certain vitamins e.g. B12
Indications for Bariatric Surgery in Type 2 DM
(a) BMI ≥ 35kg/m2
(b) Failure to lose weight by traditional methods.
(c) Had diabetes for less than 4 years
(d) Failed medical treatment. Not recommended as 1st line
8. June 2014: First Artificial [Bionic] Pancreas developed: Scientists
made a bionic pancreas that tracks blood sugar levels and automatically
pumps the correct amount of insulin and glucagon into the blood. By
mimicking the action of a real pancreas, the device can help people with
type 1 diabetes avoid constant blood sugar monitoring and manual
insulin injections.
Developed by a collaborative team from Boston University and
Massachusetts General Hospital, working together to make automated
blood glucose control a reality.
Bionic pancreas system uses continuous glucose monitoring along with subcutaneous delivery of both rapid-acting insulin (to lower blood glucose) and glucagon (to raise blood sugar) as directed by a computer algorithm. The bionic pancreas automatically makes a new decision about insulin and glucagon dosing every five minutes – that is 288 decisions per day, 7 days per week and 365 days per year.
Fig. 23: Components of Artificial (Bionic) Pancreas (Source: www.bing.com/images)
9. Stem Cell Research and Cure for Diabetes
Harvard University Stem Cell researchers have produced massive
quantities of Human-insulin-producing beta cells (Diabetes Voice. Dec
2014).These Stem Cells cured diabetes when transplanted in mice
within two weeks. This is acclaimed to be 50% of the solution to the
problem facing people living with Type 1 diabetes today.
The other remaining half of the solution involves developing an
implantable device to install and protect the beta cells from rejection by
the immune system of the recipient. Currently, the Harvard group and
MIT department of Applied Biology are working to design an
implantable device (William R. et al. Diabetes Voice 2014).
Should a cure be our primary target for diabetes?
Based on basic and clinical facts about diabetes, when "cure" comes
(and it surely will), it is likely to be multiple:
- Different cures for type 1, type 2 etc.
- Perhaps different cures for diabetes at different stages. The only thing of which we can be reasonably certain is that there will not be just one cure which will be effective for all. Diabetes is not a single disease but is a clinical syndrome that includes multiple diseases that have different aetiologies (causes), pathogeneses and rates of progression, thus may require different therapeutic approaches. This is the inarguable state of affairs in Diabetes Research.
Acceptance of this fact will greatly save our patients and influence the
prioritization of life transformative treatments that hold the potential
to profoundly transform and improve life with diabetes.
Instead of an imaginary and unconfirmed claim from alternative care
providers, it may be the case that something short of a "cure" is what
patients need for now!!!
While the concept of a cure is motivating, I believe the claim of an
‘unproven cure' by alternative care providers including herbalists
derail and distract our patients from seeking scientific treatment
advances that reduce the burden of diabetes, improve health outcomes
and ultimately restore physiology.
The right question to ask may be:
What does the person living with diabetes consider as Favourable or successful treatment?
Is it a permanent restoration of normal physiology that a person with diabetes wants or is it a safe, easy and cost-effective way to eliminate the symptoms of diabetes and its complications?
The former will take many decades to achieve but the latter is achievable through a variety of treatment approaches that are already being accomplished.
As a general rule, any discoveries happening in academia should be thought of at least 10-20 years away from any opportunity for broad clinical application. (Brewer J et al. 2014) While we continue to pursue the appealing concept of cure for diabetes, we should not lose touch with reality by committing to what is possible now!!!
Take Hom
e Message
Until there is a scientifically confirmed cure, use the latest
and the best proven therapy in d iabetes care!!!
SUMMARY OF MY ACADEMIC/PROFESSIONAL
(A) Research
My research interests have focused on areas of Endocrinology &
Metabolism
Dyslipidaemia) and HIV/AIDS. Papers from these have been presented and published in local, national and international journals of repute including Gut, Scandinavian Journal of Gastroenterology, Ethnicity & Disease, Vascular Health and Risk Management Journal, Archives of Diabetology and Cardiovascular Medicine, Pakistan Journal of Medical Sciences, Mera Diabetes International, Journal Sexual Medicine, Journal of the College of Physicians and Surgeons Pakistan, International Archives of Medicine, Nigerian Medical Practitioner, Indian Journal of Endocrinology & Metabolism, The Nigerian Health Journal, Port Harcourt Medical Journal, Journal of Social Health and Diabetes, Nigerian Journal of Orthopaedics & Trauma, BMC Endocrine Disorders, Nigerian Endocrine Practice etc. I have published over 40 Researched articles in peer-reviewed journals within and outside Nigeria. Along with senior colleagues in the department, we have motivated the younger physicians to do research. Some of our efforts have culminated in the completion of training of these young physicians who are now lecturers either in UNIPORT or other tertiary institutions in Nigeria. I am a principal author in 6 (Six) and a co-author in 3 (three) books namely; 1. National Clinical Practice Guidelines for Diabetes Management in
Nigeria (principal author, maiden edition).
