Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Surf-1.org
What Is Prostate Cancer?
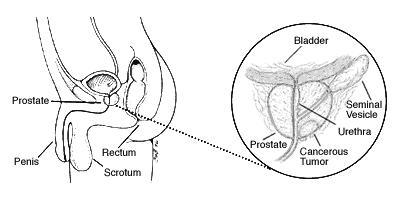
The prostate
The prostate is a gland found only in men. As shown in the picture below, the prostate is just below the bladder and in front of the rectum. It is about the size of a walnut. The tube that carries urine (the urethra) runs through the prostate. The prostate contains cells that make some of the fluid (semen) that protects and nourishes the sperm.
The prostate begins to develop before birth and keeps on growing until a man reaches adulthood. Male hormones (called androgens) cause this growth. If male hormone levels are low, the prostate gland will not grow to full size. In older men, though, the part of the prostate around the urethra may keep on growing. This causes BPH (benign prostatic hyperplasia) which can result in problems passing urine. BPH is a problem that must be treated, but it is not cancer.
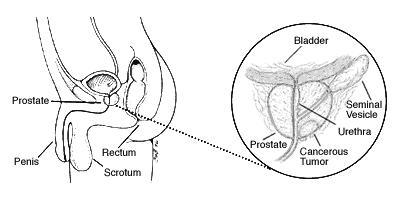
Prostate cancer
There are several cell types in the prostate, but nearly all prostate cancers start in the gland cells. This kind of cancer is known as adenocarcinoma. The rest of the information here refers only to prostate adenocarcinoma.
Most of the time, prostate cancer grows slowly. Autopsy studies show that many older men (and even younger men) who died of other diseases also had prostate cancer that never caused a problem during their lives. These studies showed that as many as 7 to 9 out of10 men had prostate cancer by age 80. But neither they nor their doctors even knew they had it.
Precancerous changes of the prostate
Some doctors believe that prostate cancer begins with very small changes in the size and shape of the prostate gland cells. These changes are known as PIN (prostatic intraepithelial neoplasia). Almost half of all men have PIN by the time they reach 50. In PIN, there are changes in how the prostate gland cells
look under the microscope, but the cells are basically still in place –they don't look like they've gone into other parts of the prostate (like cancer cells would). These changes can be either low grade (almost normal) or high grade (abnormal).
If you have had a prostate biopsy that showed high grade PIN, there is a greater chance that there are cancer cells in your prostate. For this reason, you will be watched carefully and may need another biopsy.
What Causes Prostate Cancer?
Prostate cancer is caused by changes in the DNA of a prostate cancer cell. DNA makes up our genes, which control how cells behave. DNA is inherited from our parents. A small percentage (about 5%to 10%) of prostate cancers is linked to these inherited changes. Prostate cancer may also be linked to higher levels of certain hormones. High levels of male hormones (androgens) may play a part in prostate cancer risk in some men. Some researchers have noted that men with high levels of a hormone called IGF1 are more likely to get prostate cancer, too. But others have not found such a link. More research is needed in this area.
While we do not yet know exactly what causes prostate cancer, we do know that certain risk factors are linked to the disease. A risk factor is anything that increases a person's chance of getting a disease. Different cancers have different risk factors. Some risk factors, such as smoking, can be controlled. Others, like a person's age or family history, can't be changed.
But risk factors don't tell us everything. Many people with one or more risk factors never get cancer, while others with this disease may have had no known risk factors. For some of these factors, the link to prostate cancer risk is not yet clear.
Risk factors for prostate cancer
Age: Age is the strongest risk factor for prostate cancer. The chance of getting prostate cancer goes up quickly after a man reaches age 50. Almost 2 out ofevery3 prostate cancers are found in men over the age of65.
Race: For unknown reasons, prostate cancer is more common among African American men than among men of other races. African American men are also more likely to have a more advanced disease when it is found and are more likely to die of the disease. Prostate cancer occurs less often in Asian American and Hispanic/Latino men than in non Hispanic whites. The reasons for these racial and ethnic differences are not clear.
