Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Physiopoint.cc
Physical Therapy Treatment Effectiveness for
Osteoarthritis of the Knee: A Randomized
Comparison of Supervised Clinical Exercise and
Manual Therapy Procedures Versus a Home
Program
Gail D Deyle, Stephen C Allison, Robert L Matekel,
Michael G Ryder, John M Stang, David D Gohdes,
Jeremy P Hutton, Nancy E Henderson and Matthew B
Garber
PHYS THER. 2005; 85:1301-1317.
The online version of this article, along with updated information and services, can befound online at: http://ptjournal.apta.org/content/85/12/1301
Collections
This article, along with others on similar topics, appearsin the following collection(s):
e-Letters
"Submit a response" in the right-hand menu under "Responses" in the online version of this article.
E-mail alerts
Physical Therapy Treatment
Effectiveness for Osteoarthritis of the
Knee: A Randomized Comparison of
Supervised Clinical Exercise and
Manual Therapy Procedures Versus a
Home Exercise Program
Background and Purpose. Manual therapy and exercise have not pre-viously been compared with a home exercise program for patients with osteo-arthritis (OA) of the knee. The purpose of this study was to compare outcomesbetween a home-based physical therapy program and a clinically based physicaltherapy program. Subjects. One hundred thirty-four subjects with OA of the kneewere randomly assigned to a clinic treatment group (n⫽66; 61% female, 39%male; mean age [⫾SD]⫽64⫾10 years) or a home exercise group (n⫽68, 71%female, 29% male; mean age [⫾SD]⫽62⫾9 years). Methods. Subjects in theclinic treatment group received supervised exercise, individualized manualtherapy, and a home exercise program over a 4-week period. Subjects in thehome exercise group received the same home exercise program initially, re-inforced at a clinic visit 2 weeks later. Measured outcomes were the distancewalked in 6 minutes and the Western Ontario and McMaster UniversitiesOsteoarthritis Index (WOMAC). Results. Both groups showed clinically andstatistically significant improvements in 6-minute walk distances and WOMACscores at 4 weeks; improvements were still evident in both groups at 8 weeks. By4 weeks, WOMAC scores had improved by 52% in the clinic treatment group andby 26% in the home exercise group. Average 6-minute walk distances had
improved about 10% in both groups. At 1 year, both groups were substantiallyand about equally improved over baseline measurements. Subjects in the clinictreatment group were less likely to be taking medications for their arthritis andwere more satisfied with the overall outcome of their rehabilitative treatmentcompared with subjects in the home exercise group. Discussion and Conclusion.
Although both groups improved by 1 month, subjects in the clinic treatmentgroup achieved about twice as much improvement in WOMAC scores thansubjects who performed similar unsupervised exercises at home. Equivalentmaintenance of improvements at 1 year was presumably due to both groupscontinuing the identical home exercise program. The results indicate that ahome exercise program for patients with OA of the knee provides importantbenefit. Adding a small number of additional clinical visits for the application ofmanual therapy and supervised exercise adds greater symptomatic relief. [DeyleGD, Allison SC, Matekel RL, et al. Physical therapy treatment effectiveness forosteoarthritis of the knee: a randomized comparison of supervised clinicalexercise and manual therapy procedures versus a home exercise program.
PhysTher. 2005;85:1301–1317.]
Key Words: Exercise, Knee Osteoarthritis, Manual therapy, Physical therapy.
Gail D Deyle, Stephen C Allison, Robert L Matekel, Michael G Ryder, John M Stang, David D Gohdes,
Jeremy P Hutton, Nancy E Henderson, Matthew B Garber
Physical Therapy . Volume 85 . Number 12 .
Osteoarthritis(OA)isthemostcommonjoint strength (loss of force-generating capacity of
disease causing disability, affecting more
muscle),18–20 coronary heart disease,21 and depression.22
than 7 million people in the United States.1More disability and clinical symptoms result
Several interventions are available for OA. Well-designed
from OA of the knee than from any other joint.2,3
studies show that capsaicin cream, laser treatment, and
Osteoarthritis of the knee is reported to be a major
transcutaneous electrical nerve stimulation (TENS)
health problem worldwide.4,5
decrease the pain associated with OA.23–25 Arthroscopicsurgery has not been shown to have a role in the
The etiology of knee OA is not entirely clear, but its
management of knee OA. Knee capsule injections of
incidence increases with age and in women.6,7 Obesity is
saline, tidal irrigation, and placebo surgery have all been
a risk factor for the development and progression of
shown to be equal to arthroscopy.26–28 Acetaminophen is
knee OA and the need for total joint replacement.6,8,9
widely prescribed and considered to be low risk, but
The association between physical activity and knee OA
recent studies29,30 have shown minimal benefit for reduc-
remains controversial.10–12 Underlying biomechanical
ing the pain associated with OA. Nonsteroidal anti-
factors also may predispose people to OA.13,14 Increased
inflammatory drugs (NSAIDs) are frequently prescribed,
incidence of OA has been reported in both the intact
but they have significant side effects.31–33 Topical diclofe-
and amputated limbs in people with amputations.15
nac has been found to decrease the pain of knee OA,
Early degenerative changes predict progression of the
with presumably fewer gastrointestinal side effects.34
disease.16,17 The disability and pain associated with knee
Cyclooxygenase-2-selective inhibitors (coxibs) were ini-
OA correlate with a loss of quadriceps femoris muscle
tially thought to be the safer alternative to nonselective
GD Deyle, PT, DPT, is Assistant Professor and Graduate Program Director, Rocky Mountain University of Health Professions, Provo, Utah; AssistantProfessor, Baylor University, Waco, Tex; and Senior Faculty, US Army–Baylor University Post Professional Doctoral Program in OrthopaedicManual Physical Therapy, Brooke Army Medical Center, San Antonio, Tex. Address all correspondence to Dr Deyle at 3 Sherborne Wood, SanAntonio, TX 78218-1771 (USA) (
[email protected]).
SC Allison, PT, PhD, is Professor, Rocky Mountain University of Health Professions, and Adjunct Professor of Physical Therapy Education, ElonUniversity, Elon, NC.
RL Matekel, PT, DScPT, is Lieutenant Colonel, Army Medical Specialist Corps, and Chief, Physical Therapy, Madigan Army Medical Center, FtLewis, Wash.
MG Ryder, PT, DScPT, is Major, Army Medical Specialist Corps, and Officer-in-Charge, Primary Care Physical Therapy, Brooke Army MedicalCenter, Ft Sam Houston, Tex.
JM Stang, PT, DScPT, is Lieutenant Colonel, Army Medical Specialist Corps, and Chief, Physical Therapy, Ireland Army Community Hospital, FtKnox, Ky.
DD Gohdes, PT, MPT, is Lieutenant Colonel, Army Medical Specialist Corps, and Assistant Chief, Physical Therapy, Tripler Army Medical Center,Tripler AMC, Hawaii.
JP Hutton, PT, MPT, is Lieutenant Colonel, Army Medical Specialist Corps, and Chief, Physical Therapy, Eisenhower Army Medical Center, FtGordon, Ga.
NE Henderson, PT, PhD, is Physical Therapist, Steilacoom, Wash.
MB Garber, PT, DScPT, is Major, Army Medical Specialist Corps, and Assistant Chief, Physical Therapy, Brooke Army Medical Center.
All authors provided concept/idea/research design, writing, and consultation (including review of manuscript before submission). Dr Deyle, DrAllison, Dr Matekel, Dr Ryder, Dr Stang, LTC Gohdes, Dr Hutton, and Dr Garber provided data collection. Dr Allison and Dr Henderson provideddata analysis. Dr Deyle, Dr Matekel, Dr Ryder, Dr Stang, LTC Gohdes, and Dr Hutton provided subjects. Dr Deyle provided facilities/equipment.
Dr Deyle, Dr Matekel, Dr Ryder, Dr Stang, LTC Gohdes, Dr Hutton, and Dr Garber provided clerical support.
The study was approved by the institutional review board of Brooke Army Medical Center, Fort Sam Houston, Tex.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the viewsof the Department of the Army or the Department of Defense.
This article was received September 30, 2004, and was accepted May 18, 2005.
1302 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
NSAIDs, but recent concerns have included gastrointes-
1. Knee pain and crepitus with active motion and morning
tinal, cardiovascular, renal, and hepatic side effects.35–40
stiffness ⱕ30 min and age ⱖ38 y
Glucosamine supplements are widely used, with some
2. Knee pain and crepitus with active motion and morning
stiffness ⬎30 min and bony enlargement
controversy with regard to their efficacy and long-term
3. Knee pain and no crepitus and bony enlargement
benefits for people with knee OA.41,42 Ice massageimproves range of motion (ROM), function, and knee
Figure 1.
Clinical criteria for the diagnosis of osteoarthritis of the knee.59 Sub-
strength, and cold packs decrease swelling in patients
jects with examination findings consistent with any of the 3 cate-
with knee OA.43,44 Hot packs or ultrasound are not
gories were considered to have knee osteoarthritis. Sensitivity⫽89%,
thought to be of therapeutic value.43,45
A growing body of evidence shows that exercise improvesknee joint function and decreases symptoms.46–57 Fur-
reported by Deyle et al48 are reproducible in a multi-
thermore, the findings of a recent study 48 suggest that
center trial with different subjects and treating thera-
physical therapy intervention including exercise may
pists. Our hypothesis was that physical therapy consisting
reduce the need for knee arthroplasty and intra-articular
of manual therapy and supervised exercise conducted in
injections. However, the most effective types and combi-
the clinic would be more effective than an exercise
nations of exercise and dosage are unclear. The setting
program performed at home for improving function
in which the exercises should be performed and the
and decreasing pain and stiffness.
level of professional attention required to initiate andmaintain the exercise program also should be the sub-
ject of further investigation.