2. Living with Diabetes in Nigeria (co-author, A Practical Manual of
3. HIV&AIDS: The Niger-Delta Perspective (principal author). 4. Challenges Associated with the Effective Management of HIV
infection in a Low income Setting in Sub-Saharan Africa: Case Study of Nigeria (co-author).
5. Lecture Notes & Essays in Internal Medicine with Multiple Choice
Questions (principal author, Volume I).
6. Lecture Notes & Essays in Internal Medicine with Multiple Choice
Questions (principal author, Volume II).
7. Clinical Practice Guidelines for Diabetes Management in Nigeria
(principal author, 2nd edition)
8. Diabetes Advocacy and Care in Nigeria (principal editor).
9. Dietary Management of Diabetes in Nigeria (co-author).
(B) Medical Education:
From my early years as lecturer I up to the current professorial chair, I
have actively participated in medical education, teaching both
undergraduate students and postgraduate doctors. I have participated
actively in organizing national medical conferences. My efforts in the
Endocrinology unit along with those of my colleagues have been
rewarded with the training of consultant Endocrinologists with a
number of senior residents now undergoing subspecialty specialization
in Endocrinology & Metabolism. In recognition of my outstanding
contributions in the manpower training I have received several awards
from Resident doctors and other professional societies.
(C) University/Professional/Community Activities:
I am a reviewer of a number of medical journals which include the
African Journal of Endocrinology & Metabolism, Archives of
Diabetology & Cardiovascular Medicine, The Nigerian Health Journal,
Nigerian Endocrine Practice etc. I am an external examiner in medicine
in some Nigerian Universities as well as the West African College of
Physicians.
In 2006, I linked the University of Port Harcourt Advancement Centre (currently called Uniport Foundation) with Lund University in Sweden. Two (2) lecturers from our college benefited from that program. I had earlier received training and done a collaborative research with Lund University Hospital, Sweden. I led the medical team of the FGN pilgrims to the Holy Land
(Jerusalem) in December 2003.
An active member of the College Building Committee that
submitted architectural blueprint and raising fund for a befitting college building.
Contributed in developing the current MPH programme in
community medicine.
Was acting Head of Department (HOD), Internal Medicine, from
2009 – 2012 and created more specialty units in department of medicine.
Elected National President of Diabetes Association of Nigeria in
2009 and under my leadership produced the 1st Edition of NATIONAL
DIABETES MANAGEMENT IN NIGERIA. It was an award winning publication during the World Diabetes Congress in Dubai, UAE 2011, following assessment by an International Committee of International Diabetes Federation/World Health Organization (IDF/WHO)
Currently initiated linkage between Uniport and Manchester
University, UK for Research collaboration. The Manchester Group visited the University of Port Harcourt recently.
Has designed, executed and published studies with colleagues in the
college as well as colleagues at the national level to determine, evaluate and improve Diabetes Care in Nigeria.
Coordinates the HIV/AIDS programme in UPTH and published a
monograph on HIV/AIDS treatment with its peculiarities in the Niger Delta Region, which is currently used for training.
Set up Non-communicable Diseases Research Group in the
Department of Medicine, College of Health Sciences with academic colleagues.
We are currently working on Grant Proposals.
Currently Nigerian representative in International Diabetes
Federation (IDF - based in Brussels) by virtue of being the President, Diabetes Association of Nigeria.
CONCLUDING REMARKS
Recommendations towards Diabetes Care & Support in Nigeria
(A) To Nigerians Living with Diabetes
o Be positive and live positively with diabetes.
o Get the right information about diabetes and its management
o Always adhere to the recommendations given by qualified and well
trained healthcare providers.
o Take your drugs as prescribed o Comply with appointments with your care givers o Abide by the recommendations with regards to lifestyle:
• Diet • Exercise • Cessation of smoking • Intake of alcohol
o Monitor relevant parameters like:
• Glucose (HBA1c; Fasting and 2 Hrs post meal glucose) • Blood Pressure • Cholesterol • BMI, Waist Circumference, waist to hip ratio
o Perform regular checks on your:
• Feet • Eyes • Kidneys • Etc.