Nationality: Prostate cancer is most common in North America, northwestern Europe, and a few other places. It is less common in Asia, Africa, Central and South America. The reasons for this are not clear. More testing in some developed countries likely accounts for at least part of this difference, but other factors are likely
to be important, too.
Family history: Prostate cancer seems to run in some families. Men with close family members (father or brother) who have had prostate cancer are more likely to get it themselves, especially if their relatives were young when they got the disease.
Genes: Scientists have found several inherited genes that seem to raise prostate cancer risk, but they probably account for only a small number of cases overall. Genetic testing for most of these genes is not yet available, and more study is needed in this area.
Diet: The exact role of diet in prostate cancer is not clear, but several different factors have been studied. Men who eat a lot of red meat or high fat dairy products seem to have a greater chance of getting prostate cancer. These men also tend to eat fewer fruits and vegetables. Doctors are not sure which of these factors causes the risk to go up.
Obesity: Most studies have not found that being obese (having a high amount of extra body fat) is linked with a higher risk of getting prostate cancer. Some, but not all, studies have found that obese men may be at greater risk for having more advanced prostate cancer and of dying from prostate cancer.
Exercise: Exercise has not been shown to reduce prostate cancer risk in most studies. But some studies have found that high levels of physical activity, particularly in older men, may lower the risk of advanced prostate cancer. More research in this area is needed.
Infection and inflammation of the prostate: Some studies have suggested that
prostatitis (inflammation of the prostate gland) may be linked to an increased risk of
prostate cancer, but other studies have not found such a link.
Some researchers have also looked at whether sexually transmitted infections might
increase the risk of prostate cancer. So far, studies have not agreed, and no firm
conclusions have been reached.
Treatment of Prostate Cancer
Diagnosis
The diagnosis of cancer of the prostate is made by biopsy of the prostate. This is most
commonly done in either the office or the operating room using a fine needle guided by
ultrasound.
At present, the majority of cancers are diagnosed after an evaluation for elevation of
prostate specific antigen [PSA]. PSA is a substance detected by a blood test, which
is often elevated in prostate cancers and frequently in other disorders of the prostate. Occasionally, firmness or nodularity of the prostate, detected on rectal exam, may suggest cancerous change and precipitate a biopsy. "Localized" cancers refer to those that appear to be contained within the prostate gland. "Advanced" or "metastatic" cancers are those where spread outside of the prostate is determined.
Tumor Stage and Grade
The Grade of the cancer relates to the appearance of the cancer cells under the
microscope, and is determined by the pathologist. Cancer cells that resemble normal
prostate gland cells are referred to as "low-grade" or "well-differentiated" cancers, while
those which have a more bizarre appearance are referred to as "high-grade" or "poorly
differentiated" tumors. Tumors falling in between are referred to as "moderately
well-differentiated." In general, poorly differentiated tumors are felt ot behave more
aggressively than well-differentiated or moderately well-differentiated tumors.
Gleason Grade and Score: The pathologist examines groups of cancer cells within the
tumor and identifies the dominant patterns of cancer cells in the specimen. He then
assigns each group a grade from 1 to 5 – 1 being well-differentiated tumor, and 5 being
poorly differentiated. These grades are known as the "Gleason Grades." The grades
of the two most prevalent patterns are then added together to give the "Gleason Score"
or "Gleason Sum" of the tumor. This number is usually expressed as a sum [e.g. –
"3+3," "4+3," "5+4," etc.] There is a rough correlation between the aggressiveness of a
cancer and a higher Gleason Score. As the system has evolved in recent years,
Gleason Sums of 3+3 – well differentiated cancers – are the most common,and scores
lower than this quite unusual. Occasionally the pathologist will see three patterns and
lists the most predominant pattern first, followed by the next most prominent, followed by
the third pattern. Therefore a sum might be 4+3 with a third pattern 5
The Stage of the cancer refers to its extent, which may be suggested on physical
examination, and may be further assessed by imaging studies – bone scans and CT
scans.