Benefits have been reported with manual therapy tech-
One hundred thirty-four subjects with OA of the knee
niques used in combination with joint mobility and
were randomly assigned to a clinic treatment group
strengthening exercises.48,58 Falconer et al58 found
(n⫽66; 26 male, 40 female; mean age [⫾SD]⫽64⫾10
improvements in motion (11%), pain (33%), and gait
years) or a home exercise group (n⫽68; 20 male, 48
speed (11%) after 12 treatments of stretching, strength-
female; mean age [⫾SD] 62⫾9). One of the investiga-
ening, and mobility exercises combined with manual
tors used a computer random-number generator to
therapy procedures performed in a physical therapy
determine group allocation. The randomization list
clinic over 4 to 6 weeks. A comparison group that
determined the sequence of enrollment folders con-
received the same exercise and manual therapy interven-
cealed in a locked cabinet. After a potential subject
tions plus therapeutic doses of ultrasound demonstrated
agreed to participate, a research assistant opened the
no additional improvement.
cabinet to retrieve the next folder in sequence and thenmade allocation as indicated in the folder. All folders
In a controlled, randomized, single-blinded study, Deyle
were identical in external appearance; each folder con-
et al48 demonstrated that manual therapy techniques
tained a sheet of paper indicating group assignment that
and exercises applied by physical therapists for 8 clinical
could be accessed only by opening the folder. Subjects
visits produced a 52% improvement in self-reports of
were either referred by their physicians for physical
function, stiffness, and pain as measured by the Western
therapy or were self-referred.
Ontario and McMaster Universities Osteoarthritis Index(WOMAC) scale and a 12% improvement in 6-minute
Subjects who were admitted to the study were diagnosed
walk test scores. A placebo control group that received
with OA of the knee based on clinical criteria developed
equal clinical attention showed no improvement in
by Altman59 (Fig. 1), which he found to be 89% sensitive
WOMAC scores or 6-minute walk test scores.
and 88% specific. Additional inclusion criteria wereeligibility for military health care and no physical impair-
The need for cost effectiveness throughout the health
ment unrelated to the knee that would prevent the
care system emphasizes the importance of knowing
subject from safely participating in any aspect of the
whether patients require numerous visits to a physical
study. All subjects were required to have sufficient
therapist or whether they might receive a similar benefit
English language skills to complete the pain, stiffness,
from a well-designed home program. The primary pur-
and functional assessment questionnaire. Subjects were
pose of this study was to determine the effectiveness of a
excluded if they could not attend the required number
clinically applied treatment that included exercise and
of visits, had received a cortisone injection to the knee
manual therapy compared with an exercise program
joint within the previous 30 days, or had a surgical
performed at home for OA of the knee. A secondary
procedure on either lower extremity within the past 6
purpose was to determine whether the high levels of
months. Subjects were instructed to continue taking any
improvement in pain, stiffness, and functional ability
medication that had been initiated 30 days or more priorto enrollment in the study.
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1303
tion. For example, if the examination revealed that a
Informed consent was obtained after screening for inclu-
subject was limited in the ability to perform a full squat
sion and exclusion criteria. Subjects in both groups
or if the subject experienced pain with that activity,
provided descriptive data for age, sex, height, weight,
squatting would be reassessed after manual techniques
duration of symptoms, presence of symptoms in one or
intended to improve knee flexion. If the symptoms
both knees, previous surgery, medications, exercise fre-
associated with squatting were subsequently decreased
quency, and perceived exertion levels. Sunrise and
or the range of the squatting motion improved, that
weight-bearing anteroposterior and lateral knee radio-
technique was considered to have a positive effect and
graphs were obtained and examined by radiologists for a
would be continued at subsequent sessions. General
radiographic severity rating for OA of the knee,60 with
improvements from session to session in these quick
scores ranging from 0 (least severe) to 4 (most severe).
functional tests also were considered a positive overallresponse to the intervention in either treatment group.
All enrollment, data collection, and clinic treatment
A neurological examination that included muscle
sessions were conducted in the physical therapy clinics at
strength testing, muscle stretch reflex testing, and sen-
3 military hospitals: Brooke Army Medical Center in
sory testing was performed if there were complaints of
Texas, Madigan Army Medical Center in Washington,
weakness, radiating pain, or altered sensation in the
and Martin Army Community Hospital in Georgia.
lower extremities.
Radiographs were obtained in the radiology departmentof each military hospital. Physical therapist assistants
Subjects in the clinic treatment group attended 8 treat-
trained to be research assistants obtained the blinded
ment sessions in the physical therapy clinic. Manual
pretreatment measurements. Training of the research
therapy programs were individualized based on the
assistants included review of the WOMAC procedure
results of the examination. The manual therapy tech-
manual61 and practice administering the WOMAC.
niques, consisting of passive physiological and accessory
Training for the 6-minute walk test included using a
movements, muscle stretching, and soft tissue mobiliza-
stopwatch, marking laps on a preprinted 6-minute walk
tion, were applied by the treating physical therapist
test form, and measuring the distance walked in an
primarily to the knee and surrounding structures (Tabs.
incrementally marked long hallway under simulated test
1 and 2). Detailed descriptions of the manual therapy
techniques and intervention philosophy utilized in thisstudy are available in manual therapy textbooks.68,69
The primary outcome measure in this study was the
Similar manual treatments also were administered to
WOMAC.61 Secondary outcome measures were a timed
the lumbar spine, hip, and ankle if these areas exhibited
6-minute walk test, the frequency of knee injections or
a limitation in either active or passive movement and
knee surgery, medication use, and overall satisfaction
were judged to contribute to the overall lower-extremity
with the rehabilitative treatment. The WOMAC consists
of 24 questions, each corresponding to a visual analogscale, designed to measure patients' perceptions of pain,
In addition to receiving manual therapy treatments,
stiffness, and dysfunction. High WOMAC scores reflect
subjects in the clinic treatment group performed a
high self-perceptions (greater severity) across the 3
standardized knee exercise program at each treatment
domains measured by the scale. The WOMAC, which was
session. This program consisted of active ROM exercises,
specifically designed to evaluate patients with OA of the
muscle strengthening, muscle stretching, and riding a
hip or knee, has been shown to be a highly responsive,
stationary bicycle. A physical therapist or physical ther-
multidimensional outcome measure that yields moder-
apy technician supervised these exercises. The number
ately reliable and valid scores.62–64 The timed 6-minute
of strengthening exercise bouts and stationary bicycle
walk test measures the distance a person walks in 6
riding time were increased or decreased by the treating
minutes and has been demonstrated to yield reliable
physical therapist based on subject response. The exer-
measurements of functional exercise capacity; it is fre-
cise program was based on the best available evidence
quently used in OA-related trials.46,65–67
for the most efficient methods of producing the desiredeffects of increasing strength, flexibility, and ROM at the
initiation of this study.71–76 Subjects were examined for
received a standardized clinical examination. The exam-
adverse signs and symptoms such as increased pain, joint
ination included active and passive ROM assessments,
effusion, and increased skin temperature over knee
manual muscle testing, and palpation of the lumbar
joints at each clinic visit. All elements of hands-on
spine, hip, knee, and ankle. Simple functional tests
treatment and exercise were progressed only if the
(eg, squatting, step-ups) that limited or reproduced
symptoms and signs of OA were decreasing. If any
symptoms were used to obtain daily baseline measure-
soreness lasted more than a few hours after the interven-
ments to help assess the effect of the manual interven-
tion, the regimen was decreased accordingly for that
1304 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
Table 1.
Comparison of Interventions by Intervention Group
Strengthening exercise
Strengthening exercise
Stretching exercise
Stretching exercise
No manual therapy
Level of exercise supervision
1 exercise instruction session
Level of exercise supervision
2 exercise instruction
7 supervised exercise
a Home stationary bicycle riding in both exercise groups was allowed if it was part of the participant's exercise program before the study. Participants in the homeexercise group were not specifically instructed to ride a stationary bicycle, nor was it recorded on the exercise adherence log. ROM⫽range of motion.
subject. Subjects in the clinic treatment group per-
for another blinded assessment of WOMAC scores and
formed the same home exercise program as the home
6-minute walk test measurements. Subjects in both
exercise group each day that they were not treated in the
groups were instructed to refrain from their home
physical therapy clinic.
exercises and their daily walk on the day of the secondassessment. Assessments were performed at the same
The home exercise group received detailed verbal and
time of day as the pretest to help control for daily cycles
hands-on instruction in a home-based program of the
in pain and stiffness.
same exercises as the clinical treatment group. Similar tothe subjects who received clinical treatment, subjects in
During the second 4-week period, subjects in both
the home exercise group were instructed that pain
groups continued their daily home exercise program. At
should be avoided in all exercises except in the case that
8 weeks, both groups of subjects returned for a third
pain or stiffness decreased with each repetition. Each
assessment of WOMAC scores and 6-minute walk test
subject received a detailed supporting handout contain-
measurements. At 1 year, subjects were contacted and
ing instructions and photographs of the exercises. A
queried about knee injections, knee surgeries, medica-
home program adherence log was maintained by each
tion use, and overall satisfaction with outcomes of their
subject. Subjects in the home exercise group were
rehabilitative treatment. WOMAC scores and 6-minute
allowed to ride a stationary bicycle if they stated that
walk test measurements were obtained at 1 year for those
riding a bicycle was currently part of their exercise
subjects who were able to return to the clinic for
routine or if they could not walk for safety reasons.
Riding of the stationary bicycle was not recorded on theexercise adherence log for the home exercise group.