(B) To the Care-givers:
o Be empathic to the patients not judgmental.
o Treat them holistically i.e.: treat not just blood sugar but also BP,
o Take into serious consideration their psychosocial needs and factor
them in the overall care plan
o Above all make yourself available and accessible to the PLWD
Provide them with your contacts numbers so that you can be
reached in case of emergency or need to clarify some issues.
Do not see the PLWD as "pests" but as people you have been
trained to provide care for.
o Update yourself with current trends in the management of diabetes
so that the quality of care you give to PLWD will be appropriate & adequate.
(C) To the Government:
o Develop and implement a policy towards Diabetes Care in Nigeria
o The policy should be aimed at meeting the yearning needs of
PLWD and ensure that they are adequately catered for by: Ensuring that relevant diabetes care products especially drugs
are free of charge or at least subsidized
Ensuring that insulin is given free of charge to ALL PLWD as
done in many other countries.
Ensuring that the National Health Insurance provides sufficient
cover for all round diabetes management.
o Government should provide diabetes centers of excellence across
the country where PLWD could go to for world class care.
(D) To Non-Governmental Organizations
The NGOs should:
o Form a strong pressure group to push government towards
developing and implementing a diabetes care policy for the country.
o Should be actively involved in the development of such policies and
also ensure that the policies once developed are appropriately implemented.
o Should serve as a rallying point for all PLWD in Nigeria and they
should at all-time defend their interest.
o Should discard the cloak of self-centeredness and replace it with the
cloak of selflessness and service to humanity.
(E) To Corporate Organizations:
(e.g. pharmaceutical companies, Foundations etc.)
o They should devote a portion of their earnings towards helping the
course of diabetes care in Nigeria. This could be a part of their Corporate Social Responsibility.
o They should set foundations with a bias towards diabetes care.
o They should actively be involved in sponsoring diabetes related
activities like DAN conferences, Endocrine Society conferences and other diabetes related seminars in Nigeria.
DIABETES EPILOGUE
Diabetes is not a death sentence
I still have the opportunity to live a long and healthy life
The life ahead may be Hard and Difficult
But I will face it with courage and dedication
To ensure that diabetes does not subtract even a month from my life
I will do all that is required
To live long and healthy, inspite of the disease
I will do it for myself & for my loved ones
I must fight to remain alive and healthy,
To achieve my life ambitions, and
To continue to be a blessing to All
So help me God!!!
(Culled from the Book: 101 Ways to live a long and healthy life with
Diabetes Mellitus)
References
1) Wilson JD. The Evolution of Endocrinology. Plenary Lecture at the 12th
International Congress of Endocrinology, Lisbon, Portugal, 31st August 2004. ClinEndocrinol. 2005;62(4): 389-396.
2) Brown-Séquard CE. Du role physiologique et therapeutique d'un suc
extrait de testicules d'animaux d'apres nombres de faits observe chez
l'homme. Archives de Physiologie Normale et Pathologiques 1889; (5e
ser) : 1739–1746.
3) Starling EH. The chemical regulation of the secretory process (Croonian
Lecture to the Royal Society). Proceedings of the Royal Society 1904;
73B: 310–322.
4) Jameson JL (ed). Principles of Endocrinology. In: Harrison's
Endocrinology (3rd edition). New York, McGraw Hill 2012.
5) IDF Diabetes Atlas. 6th Edition. International Diabetes Federation, 2013.
Available at: http//www.idf.org/diabetesatlas
6) World Health Organization (WHO). Definition, Classification and
Diagnosis of Diabetes. Geneva, WHO 1999 & 2006.
7) Chinenye S, Phillip-Ephraim EE, Young EE. Lecture Notes & Essays in
Internal Medicine with Multiple Choice Questions & explanatory answers (Volume I: Endocrinology, Diabetology & Metabolism) Port Harcourt, Nigeria: University of Port Harcourt Press; 2013.
8) Chinenye S., Onyemelukwe GC, Johnson TO et al. Diabetes Advocacy
and Care in Nigeria. Port Harcourt, Nigeria: Diabetes Association of Nigeria; 2014.