Treatments for Prostate Cancer
Treatment of prostate cancer is based on the extent of the tumor, the age and condition
of the patient, the patient's life expectancy, and the patient's level of comfort with various
treatment choices. Cancer which is localized – limited to the prostate gland – is often
curable; cancer which has spread outside of the prostate is not curable, but is often
treatable and controllable for many years. Unlike some cancers, prostate cancer tends
to spread very slowly in most cases. Additionally, it spreads in a fairly predictable
manner – first to the lymph nodes of the pelvis and those around the body's major blood
vessels, and then to the bones of the pelvis and spine. The rate at which the cancer spreads and the pattern of that spread will vary considerably from patient to patient.
Localized cancers – those limited to the prostate – are usually treated by surgical
removal or by radiation therapy.
Surgery may entail an open operation, done through an incision made in the lower
abdomen (radical retropubic prostatectomy - RRP), or through an incision made in
the perineum, between the rectum and the scrotum (radical perineal prostatectomy -
RPP). "Radical" refers to the fact that not only the prostate but also some attached and
surrounding tissues – the seminal vesicles, portions of the vasa deferentia, and some
connective tissue and blood vessels surrounding the prostate are also removed to
assure thorough elimination of the cancer. When indicated, the pelvic lymph nodes are
also sampled to assess for microscopic spread of cancer.
In recent years, a technique of prostate surgery using a surgical robot has been
developed, in which the surgery is done laparoscopically through very small abdominal
and pelvic incisions. This is known as "robot assisted laparoscopic prostatectomy"
[RALP] or the "DaVinci Robotic Prostatectomy" [DVP], so named because the robot
system is named for Leonardo DaVinci. There is growing evidence to suggest that
patients lose less blood, and may recover more quickly from surgery done using the
robot than with open procedures.
All surgical procedures may adversely affect a patient's ability to control his urination postoperatively. These difficulties are usually temporary, and continence is regained in weeks or months. Rarely significant incontinence may be permanent and may require additional treatment or surgery to correct. Additionally, surgery may injure or damage the small nerves that control erections, and may render a patient unable to achieve an erection postoperatively. Again, when necessary, there are treatments for this which assist a post-surgical patient with erection problems to function sexually. Surgical removal of the prostate renders the patient infertile.
Radiation therapy may entail external beam radiation [EBRT] in which ionizing
radiation is directed at the prostate from a radiation source outside of the body or
brachytherapy, sometimes also referred to as radioactive seed implant therapy or
interstitial therapy.
In an EBRT treatment, the patient lies on a table and radiation, focused on the prostate,
is beamed at the gland for several minutes. Treatments are repeated daily for 5 days a
week, with rest on the weekend days, and a full course of EBRT is usually 8 to 8-1/2
weeks, or 40 to 45 treatments. Side effects of treatment may include burning with
urination, diarrhea, rectal inflammation or tenderness, or generalized fatigue. There is evidence that suggests radiation therapy may be more effective when given along with hormonal therapy during treatment this may consist of a relatively short course of six months or, for some cases as long as 2 ½ years following completion of EBRT. Your urologist may suggest this if he feels it is appropriate in your case.
In brachytherapy, tiny metal capsules or "seeds," each about the size of a 1/16-inch
piece of pencil lead, are implanted into the prostate to radiate the tumor from within.
This procedure is done in the operating room, usually as outpatient surgery. The patient
is anesthetized, and the surgeon, using an ultrasound probe to guide a succession of
hollow needles into the prostate, places between 80 and 150 "seeds" evenly throughout
the gland. The radiation within the "seeds" then treats the tumor over the succeeding 4
to 6 months. Side effects are similar to those experienced with EBRT.
The advantage is the convenience of a one-day treatment session, and the possibility of delivering higher doses to the prostate
Cryotherapy: Another treatment sometimes used in localized prostate cancer is
cryotherapy of the prostate, which destroys the cancer by freezing. In this treatment,
the patient is anesthetized in the operating room and small probes are passed into the
gland, which permit it to be frozen in a controlled manner. Although a relatively new
treatment, results show this to be a promising option for treatment in selected patients.