The sample size was determined a priori by a statistical
The details of the manual therapy and exercise interven-
power calculation based on anticipated group differ-
tions for both groups are shown in Tables 1 through 5.
ences in WOMAC scores at 4 weeks. For this calculation,the standard deviation was estimated to be 400 mm, the
A follow-up examination was performed for the home
minimal clinically important difference between groups
exercise group 2 weeks after the initial visit. Examiners
was defined as 200 mm (about 20% of anticipated
checked for adverse signs and symptoms such as
average baseline score), and statistical power was 80%
increased pain, joint effusion, and increased skin tem-
with approximately 64 subjects per group.
perature over knee joints. The exercise log was reviewed,the subjects were again supervised performing the
Data Analysis
home-based program, and observed performance defi-
Data from the initial measurement session were analyzed
ciencies were corrected. Exercises were progressed only
to determine whether significant group differences
if the symptoms and signs of OA were stable or decreasing.
existed using independent
t, Mann-Whitney
U, andchi-square tests for ratio, ordinal, and categorical vari-
Neither group of subjects was aware of the intervention
ables, respectively. All data analyses were performed with
that the other group was receiving. Subjects in both
SPSS for Windows (version 10.1).* Descriptive data
groups were instructed to take a daily walk at a comfort-able pace and gradually progressed distance. After 4weeks, subjects from both groups returned to the clinic
* SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1305
Table 2.
Common Knee Impairments Addressed by Manual Therapy
Loss of knee extension
Manual mobilization through range of motion (ROM)
Mobilization grades III and IV to III⫹⫹ and IV⫹⫹
and knee extension at end range
2–6 bouts of 30 s per manual technique
Clinical observation: this manual intervention may
Knee extension with valgus or abduction
provide near-immediate decrease of symptoms
Knee extension with varus or adduction
and may be approached with relatively morevigor than knee flexion
Loss of knee flexion
Manual mobilization through ROM and knee flexion
Mobilization grades of III- and IV- to III⫹ and IV⫹
2–6 bouts of 30 s per manual technique
Clinical observation: pain with end-range knee
Knee flexion plus medial (internal) rotation
flexion may be due to degenerative meniscaltears; end-range techniques should be utilizedwith caution
Loss of patellar glides
Manual mobilization of the patella in 5°–10° of knee
Mobilization grades of IV to IV⫹⫹
2–6 bouts of 30 s per manual technique
Clinical observation: some patients may be
intolerant of even slight compressive forces over
the patella; therapist hand placement is
Manual stretches at end length of the muscle
Sustained manual stretches of 12–30 s duration
Quadriceps femoris
repeated 1–3 times per muscle
Clinical observation: the lumbar spine should be
manually stabilized and protected during all
extremity stretches, particularly hip flexor
stretches; many of these patients also will have
Tensor fasciae latae and the iliotibial band
arthritic changes in the spine, and symptomscan be increased without care in positioning
Soft tissue tightness
Soft tissue mobilization
Circular fingertip and palm pressure mobilization
Suprapatellar and peripatellar regions
at the depth of the capsule or retinaculum for
Medial and lateral joint capsule
1–3 bouts of 30 s per area
Clinical observation: the soft tissue work in the
popliteal fossa seems to work best whenperformed slowly with occasional sustainedpositions of 10–12 s, this technique works wellwhen combined with the manual mobilizationsinto knee extension
analysis and tests for the assumptions of normality and
possible predictors among baseline variables were
homogeneity of variance were followed by a 2 ⫻ 3
included in a forced-entry analysis: treatment group
assignment, age, height, weight, sex, duration of symp-
(MANOVA) with an alpha level of .05 for the subset of
toms, self-rating of physical activity level, days per week
120 study participants who provided all data at baseline,
of aerobic activity, bilaterality of symptoms, use of med-
4 weeks, and 8 weeks. The independent variables for the
ications, severity of radiographic findings, and initial
MANOVA were group (with 2 levels) and time (with 3
scores for the WOMAC and the 6-minute walk test. The
levels). The 2 dependent variables were WOMAC scores
WOMAC scores and 6-minute walk test measurements
and 6-minute walk test distances. Subsequent 2 ⫻ 3
obtained at the 4-week follow-up were entered as depen-
univariate analyses of variance (ANOVAs) for each
dent variables for the regression analyses. An intention-
dependent variable were performed with a Bonferroni-
to-treat analysis was conducted by carrying the last
corrected alpha level of .025.
Post hoc analyses of signif-
obtained measurements forward for those subjects who
icant group ⫻ time interaction effects were performed
did not complete all aspects of the study.
with the Tukey multiple-comparison procedure.
In order to investigate the potential for confounding
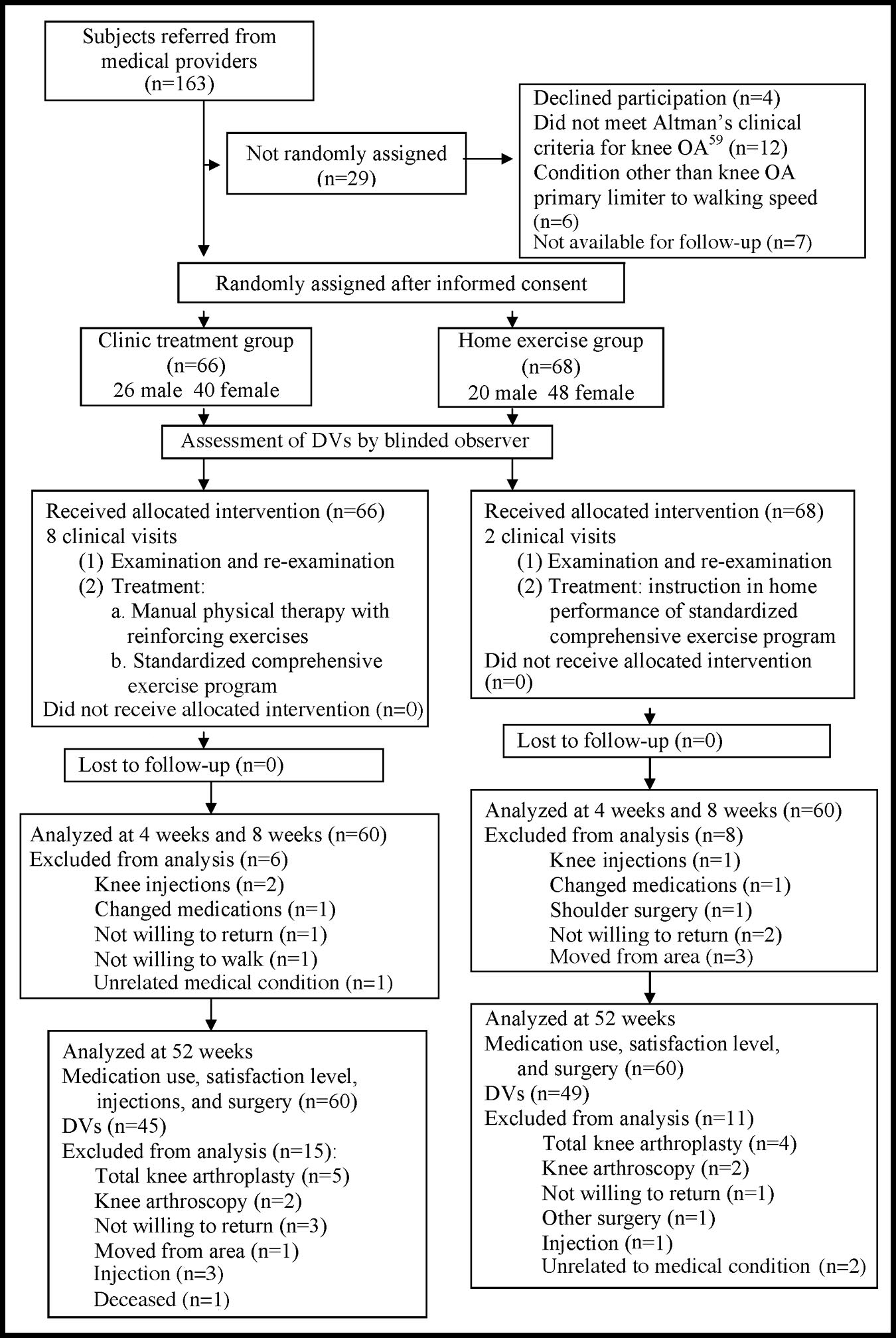
Of the 134 subjects initially enrolled in the study (Fig. 2),
variables, a separate multiple regression model was cre-
60 subjects in the clinic treatment group and 60 subjects
ated for each outcome variable. In each model, 13
in the home exercise group completed all treatment and
1306 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
Table 3.