9) Chinenye S, Ofoegbu EN, Onyemelukwe GC et al. Clinical Practice
Guidelines for Diabetes Management in Nigeria (2nd edition). Port Harcourt, Nigeria: Diabetes Association of Nigeria 2013.
10) Ogbera AO, Fasanmade O, Chinenye S, Onyekwere C. Characterization
of Newly Registered Patients with Diabetes Mellitus in an out Patient
Facility in Nigeria. Nigerian Endocrine Practice 2007; 1 (3): 19-28.
11) Chinenye S, Ogu R, Akhidue K. Diabetes In Pregnancy: The Nigerian
Perspectives using the new WHO criteria. Indian J EndocrMetab 2014 (in press).
12) Institute of Medicine. Living well with chronic illness: A call for Public
Health Action. Washington DC20001.National Academy of Sciences 2012.
13) Ogbera AO, Fasanmade O, Chinenye S, Onyekwere C. Characterization
of Newly Registered Patients with Diabetes Mellitus in an out Patient Facility in Nigeria. Nigerian Endocrine Practice 2007; 1 (3): 19-28.
14) Uloko AE, Gezawa ID, Muhammad FY, Habibu RA, Ramalan MA,
Muhammed AA et al. Dysglycaemia among HIV patients on Highly active Anti-retroviral
EMSON/2014/019 (BENIN 2014 Conference); 36:pg43.
15) Ogbera AO, Kapur A, Chinenye S, Fasanmade O, Uloko A, Odeyemi K.
Undiagnosed diabetes mellitus in tuberculosis: A Lagos report. Indian J EndocrMetab 2014;18:475-9.
16) Ogbera AO, Chinenye S, Fasanmade AO, Akinlade A. Characterization of
Lipid Parameters in Diabetes Mellitus – A Nigerian Report. International Archives of Medicine 2009; 2 (1) 2-19 (Doi-10.1186/1755-7682-2-19).
17) Ogbera AO, Chinenye S, Onyekwere A, Fasanmade O. Prognostic
indices of Diabetes Mortality. Ethnicity & Disease 2007; 17: 721-725.
18) Chinenye S, Ogbera AO. Current Concepts in the Management of
Diabetes Mellitus. TNHJ 2006; 6 (3/4): 383-390.
19) IDF Africa Region. Type 2 Diabetes Clinical Practice Guidelines for Sub-
Saharan Africa. Tanzania. IDF Africa-WDF 2006.
20) Chinenye S, Ogbera AO, Kalra S. Patient-centered Care in Diabetology:
sub-Saharan African perspective. AJDM 2014; 22(1):5-8.
21) Funnel MM, Brown TL. National Standards for Diabetes Self-
management Education. Diabetes Care Jan 2010. doi:10.2337/dc10-S089. Vol 33 No.supplement1 S89-S96.
22) Norris SL, Lan J, Smith SJ, Schnid CH, Engelgan MM. Self-management
education for adults with type 2 diabetes: a meta-analysis on the effect on glycaemic control. Diabetes Care 2002, 25:1159-1171.
23) World Health Organization (Regional Office for South-East Asia). Self-
care in the Context of Primary Health Care. Report of the Regional Consultation Bangkok, Thailand, 7 – 9 January 2009.
24) Umeadi M, Chinenye S. Dietary Management of Diabetes in Nigeria. Port
Harcourt, Nigeria: Diabetes Association of Nigeria; 2014.
25) Casperon CJ, Powell KE, Christenson GM. Physical activity, exercise and
physical fitness: definitions and distinctions for Health-related Research. Public Health Rep 1985; 100:126-131.
26) Chinenye S. The Current Classification and Diagnostic Criteria for
Diabetes Mellitus. NJM 2002; 11(2): 84-86.
27) Chinenye S, Uchenna DI, Unachukwu CN, Ogbera AO, and Ojule AC.
The Pattern of Diabetes Mellitus in Rivers State, Nigeria. Nigerian Endocrine Practice 2008; 2 (2) 87-93.
28) Chinenye S, Uloko AE, Ogbera AO et al. Profile of Nigerians with
diabetes mellitus – Diabcare Nigeria study group (2008): Results of a multicenter study. Indian J EnocrMetab2012; 16:558-64.