Because cryotherapy almost always damages the nerves and renders the patient unable
to have erections, it is a less popular option for men in whom sexual function is an
important issue.
Advanced cancers and metastatic cancers are managed with androgen deprivation
therapy[ADT] or "hormonal therapy". In some advanced cases, chemotherapy may
also be used.
In patients who have minimal disease on biopsy, who have concomitant serious medical
problems, who are of advanced age, or who have less than 10-year life expectancy,
often no initial active treatment is most appropriate. Patients with an indolent tumor
and no suggestion of tumor progression may best be served by withholding treatment
until some evidence of progression is documented. Should cancer progression be
identified on physical exam or imaging or changes in the PSA level, therapy can be
immediately instituted.
Hormonal Therapy or Androgen Deprivation Therapy (ADT)
TESTOSTERONE and the PROSTATE
Because it is a part of the male reproductive system, the prostate gland is closely
controlled by the male sex hormone testosterone, which is mostly manufactured in the
testes. Testosterone stimulates prostate cells to produce secretions that constitute
about 85% of the fluid that a man ejaculates during intercourse. When testosterone is
not present, prostate cells, as well as other parts of the male reproductive system, are
rendered inactive.
Since prostate cancer is comprised of abnormal cells that are derived from once normal prostate cells, the vast majority of these cancer cells are also stimulated by testosterone. In the late 1930s, it was discovered that prostate cancer could be controlled by stopping the body from producing testosterone, thereby shutting down the tumor. The urologist who made this observation, Dr. Charles Huggins, was awarded a Nobel Prize.
CONTROLLING TESTOSTERONE
The earliest prostate cancer patients were treated by surgically removing the testes, an
operation called an orchiectomy. In recent years, medications have been developed
that "shut down" testosterone manufactured in the testes. These drugs are known as
LHRH(luteinizing hormone releasing hormone) agonists. LHRH is produced by the
pituitary gland and when it is released into the bloodstream it stimulates the testes to
produce testosterone and other androgens. Paradoxically, the agonist character of the
drug serves to exhaust the pituitary such that it can no longer produce LHR H. and
therefore androgen production comes to a relative halt
There are several LHRH. drugs which are used:the most common are Eligard
(leuprolide), Leupron (leuprolide), Zoladex (goseralin); other less commonly used
include histerelin and tripterelin These are administered by injection and can be dosed to
provide timed-release coverage for 1, 3, 4 or 6 months. Vantas (histrelin) and Viadur
(leuprolide acetate) can be administered as an implant which releases medication for a
full year.
Casodex (bicalutamide) and Eulexin (flutamide) are oral anti-androgen drugs which
block testosterone from stimulating the prostate cell at the level of the cell. Eulexin is
now used infrequently, but Casodex is sometimes used in conjunction with one of the
LHRH agonist drugs. Older drugs, such as cyproterone and TACE are now rarely
encountered.
In December of 2008, degarelex , a new addition to prostate cancer treatment, was approved by the FDA. This drug is a LHRh antagonist. Therefore, rather than operating by initial overstimulation and subsequent depletion, it directly inhibits the pituitary's production of LHRH and thereby halts the production of androgens. Currently it is available only in a one-month injection.
The effectiveness of treatment is usually monitored by physical examination, as well as with PSA levels, serum testosterone levels, and sometimes alkaline phosphatase determinations.
SIDE EFFECTS OF HORMONAL THERAPY
While LHRH agonists and antagonists and anti-androgen therapies are quite effective in
controlling most prostate cancers, both types of drugs exhibit side-effects. Low
testosterone results in a reduction of energy level in many men, and most men notice a
significant decrease in sex drive accompanied by impaired sexual function. Hot flashes,
similar to those experienced by women at menopause, are reported by many men.