Patient Exercise Program: Strengthening Exercises
Statis quad sets in knee extension
Hold each contraction for 6 s with a
Patient is positioned fully supine or supine supported
10-s rest between repetitions
on elbows with the knee in full extension
Patient contracts the quadriceps femoris muscle and
pushes the knee down while maintaining the footin full dorsiflexion
Standing terminal knee extension
Perform 3⫻ per week
Hold each contraction for 3 s
Patient stands with a resistive band or a cuff from a
weighted pulley mechanism behind a slightly
Increase resistance as tolerated
Patient contracts the gluteal and quadriceps femoris
muscles to fully straighten the hip and knee
Patient performs one of the following activities 3⫻
ordered from least to most
Patient should progress to the most challenging
activity that he or she can successfully completewith minimal or no pain
Seated leg presses
Patient is seated holding a resistive band in both
Hold each contraction 3 s with knee as
straight as possible
Patient places his or her foot against the band, then
Slowly return to starting position and
straightens the knee by pushing the foot down
repeat for a 30 s bout.
and forward by contracting the gluteal and
Progress to bands of increasing
quadriceps femoris muscles
resistance and additional bouts
Partial squats weight-lessened
Patient stands with arm support as needed
Hold each contraction 3 s with hips and
with arm support as needed
Patient performs a partial squat, keeping the knees
knees as straight as possible
centered over the feet
Return to standing by contracting the quadriceps
Progress to full body weight without
femoris and gluteal muscles
support and additional bouts
Patient stands in front of a low step
Slowly repeat for 30 s
Patient places foot of involved leg on step and
Progress to increased height of the step
brings body over foot to stand on the step
and additional bouts
Use as little push-off assistance from the contralateral
Alternate legs if both knees are involved
Step down with the contralateral foot
testing at 0, 4, and 8 weeks. In the clinic treatment
group, 1 subject withdrew due to unrelated medical
completers in each group are given in Table 6. Table 7
reasons, 2 subjects were disqualified after receiving knee
contains mean scores with 95% confidence intervals
injections, 1 subject changed medications during the
(CIs) for the dependent variables measured at 0, 4, and
study, and 1 subject failed to return for unknown
8 weeks for the completer subjects. Medication use by
reasons. The 6-minute walk test measurement for the
subjects in each group of completers is presented in
8-week testing session was unavailable for 1 additional
subject in the clinic treatment group. In the homeexercise group, 3 subjects moved from the area, 1 subject
For subjects who completed all aspects of the study, the
changed medications during the study, 1 subject with-
randomization procedure resulted in reasonably homog-
drew to receive shoulder surgery, 1 subject was disqual-
enous groups at the outset of the study (Tab. 6). The 14
ified after receiving cortisone injections to the knee, and
subjects who failed to return for the 4-week or 8-week
2 subjects failed to return for unknown reasons. No
measurement session appeared to differ from the sub-
subjects were discontinued due to lack of adherence to
jects who completed the study, as measured by several
the treatment regimen. All 120 subjects who completed
variables. However, the statistical tests revealed signifi-
the study attended all clinical appointments and
cant differences only for the initial WOMAC scores,
reported for testing at 0, 4, and 8 weeks. The other 14
which were about 22% worse (
P⫽.03) for the subjects
subjects reflect an overall dropout rate of 11%: 9% in the
who did not complete the study, and for radiographic
clinic treatment group and 12% in the home exercise
severity scores (
P⫽.002) (median⫽2 for the subjects who
completed the study and median⫽3 for the subjects who
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1307
Table 4.
Patient Exercise Program: Stretching Exercises
Standing calf stretch
Hold for 30 s and repeat 3⫻
Patient stands with the heel of the foot on the
ground behind the patient; the toes pointstraight ahead
The patient leans forward until a moderate pull
is perceived in the calf musculature
The patient may use his or her arms for support
against a wall or furniture as needed
Supine hamstring muscle stretch
Hold for 30 s and repeat 3⫻
Patient is positioned supine with the contralateral
Clinical observation: if radicular symptoms are
lower extremity maintained as straight as
produced, decrease or eliminate the ankle
dorsiflexion or the intensity of the stretch
The ipsilateral hip is flexed to 90°The knee is straightened and the proximal lower
leg supported with the hands until a moderatepull is perceived in the posterior thigh and calf
The ipsilateral ankle should be dorsiflexed
Prone quadriceps femoris
Hold for 30 s and repeat 3⫻