29) Ekere AU,Chinenye S, Dodiyi-Manuel A. The Diabetic Foot – A Review.
Nigeria Journal of Orthopaedics and Trauma. 2003; 2(1): 4-10.
30) Unachukwu C, Babatunde S; Chinenye S Peripheral Neuropathy in
Diabetics with Foot Ulcers in Port Harcourt, Nigeria. Nigerian Journal of Orthopaedics and Trauma 2004; 3(2):214-224.
31) Chinenye S, Young EE, Onwuchekwa AC. Diabetes Mellitus in the
elderly-Niger Delta Experience. Arch Diab& Cardio Med; 2012 March issue: 7-11.
32) Chinenye S, Ogbera AO. Socio-cultural aspects of diabetes mellitus in
Nigeria. Journal of Social Health and Diabetes 2013; 1(1): 15-20.
33) Chinenye S, Oputa RN, Oko-Jaja RI. Diabetes and related diseases in
Nigeria: Need for improved primary care in rural communities. Res. J. of Health Sci 2014; 2(2):99-107.
34) Gupta PD, De A. Diabetes mellitus and its Herbal Treatment. International
Journal of Research in Pharmaceutical and Biomedical Science 2012;3(2):706-721
35) Oputa RN, Chinenye S. Diabetes in Nigeria – a translational medicine
approach. AJDM 2015; 23(1):7-10.
37) William R. Harvard Team gets one step closer to cure. Diabetes Voice
38) Brewer J. Should a cure be our primary target for Type 1 diabetes?
Diabetes Voice 2014;59(4):22-24.
39) Chinenye S, Unachukwu CN, Hart A. Diet and Diabetes: Theory and
Practice for Care Providers. Mera Diabetes international May 2007; 15
(1): 9-11.
40) Ogbera AO, Chinenye S, Akinlade A. insulin injection Practices in People
with Diabetes Mellitus. African Journal of Endocrinology and Metabolism
2008; 7 (1) 12-15.
41) Unadike BC, Chinenye S Knowledge, Awareness, and Impact of Diabetes
among Adolescents in Uyo, Nigeria. Mera Diabetes International May 2009; 12-14.
42) Ogbera AO, Chinenye S, Akinlade A, Eregie A, Awobusuyi J. Frequency
and Correlates of Sexual Dysfunction in Women with Diabetes Mellitus. J
Sex Med 2009;6:3401-3406.
43) Chinenye S, Young E. Management of Diabetes Mellitus in Developing
Countries: The Relevance of Postprandial Hyperglycaemia. Pak J Med Sci
2011;27(3):677-681
44) Chinenye S, Young E.- State of Diabetes Care in Nigeria – A Review. The
Nigerian Health Journal 2011; 11(4):101 – 109
45) Ogbera AO, Chinenye S, Fasanmade O, Ajala W. Hypogonadism and
Subnormal Total Testosterone Levels in Men with Type 2 Diabetes
Mellitus. Journal of the College of Physicians and Surgeons Pakistan
2011; 21(9): 517-521.
46) Young EE, Chinenye S, Unachukwu CN. Beta Cell Response to a mixed
meal in Nigerian patients with type 2 diabetes. BMC Endocrine Disorders
2012; 12(11): 1472-6823
47) Chinenye S, Ogbera AO, Young EE. Prevention and Control of non-
communicable diseases in Nigeria: Challenges and strategic directions. Arch Diab& Cardio Med; 2012 March issue: 12-20
48) Oputa RN, Chinenye S Diabetes Mellitus: a global epidemic with
potential solutions. African Journal of Diabetes Medicine 2012; 20(2): 33-
35
49) Chinenye S, Young EE. Isolated postprandial hyperglycemia in type 2
diabetic patients in a Nigerian Tertiary Health Center. Indian J
EndocrMetab 2012; 16(4): 604-608.
50) Chinenye S, Young EE. Diabetes Conversation Map in Nigeria: A New
socioeducational tool in diabetes care. Indian J EndocrMetab 2013;17:1009-11.
51) Chinenye S, Anah CO &I hekwaba AE. Thyrotoxicosis in the Niger Delta
Region – Port Harcourt Experience. Nigerian Medical Practitioner 2006;
49(3): 59-63.
52) Ordinioha B, Brisibe S. 101 Ways to Live a Long and Healthy Life
with Diabetes Mellitus. Port Harcourt, Nigeria: Preventive and Public Health Consult, 2015.