With the prolonged use of LHRH agonists often required, there may be loss of muscle
strength and bulk, changes in hair pattern or quality, an impaired ability to focus or
concentrate, weight gain, fluid retention, breast changes, and loss of calcium from the
bones (osteopenia/osteoporosis). This loss of bone density may predispose men to
fractures, so often supplemental calcium and vitamin D therapy is recommended. This
will be addressed elsewhere.
TIMING OF HORMONAL THERAPY
Because hormonal therapy does cause side effects, the most appropriate time to initiate
therapy is not always clear, and also may vary depending upon the clinical situation.
Certainly clear evidence of progressive cancer would warrant starting therapy. Often if
bone metastases are present, patients may receive a short course of Casodex or DES.
This is because the injectable LHRH agonists will initially stimulate testosterone, and
therefore possibly the tumor, for a short period of time. This is avoided with Casodex or
DES suppression. Once the LHRH agonist therapy has begun, Casodex may be
discontinued, but in other instances it will be combined with the LHRH agonists (CAB) for
a longer duration, unless an extended period off medication occurs.
Many clinicians will not treat patients with hormonal therapy if the only evidence of recurrent or residual disease is an elevated PSA. Most often, patients will be followed with interval examinations and PSA determinations until some identifiable evidence of tumor progression is confirmed, at which time therapy is begun.However, there are certain criteria i.e. initial tumor grade, rapidity of PSA rise (PSA doubling time) that will prompt earlier androgen deprivation
Intermittent Androgen Therapy (IAT): In selected patients, hormonal therapy may be initiated and continued until PSA testing indicates that PSA has leveled off at a very low level. At this point, hormonal therapy is discontinued, and the PSA and physical exam are tracked, usually every 3 to 6 months, until some predetermined level of PSA – this may be the level of PSA at the time treatment was initially started. The interval off treatment (referred to as a drug holiday) may range from several months to several years. Once the PSA level is exceeded, hormonal therapy is reinstituted and again followed
until it falls to an acceptably low level, at which time therapy is again withheld and the cycle is repeated. Such intermittent therapy allows the patient time off hormonal medication and may improve his bone metabolism, energy levels, and sexual function.
Hormonal therapy on an intermittent schedule (known as IAT – Intermittent Antiandrogen Therapy) is sometimes used to diminish the negative effects of treatment, provide periods for the patient to be off the drugs, and diminish the risks of long-term consistent treatment.
HORMONE RESISTANCE
While initially the vast majority of cells in a given patient's cancer are sensitive to
hormonal treatment, some cells are not. These are known as "hormonally resistant"
tumor cells, and with time, they will become the dominant component of the tumor. As
this happens, the effectiveness of hormonal treatment is diminished, and there may be
an associated rise in PSA as well as other evidence of progression of the cancer. The
interval to progression is usually several years, and may be as long as 10 years or more
in some cases. When cancer progresses despite hormonal therapy, other forms of
tumor treatment, such as conventional chemotherapy, are likely to be recommended.
Using alternative anti-androgen medications, radiation therapy, and steroids may also be
considered. There are currently a number of agents that are being tested in clinical trials
which may be able to lowered testosterone more completely and reliably than the current
agents thereby hopefully increasing the duration of tumor response
BONE METABOLISM, CALCIUM SUPPLEMENTATION AND VITAMIN D THERAPY
Hormonal therapy taken for the treatment of prostate cancer is known to cause changes
in bone structure and loss of calcium – a condition known as osteopenia or osteoporosis.
With long-term treatment, the bone loss may predispose the patient to fractures. Such
bone loss can be diminished by increasing the intake of Vitamin D and calcium. In
addition, regular exercise and weight conditioning and cessation of smoking will
decrease bone loss.
We advise that patients receiving hormonal therapy for prostate cancer receive 500 to 1000 milligrams of calcium supplement (calcium carbonate, calcium malate, or calcium gluconate, calcium citrate) as well as 600 to 1200 units of Vitamin D each day. Such supplements are available over the counter.