Patient is positioned prone with both hips and
Clinical observation: hamstring muscle
cramping may occur if the patient attempts
A strap is placed around the ipsilateral ankle
to actively bend the knee; to reduce this
and brought posteriorly and superiorly over
possibility, always use the strap to passively
the ipsilateral shoulder
The patient grasps the strap in the ipsilateral
Maintain a gentle stretch and comfortable
hand and bends the knee by straightening his
position for the lumbar spine
or her elbow and pulling on the strap
Hard stretching will frequently create lumbar
The knee is progressively flexed until a gentle
symptoms in this population
stretch is perceived in the anterior thigh
Table 5.
Patient Exercise Program: Range of Motion Exercises
Knee in mid-flexion to full-extension
Performed once daily
Two 30-s bouts with 3-s hold at end
Patient is positioned supine or supine supported
Clinical observation: these exercises work
Knee is brought to 45° of flexion with the
best if performed on a smooth surface
ipsilateral foot sliding on the surface that the
such as a hardwood or linoleum floor
patient is lying on
or if a sliding board is used
The knee is then fully extended with a strong
quadriceps femoris muscle contractionagainst any limitation to full knee extension
Knee in mid-flexion to full-flexion
Performed once daily
Two 30-s bouts with 3-s hold at end
Patient is positioned supine or supine supported
Clinical observation: pain with end-range
Knee is brought to full flexion with assistance of
knee flexion may be due to
the upper extremities or a strap
degenerative meniscal tears
A gentle challenge to end-range flexion is
Over-pressure to end range should be
applied with caution
Stationery bicycle
Performed once daily
5 min, increase time as tolerated
Knees should be at nearly full extension at
Clinical observation: some patients are
bottom of pedal stroke
intolerant of the stationary bicycle, andclinical judgment is required tocontinue the activity
1308 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
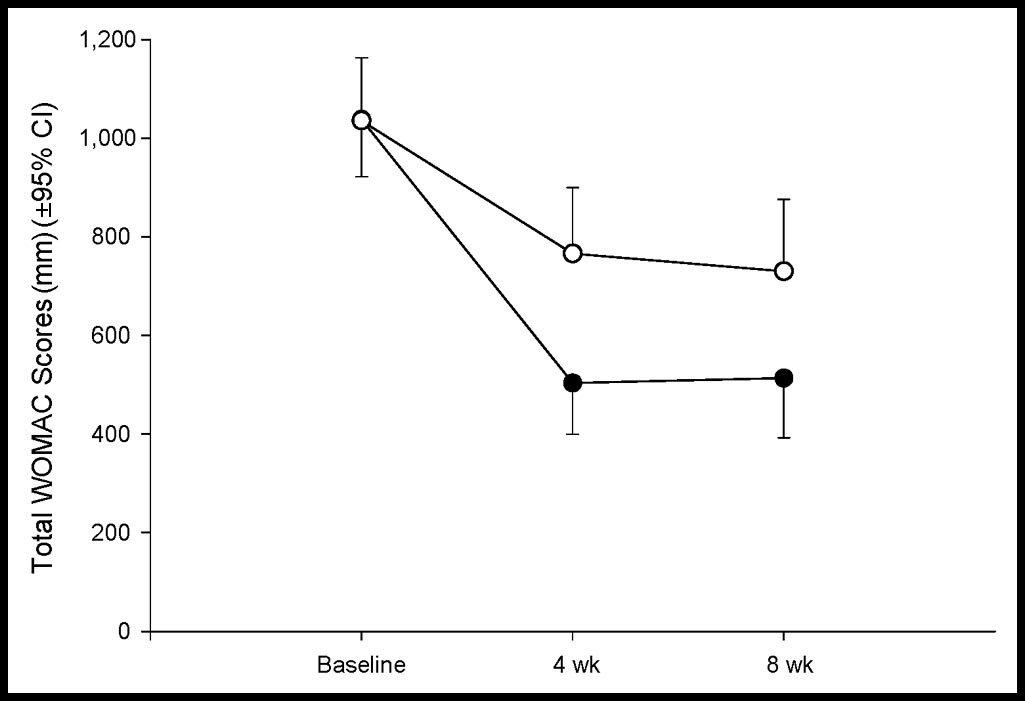
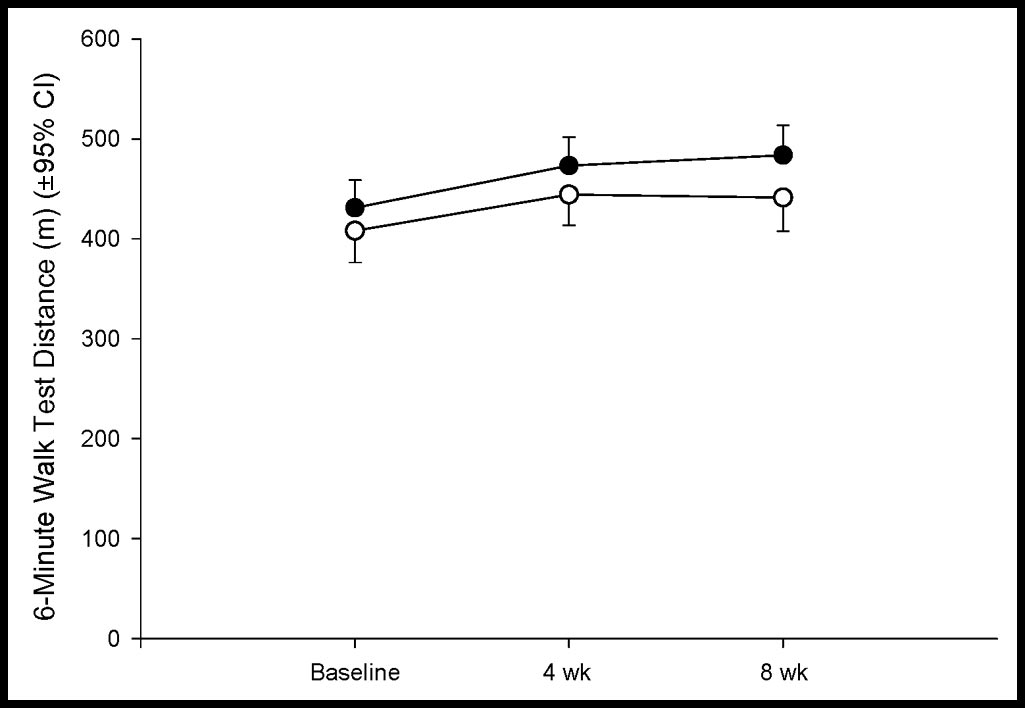
The assumptions of normality andhomogeneity of variance were met forboth WOMAC scores and 6-minutewalk test measurements. For the 120subjects who provided data at 0, 4, and8 weeks, the MANOVA revealed agroup
⫻ time interaction effect
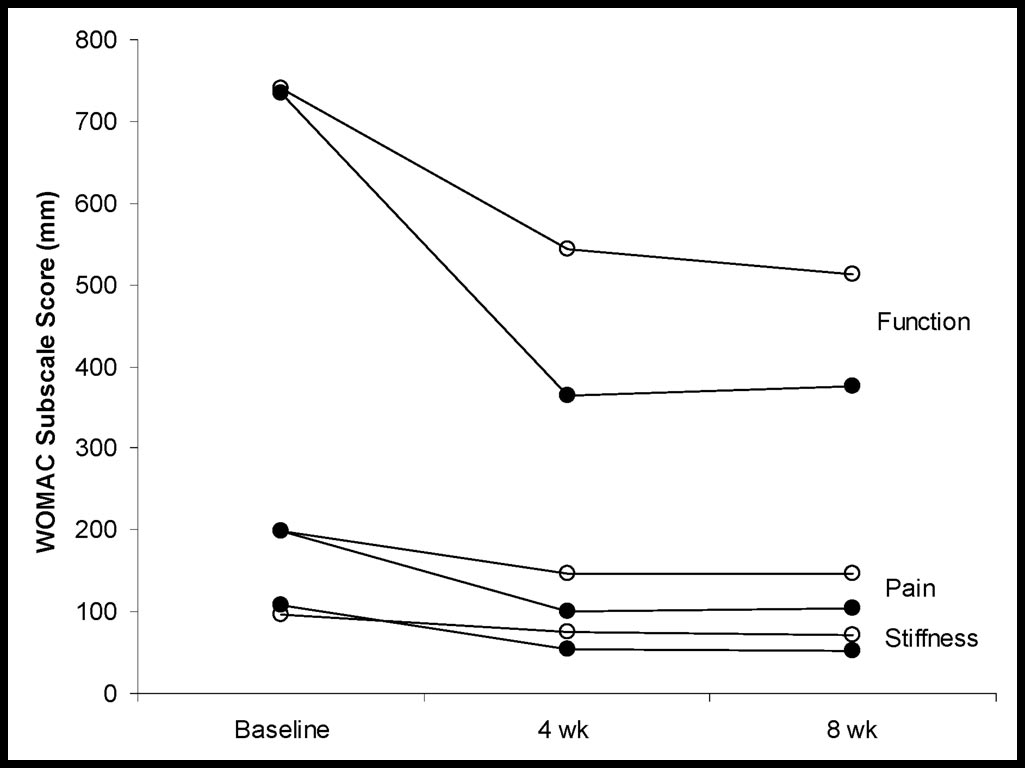
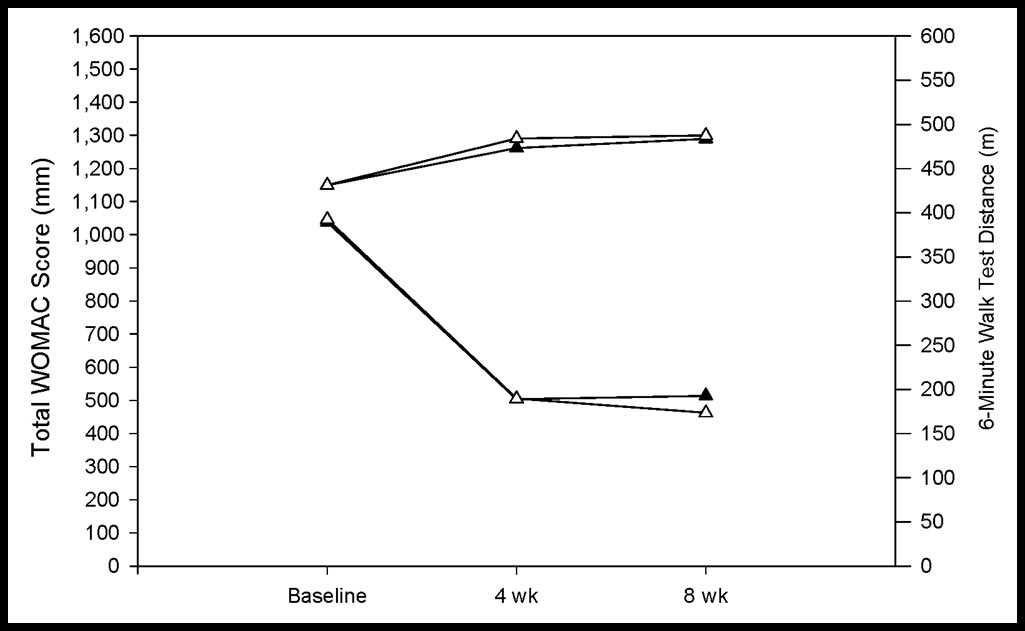
(P⫽.001), suggesting that changes inaverage scores over time depended ontreatment group assignment. Subse-quent univariate ANOVAs also demon-strated a group ⫻ time interactioneffect for the WOMAC scores (P⫽.001)but not for the 6-minute walk test dis-tances (P⫽.199). The nonparallel plotsof the average WOMAC scores (Fig. 3)reflect the differential effect over timeof the clinic treatment and home exer-cise treatment on this outcome vari-able. In contrast, the relatively parallelplots of the average distances walkedreflect the lack of an interaction effectfor this variable (Fig. 4). For both theWOMAC scores and the 6-minute walktest measurements, there was a statisti-cally significant (P⬍.001) main effectfor time, reflecting an improvementfrom average initial values to thoserecorded at 4 weeks.
Post hoc pair-wise comparisons of meanscores revealed that the 2 groups ofsubjects who completed the study werehomogenous at the time of initial test-ing for WOMAC scores and 6-minutewalk test distances (P ⬎.05). Comparedwith initial 6-minute walk test distances,both groups improved, on average,about 40 m (about 10%) at 4 weeks(95% CI⫽30 – 48 m) and did notchange substantially between 4 and 8
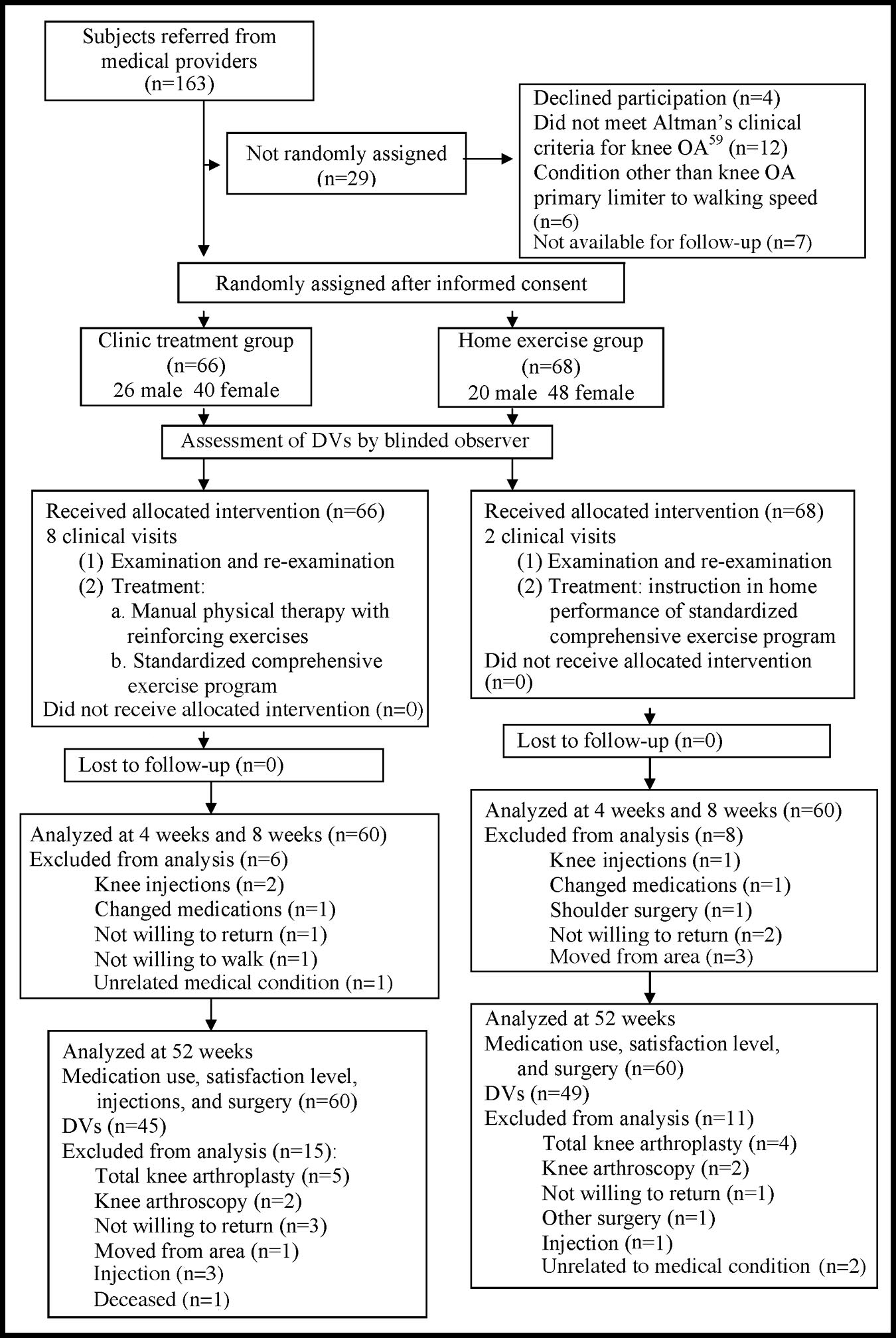
Figure 2.
weeks (Tab. 7). Both groups also
Flow chart describing the progress of subjects through the trial. OA⫽osteoarthritis,
improved in average WOMAC scores
DV⫽subjects for whom the dependent variables were measured.
between baseline and 4 weeks, but theclinic treatment group improved abouttwice as much as the home exercise
did not complete the study) (Tab. 6). Durations of
group. The average 4-week WOMAC score improved
symptoms appeared to be longer but were not signifi-
52% (535 mm, 95% CI⫽426 – 644 mm) for the clinic
cantly different for the subjects who did not complete
treatment group and 26% (270 mm, 95% CI⫽193–346
the study (P⫽.43). This apparent difference in mean
mm) for the home exercise group. Neither group
duration was attributable primarily to one subject who
reported symptoms lasting 564 months. Upon removing
between 4 weeks and 8 weeks. Average WOMAC scores
the outlier, mean duration of symptoms for the subjects
for the clinic treatment group were 263 mm better (95%
who completed the study was 74 months versus 71
CI⫽93– 432 mm) than those for the home exercise
months for the subjects who did not complete the study
group at 4 weeks and 217 mm better (95% CI⫽34 –
400 mm) at 8 weeks (Tab. 7). The multiple regression
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1309
Table 6.