CITATION
Of
PROFESSOR SUNDAY CHINENYE
MBBS (Ibadan), FWACP, FACE, FNSEM
Sunday Chinenye, a Professor of Medicine and Endocrinology, is a 1987 Bachelor of Medicine and Bachelor of Surgery (MBBS) graduate of the premier University of Ibadan, Ibadan. He holds the post-graduate fellowship degree of the West African College of Physicians in Internal Medicine and Endocrinology. He is also a fellow of the American College of Endocrinology and Nigerian Society of Endocrinology. His core research interests are Internal Medicine, Endocrinology, Advocacy and HIV Medicine. He hails from Akwete-Ndoki, an ancient town of Ndoki Ethnic Nationality, the origin of the popular Akwete cloth, a border town between Rivers and Abia States, bisected by a major river emptying into the Atlantic Ocean and also running through Opobo and Andoni.
Through this major river, Akwete-Ndoki became a major colonial town and famous sea-route through which even the famous King Jaja of Opobo as a slave boy was routed to Igbani land. The relics are there till date. It is often said that the story of Igbani land is not complete without Ndoki and vice versa. He attended Christ Church School, Akwete-Ndoki and had his secondary education at Ndoki Grammar School, Ndoki. He was nurtured and brought up by his devout Christian parents (all of blessed memory), grew up in his hometown where he was groomed with the ethics and traditions of his people. He embarked upon a highly distinguished medical career at the University of Ibadan in 1981 and finished at a record time in 6 years before proceeding for his post-graduate medical education. He is an Honorary Consultant Physician/Endocrinologist /Diabetologist; the coordinator of Anti-Retroviral programme in University of Port Harcourt Teaching Hospital; the National President, Diabetes Association of Nigeria; a Royal High Chief of Umuihueze-Akwete ancient kingdom and Justice of Peace. He was the acting Head, Department of Internal Medicine, University of Port Harcourt from December 2009 – Feb 2012.He has been an associate editor and now a reviewer for several local and international journals. An examiner at the West African Post Graduate Examinations, he has over 40 published articles in local and international journals to his credit in addition to 8 books and Chapter in a book. He has served in several committees and boards in the University. Prof. Sunny Chinenye is an external examiner in Internal Medicine to various Nigerian Universities. Having practiced the noble medical profession for over 28 years now, Professor Chinenye rose through a series of professional ranks which has made him widely respected and valued for his contributions to academics and public life. He has made sustained and original contributions in several important fields that fundamentally impact upon the quality of life in the society, namely: Academics, Health and Social care, social justice, education and
training. One of those leading roles was and still as the National
President of Diabetes Association of Nigeria. He has received
acknowledgement from a number of the Nation's eminent public figures
familiar with his works coupled with awards and laurels. His selfless
determination have touched and immeasurably improved the lives of
many people, particularly Nigerians living with diabetes, the vulnerable,
the disabled and the disadvantaged.
In addition to giving valuable service to the society, Professor Chinenye
has an inspirational vision and sustained expert knowledge. Professor
Sunny Chinenye is happily married to a beautiful wife and he is a father
of four lovely children. His first daughter just graduated with a 1st class
(special Honours) in Computer Science and currently serving the NYSC
programme.
Vice-Chancellor Sir, ladies and gentlemen, it is therefore with great
pleasure that I present this erudite scholar, Professor Sunday Chinenye
to deliver the 126th Inaugural Lecture of the University of Port Harcourt.
Thank you and God Bless!!
Professor IM Siminialayi
Dean, Faculty of Basic Medical Sciences
Source: http://www.uniport.edu.ng/files/126InauguralLectureUpdated2.pdf
2. AusgAbe, JAhrgAng 2013 MontAg, 8. April 2013 AMtliche Mitteilung Auflassung VS Selker Volksschule & Kindergarten nach Schuljahr 2013/14 geschlossen In den letzten Jahren beschäf- len, ist Selker unter den betrof- menten den auch notwendigen tigte sich der Gemeinderat stets fenen Einrichtungen. Bereits in Stellenwert einzuräumen. "Sie
Developments in International Commercial Mediation: USA, UK, Asia, India and the European Union By Danny McFadden LLM, FCIArb This paper will look at some of the major developments in international commercial mediation to date but the author would ask the reader to bear in mind that the picture is constantly changing which reflects the adaptability and dynamism of mediation in the modern era.