In order to monitor adequate delivery of vitamin D supplementation, blood levels of vitamin D may be requested in order to adjust the vitamin D dose appropriately. In addition, to monitor the extent of osteopenia or osteoporosis, and the response to therapy, bone mineral density studies may be recommended
CALCIUM SUPPLEMENTATION AND VITAMIN D THERAPY
Hormonal therapy taken for the treatment of prostate cancer is known to cause changes in bone structure and loss of calcium – a condition known as osteopenia which may lead to a more severe condition of significant bone loss called osteoporosis. Hormonal therapies in men create a situation somewhat akin to that in post menopausal women. With long-term hormonal treatment, bone loss may predispose the patient to fractures, particularly in the hips and spine. Such bone loss can be diminished by increasing the intake of Vitamin D and calcium. In addition, regular exercise, weight conditioning, and cessation of smoking will help to decrease bone loss.
We advise that patients receiving hormonal therapy for prostate cancer receive 500 to 1000 milligrams of calcium supplement (calcium carbonate, calcium malate, or calcium gluconate) as well as 600 to 1200 units of Vitamin D each day (vitamin D3 , also called cholicalciferol). Vitamin D is necessary for the intestine to absorb dietary calcium. Both calcium and vitamin D supplements are available over the counter. One 8-oz glass of milk provides about a tenth of the daily requirement of calcium. TUMS is another inexpensive source of calcium supplementation.
In order to monitor adequate delivery of vitamin D supplementation, blood levels of vitamin D may be requested in order to adjust the vitamin D dose. In addition, to monitor the extent of osteopenia or osteoporosis, and the response to therapy, bone mineral density studies may be recommended
Patients with a history of kidney stones should discuss calcium and vitamin D supplements with their urologist prior to beginning therapy.
In addition to calcium and vitamin D, a drug called alendronate sodium (Fosamax) may also be prescribed. This drug facilitates an increase in bone mass and reduces the incidence of fractures. It is available as the plain medication and as "Fosamax plus D," which includes vitamin D supplementation. The drug is administered weekly and should be taken in the morning with 6-8 oz of water, before any food is taken. Patients should remain upright for at least 30 minutes following administration.
Rarely patients will experience bone, joint, or muscle pain with Fosamax therapy, and osteonecrosis of the jaw has also been reported, usually associated with a dental extraction or infection.
An intravenous medication, zoledronic acid or Zometa, also works to supplement bone resorption of calcium, and may be suggested in certain cases of advanced cancer.
A monoclonal antibody, denusamab, and a selective estrogen receptor modifier, toremifine have both been tested in phase 3 trials and each has shown to be effective in reducing osteoporosis and fractures secondary to this process. Both agents are currently being evaluated by the FDA for approval
Source: http://surf-1.org/downloads/ProstateCancer.pdf
Volume: 2, Issue: 1 April 2015 Twin Deficit Hypothesis: A Case of Pakistan Farrah Yasmin The Women University, Multan Pakistan Abstract: The prime motive of this study is to scrutinize the twin deficit for annual time series data over the period 1990-2010 for Pakistan. Twin deficit hypothesis expressed that an expansion in budget deficit will ground for rise in current account deficit. To diagnose affiliation amongst couple of variables, applied Unit root test (ADF-test), Johansen cointegration technique, Impulse response function and Granger causality test. The Granger causality demonstrate that the causality direction travel from current account deficit to budget deficit. When current account deficit occurs it leads to budget deficit. So the finding proves that there is a positive connection among both variables. Investigations are most reliable for Pakistan economy. Finally, this study confirms the rapport amid current account deficit and budget deficit. Keywords: Budget deficit, Current account deficit, Pakistan
2012 Drug Plan rePort b e n e f i t s plan costs. In particular, Brilinta and Eliquis join new agents such as Pradax and Xarelto to provide a wide range of new innovations in the oral blood clot treatment market—at a cost premium to existing therapies. Byetta and Trajenta are examples of the significant research and development focused on treating diabetes.