Baseline Characteristics: Descriptive Statistics and Group Comparisons
Duration of symptoms (mo)
WOMACa score
Distance walked, 6 min (m)
Bilateral symptoms
Days/week of vigorous
physical activity
Severity of radiographic
a WOMAC⫽Western Ontario and McMaster Universities Osteoarthritis Index.
Table 7.
Group Comparisons: Means and 95% Confidence Intervals (CIs) for the Western Ontario and McMaster Universities Osteoarthritis Index
(WOMAC) and the 6-Minute Walk Test at 0, 4, and 8 Weeksa
Clinic treatment group
Home exercise group
6-minute walk test (m)
Clinic treatment group
Home exercise group
a Includes only subjects who completed testing at 8 weeks. Clinic treatment group: n⫽60; home exercise group: n⫽60.
analysis revealed no meaningful influence of the poten-
that did not differ substantially from the results of the
tial confounding variables on the outcome scores.
analysis for the 120 subjects who completed the study. In
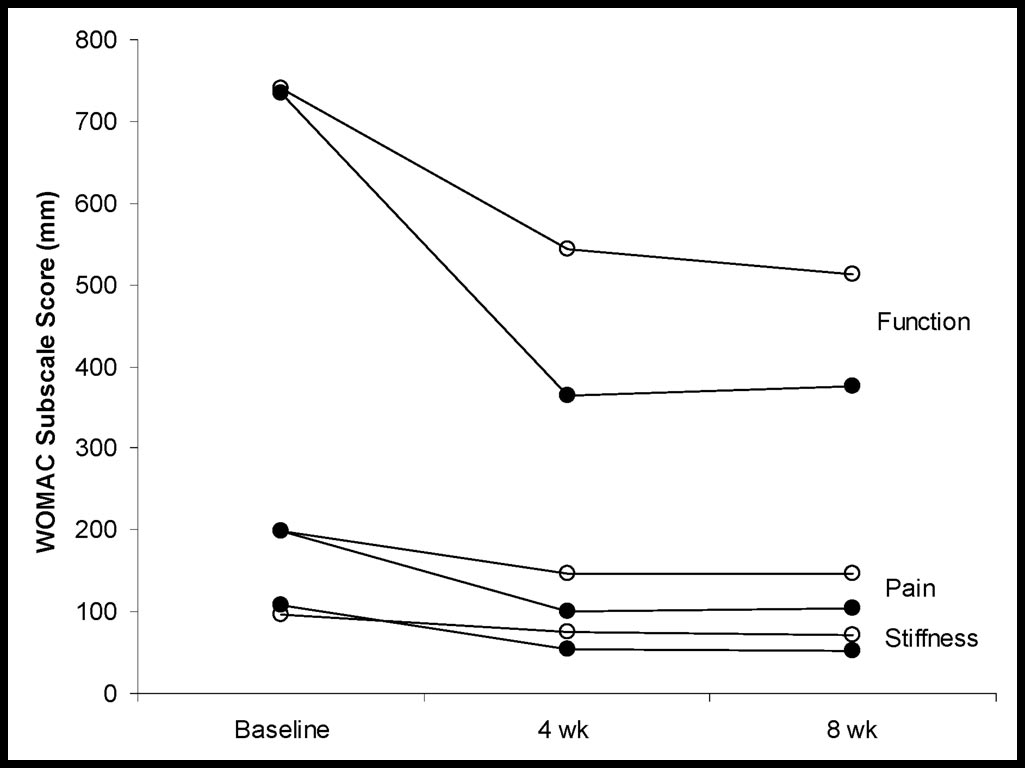
WOMAC subscale analyses also were conducted for
the intention-to-treat analysis, both groups improved
those subjects who adhered to protocols through week 8.
about 9% in average 6-minute walk test distances at 4
Results were consistent and similar to the results of the
weeks; average 4-week WOMAC scores were improved
total WOMAC score analysis, with significant group ⫻
45% for the clinic treatment group and 24% for the
time interaction effects (Pⱕ.004) for each of the pain,
home exercise group.
stiffness, and function subscales (Fig. 5).
All 120 subjects who completed testing through 8 weeks
The results of the intention-to-treat analysis conducted
were contacted 1 year after enrollment into the study. By
for all 134 subjects enrolled in the study yielded results
1 year, 5 subjects (8%) in the clinic treatment group and
1310 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
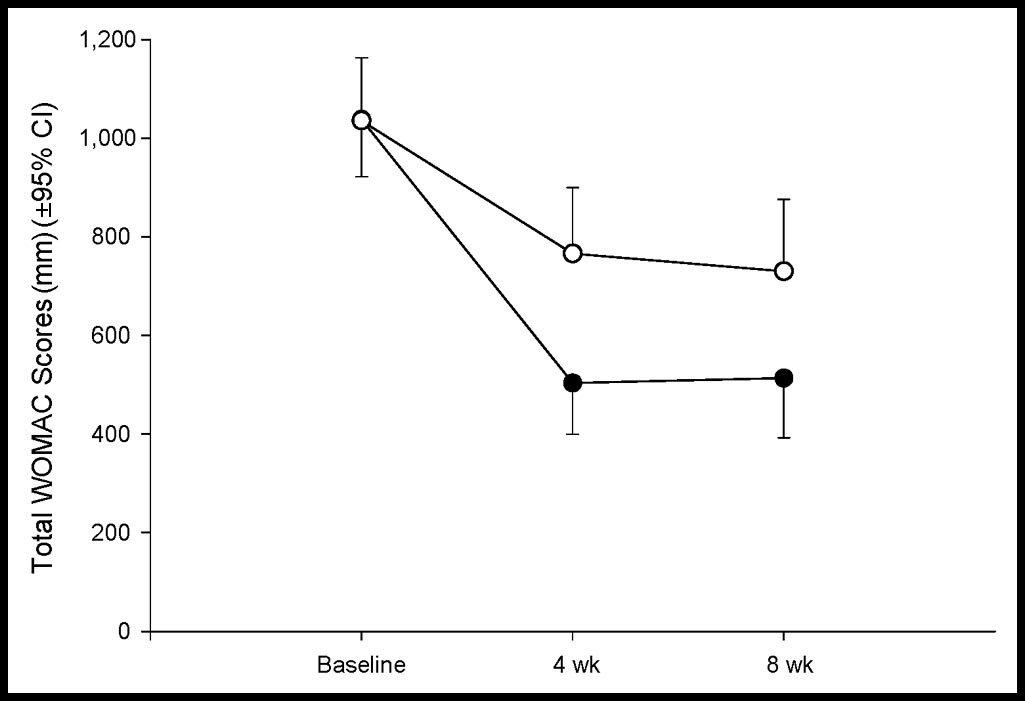
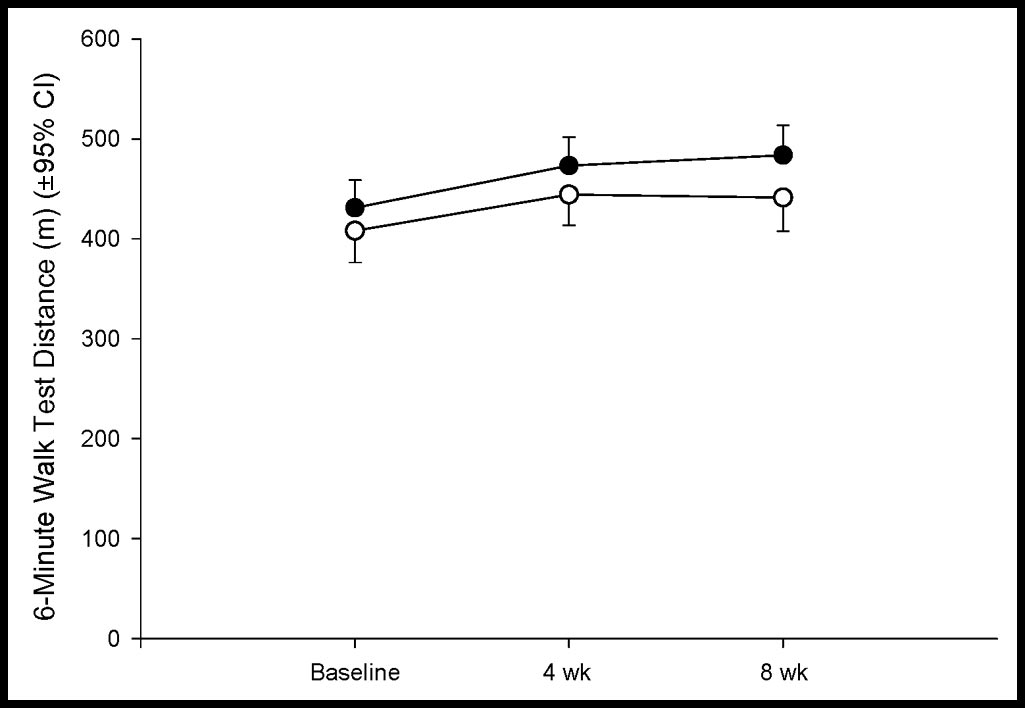
Table 8.
Medication Usea in the Clinic Treatment Group and Home Exercise Group
Clinic Treatment Group Completers (nⴝ60)
Home Exercise Group Completers (nⴝ60)
No. of Subjects
% of Subjects
No. of Subjects
% of Subjects
Codeine phosphate
a Use of medication was documented but not controlled in this study. Invasive cointerventions such as cortisone injections or surgical procedures were grounds forremoval from the study.
b G.D. Searle & Co, Div of Pfizer, 235 E 42nd St, New York, NY 10017-5755.
c Mylan Pharmaceuticals Inc, 781 Chestnut Ridge Rd, PO Box 4310, Morgantown, WV 26504-4310.
d GlaxoSmithKline, Five Moore Dr, Research Triangle Park, NC 27709.
e LKT Laboratories Inc, 2233 University Ave W, St Paul, MN 55114-1629.
Figure 3.
Figure 4.
Average Western Ontario and McMaster Universities Osteoarthritis
Average distance walked in 6 minutes at initial visit, 4 weeks, and 8
Index (WOMAC) scores at initial visit, 4 weeks, and 8 weeks. Lower
weeks. Closed circles represent the clinic treatment group; open circles
scores indicate perceived improvement in pain, stiffness, and function.
represent the home exercise group. On average, subjects in both groups
Closed circles represent the clinic treatment group; open circles repre-
improved over the 8-week period (P⬍.001). CI⫽confidence interval.
sent the home exercise group. Among subjects who completed the study,those in the clinic treatment group had a greater average improvementin WOMAC scores over the 8-week period (P⬍.001) than those in the
testing at 1 year to determine whether the improvements
home exercise group. CI⫽confidence interval.
in 6-minute walk test distances and the WOMAC scoresat 8 weeks were still evident 1 year after the intervention.
4 subjects (7%) in the home exercise group had received
At the 1-year follow-up, average improvements in
a total knee arthroplasty. Two subjects (3%) in the
WOMAC scores and 6-minute walk test distances were
clinical treatment group and 2 subjects (3%) in the
still significantly improved. Compared with baseline
home exercise group had knee arthroscopy. Two sub-
scores, average 1-year WOMAC scores were 32% better
jects (3%) in the clinic treatment group and 1 subject
in the clinic treatment group and 28% better in the
(2%) in the home exercise group received steroid
home program group. However, after 11 months of
identical home program regimens, both groups wereequally improved over baseline WOMAC measurements.
Among the 120 subjects who completed testing through8 weeks, 45 subjects in the clinic treatment group and 49
Subjects contacted at 1 year responded to a 5-point
subjects in the home exercise group were available for
Likert-type question asking how satisfied they were with
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1311
home exercise group. Improvements and between-group differences seen at 4 weeks were still measurableat 8 weeks. The benefits of a 4-week intervention werenot lost for either group during an intervening monthwith no treatment other than continued home exercises.
Subjects in the clinic treatment group appeared to bemore satisfied with the overall outcome of their rehabil-itative treatment than subjects in the home exercisegroup. These results suggest that clinical interventionconsisting of manual therapy and supervised exercisewas more effective than a home exercise program forincreasing function and decreasing pain and stiffnessover an 8-week period.
The difference between groups is likely attributable tothe additional effects of the clinical intervention consist-
Figure 5.
ing of manual therapy, stationary bicycling, and supervi-
Average Western Ontario and McMaster Universities Osteoarthritis
sion of the exercises that the other group was perform-
Index (WOMAC) subscale scores at initial visit, 4 weeks, and 8 weeks.
ing unsupervised at home. Deyle et al48 demonstrated no
Lower scores indicate perceived improvements in pain, stiffness, andfunction. Closed circles represent the clinic treatment group; open circles
significant change in WOMAC scores or 6-minute walk
represent the home exercise group. The upper pair of plots represent
test measurements in patients with knee OA who
mean scores for the function subscale, the middle pair of plots represent
received a clinically applied placebo treatment.
mean scores for the pain subscale, and the lower pair of plots representmean scores for the stiffness subscale. Among subjects who completed
The clinical intervention was more expensive than the
the study, those in the clinic treatment group had greater averageimprovements, with all 3 WOMAC subscale scores over the 8-week
home intervention. Per-visit reimbursement for the clin-
period (Pⱕ.004) than those in the home exercise group.
ical physical therapy interventions would range from $83for Medicare to $129 for commercial reimbursementrate. Therefore, the cost for 2 to 3 visits to initiate and
the overall result of their rehabilitative treatment. Poten-
maintain the home program is minimal. The difference
tial responses were: "not at all satisfied," "a little satis-
for 8 clinical visits in the clinic treatment group versus 2
fied," "a fair amount satisfied," "much satisfied," and
clinical visits in the home program group would range
"very much satisfied." Subjects in the clinic treatment
from $498 to $774. These additional costs are compara-
group indicated a greater level of satisfaction (P⫽.018)
ble to the costs of other interventions such as the cost of
than those in the home exercise group. Fifty-two percent
a series of viscosupplementation injections, and they are
of those in the clinic treatment group said they were
less than one tenth of the cost of a total knee replace-
"very much satisfied" with their outcomes compared with
ment.78 The question then becomes whether twice the
only 25% in the home exercise group. Sixteen percent of
level of improvement in the WOMAC score over a period
those in the home exercise group stated they were "a
from 8 weeks to less than 1 year merits the additional
little satisfied" or "not at all satisfied" compared with
only 5% in the clinic treatment group.
The results observed in the clinic treatment group in this
Subjects contacted at 1 year also were asked whether they
study are nearly identical to those previously reported in
were taking any medications for their OA. Sixty-eight
an earlier study for the same intervention.48 In both
percent of the subjects in the home exercise group were
studies, subjects in the clinic treatment groups improved
taking medications compared with 48% in the clinic
an average of about 50% in WOMAC scores and about
treatment group (P⫽.03).
10% in 6-minute walk test distances over the 4-weekperiod of active treatment (Fig. 6). The reproducibility
of these observed treatment effects is apparent from
Both treatment groups obtained successful outcomes, as
nearly identical improvements for the clinical treatment
measured by significant reductions in WOMAC scores
groups in these 2 studies that enrolled completely dis-
and improvement in 6-minute walk test distances over a
tinct sets of subjects and used distinct sets of treaters and
4-week period. The reductions in WOMAC scores in
both groups exceeded the 20% to 25% levels suggestedas minimally meaningful by Barr et al.77 The post-
The reproduction of these findings is important to the
treatment WOMAC scores in the group who received
management of patients with OA of the knee. The level
biweekly treatments in the physical therapy clinic were
of functional improvement with this clinical treatment
markedly better than the WOMAC scores seen in the
1312 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
in the clinical treatment group to the level of the homeexercise group is presumably due to withdrawing theclinical sessions consisting of manual therapy, stationarybicycling, and supervised exercise. Both groups contin-ued the common home exercise program and main-tained an equal level of improvement.
Typically, when manual therapy and reinforcing exer-cises are utilized in a clinical setting, periodic follow-upappointments help maintain the effects of the interven-tion. It will be important to determine the optimalfrequency of follow-up treatment sessions required tomaintain the higher level of improvement realized from
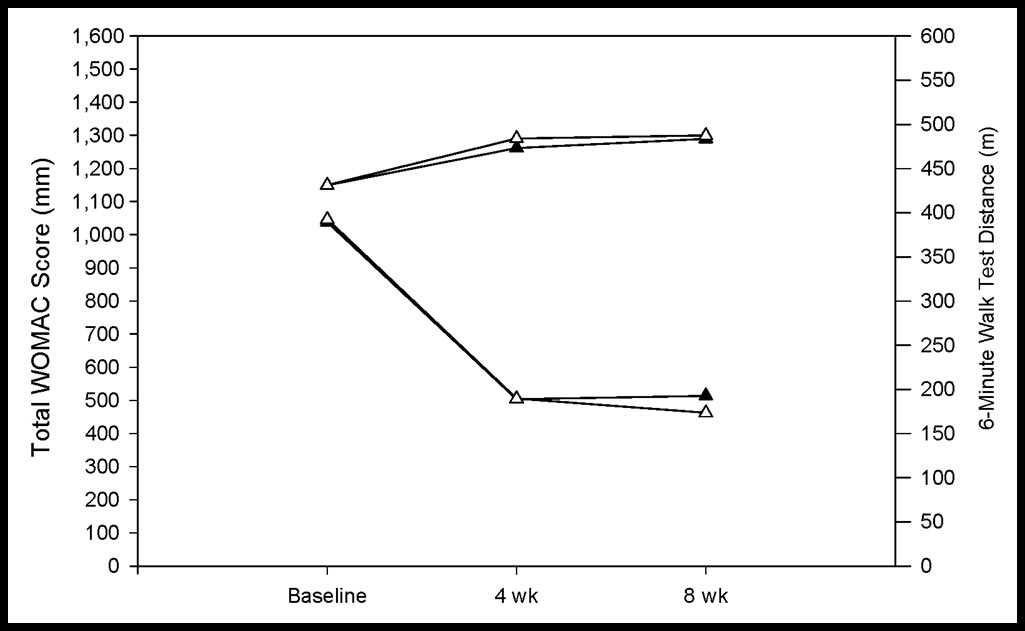
Figure 6.
clinical treatment in this study. The practice of establish-
Average distances walked and average Western Ontario and McMas-
ing periodic recheck appointments or allowing the
ter Universities Osteoarthritis Index (WOMAC) scores at initial visit, 4
patient to contact the physical therapist when relief from
weeks, and 8 weeks from 2 separate groups of subjects who received
manual treatment and reinforcing exercise diminishes
identical manual therapy plus supervised exercise treatments from 2studies with similar research designs. The upper set of plots represents
appears appropriate on the basis of the results of this
average 6-minute walk test distances scaled on the right axis; the lower
study. The 8 clinical visits also might be spread more
set of plots indicates average WOMAC scores, scaled on the left axis.
evenly over a longer period in order to sustain the effects
Closed triangles represent the subjects from the current study (n⫽60);
of manual therapy. Some subjects derived benefit after
open triangles represent subjects from the 2000 study by Deyle et al48
only 2 to 4 interventions; for these subjects, the remain-
(n⫽33). Both sets of plots combine to demonstrate the reproducibility ofthese results.
ing clinical sessions could have been distributed over alonger period of time. Some authors82,83 have advocatedthe use of periodic physical therapy treatment for
program of manual therapy and supervised exercise is
chronic conditions and have compared this strategy with
greater than has been reported for other conservative
the use of other therapeutic approaches, including use
treatments24,53,54 and has been compared with improve-
of medications for chronic conditions.
ments seen after total knee arthroplasty.79
The treatment effects associated with other common
The benefit from the comprehensive clinically instruct-
interventions for knee OA also are known to diminish
ed home exercise program in the current study is
over time and may be additionally associated with signif-
consistent with the highest levels of benefit from exer-
icant side effects. Viscosupplementation is a widely used
cise reported in the previously cited studies. This benefit
and recommended knee OA therapy.84 Individual stud-
accrued to patients in the current study with only 2 clinic
ies that have demonstrated benefit for hyaluronic acid
visits, whereas previously reported home regimens
also revealed a return to near-baseline levels after 3 to 6
required a range of 1 to 12 (mean of 4) clinical visits for
months.85–88 Intra-articular hyaluronate injections have
instruction and reinforcement to yield similar or lesser
been associated with calcium pyrophosphate dehydrate
benefits.46,47,49,51,55,56,80,81 The success of the home pro-
arthritis and inflammatory flares of other types.89,90
gram may be attributable to any or all of the features
Intra-articular steroids have been associated with
designed into the program: careful instruction, minimal
increased risk for septic arthritis.91 Single intra-articular
exercise performance time, an adherence log, a high-
injections of steroids for knee OA have been demon-
quality exercise folder, and a comprehensive set of
strated to be equivalent to placebo. Multiple injections
exercises addressing muscle tightness, limitations in
have produced pain relief indistinguishable from a pla-
joint movement, muscle weakness, and general fitness.
cebo at 4 to 6 weeks.86
Although the exercises of the subjects in the clinictreatment group were observed and corrected as neces-
It would be important to know whether the subjects who
sary, subjects in the home exercise group exercised
received the interventions in this study were better
without the supposed benefits of frequent supervision;
prepared for total joint replacement surgery or had
they received one-to-one supervision only initially and at
lower postoperative complication rates. In general, refer-
the 2-week follow-up visit.
ring physicians and other clinicians need to knowwhether short-term physical therapy interventions for
The WOMAC scores at the 1-year follow-up measure-
chronic conditions such as OA of the knee can influence
ment were still improved over baseline measurements,
eventual utilization of more invasive treatments such as
although group differences on this scale that were
injections and joint arthroplasties. More attention needs
evident at 4 weeks and 8 weeks were not observed at 1
to be placed on studying the effects of combinations of
year. The reduction of the treatment effect after 1 year
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1313
therapies such as glucosamine use, viscosupplementa-
tion group in this study and yet failed to demonstrate any
tion, and physical therapy. More work also is needed to
change over time.
further define the relative benefits of home programsand intensive clinical intervention in physical therapy.
Results of this study should be reasonably generalizableto patients with knee OA of either sex with similar ages
Both groups in the current study improved their walking
and OA severity levels. There is a common perception
distance to about the same extent, presumably because
that studies of patients in military health care facilities
of the identical instructions regarding a daily walking
may suffer from limited external validity because of
program. This finding is consistent with results from a
cultural differences and unique factors related to subject
previous study 48 in which placebo group patients
adherence to treatment regimens. We do not think it is
received no instructions for a walking program and did
likely that the high level of benefit demonstrated for
not improve their walking distances.
either treatment group was due to any factors related tomilitary service. Foremost, 63% of the subjects in this
The combination of manual therapy and exercise has
study were family members who had never served in the
been shown to reduce the need for total knee replace-
military. Only one subject was on active duty during the
ment and steroid injections, with a number needed to
study. The mean body mass index (BMI) for the former
treat of 7 when compared with placebo intervention.48,78
military subjects (BMI⫽30.6, 95% CI⫽29.0 –32.1) was
In the current study, there was not a difference in the
not significantly different from that of subjects who had
surgical rates between the 2 effective interventions. This
never served in the military (BMI⫽32.5, 95% CI⫽30.9 –
finding may be due, in part, to the fact that both groups
34.0); the subjects in both groups were equivalently
performed the same home exercise program and the
obese. The mean level of physical activity also was
additional benefit of the clinical intervention was
equivalent for those subjects who had served in the
allowed to regress over time. It would be interesting to
military and for those subjects who had not served in the
determine whether additional sessions would further
military. The average number of days per week of
reduce the need for total joint replacement and other
vigorous physical activity at the time of study enrollment
also was equivalent for those subjects with prior militaryservice (average days per week⫽2.13, 95% CI⫽1.45–
Alternatively, it may be possible for patients or their
2.80) versus those subjects without prior military service
spouses to administer simple manual therapy techniques
(average days per week⫽2.00, 95% CI⫽1.48 –2.52).
to perpetuate the effects of clinical intervention. How-
Finally, most of the subjects who had served in the
ever, patients with knee OA may be elderly and have
military had been retired for periods of time longer than
involvement in other joints, which may make it difficult
the duration of their military service.
for self-treatment or even treatment administered by aspouse. Future studies, we believe, should address
One rationale for the manual therapy approach to OA is
whether patients with OA of the knee might be catego-
that the reduced pain and stiffness associated with the
rized into specific subgroups with preferentially greater
manual therapy intervention allows patients to partici-
probabilities of responding to specific interventions.
pate more successfully in the exercise program andactivities of daily living. Knee OA symptoms may result
Two potential threats to internal validity in the current
from restricted mobility and adhesions due to recurrent
study warrant consideration. It is possible that both
inflammations of both intra-articular and periarticular
groups improved for reasons unrelated to our interven-
tissues. Movement restrictions due to changes within
tion. The clinical treatment group may have improved
these tissues also may alter the biomechanical forces on
more dramatically simply because of the increased inten-
articular surfaces to create additional symptoms. The
sity of the relationship with the physical therapists. We
manual therapy passive movement techniques were
consider this explanation unlikely for 2 reasons. First,
applied to increase excursion in both intra-articular and
both groups comprised patients with chronic OA; the
periarticular tissues when restricted mobility was judged
average duration of symptoms was more than 5 years. It
to be related to the reproduction of symptoms or
is unlikely in these groups that spontaneous improve-
ments of 35% to 50% would be observed over a 1-monthperiod. Second, the current study builds on the results of
an earlier study 48 with a placebo group. In that study, no
A clinical physical therapy program of manual therapy to
changes in the WOMAC scale or in 6-minute walk test
the lower quarter combined with supervised exercise
distances were observed in the placebo group from
applied by skilled physical therapists was compared with
initiation of treatment through the 1-year follow-up. The
a home exercise program for improving function and
placebo group in the earlier study had the same intensity
decreasing stiffness and pain in subjects with OA of the
of physical therapist interaction as the clinical interven-
knee. The comprehensive clinical treatment program
1314 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
resulted in large improvements, reproducing the results
15 Jevsevar DS, Riley PO, Hodge WA, Krebs DE. Knee kinematics and
previously reported for the same therapeutic regimen.
kinetics during locomotor activities of daily living in subjects with knee
After 1 month of treatment, the average improvement in
arthroplasty and in healthy control subjects. Phys Ther. 1993;73:229 –239; discussion 240 –242.
pain, stiffness, and function seen in the clinic treatmentgroup was twice the magnitude of the improvement
16 Wolfe F, Lane NE. The long-term outcome of osteoarthritis: rates
and predictors of joint space narrowing in symptomatic patients with
observed in the home exercise group.
knee osteoarthritis. J Rheumatol. 2002;29:139 –146.
One year after withdrawing the clinical intervention and
17 Englund M, Lohmander LS. Risk factors for symptomatic knee
osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis
further patient contact, this difference between groups
was no longer evident. Both groups remained substan-
18 Lewek MD, Rudolph KS, Snyder-Mackler L. Quadriceps femoris
tially improved over baseline measurements. Subjects in
muscle weakness and activation failure in patients with symptomatic
the clinic treatment group appeared less likely to be
knee osteoarthritis. J Orthop Res. 2004;22:110 –115.
taking medications for their arthritis and were more
19 Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee
satisfied with the overall outcome of their rehabilitative
osteoarthritis: its prevalence and relationship to physical function.
treatment at 1 year compared with subjects in the home
Arthritis Rheum. 2004;51:941–946.
exercise group.
20 Fitzgerald GK, Piva SR, Irrgang JJ, et al. Quadriceps activation
failure as a moderator of the relationship between quadriceps strength
and physical function in individuals with knee osteoarthritis. Arthritis
1 D'Ambrosia RD. Epidemiology of osteoarthritis. Orthopedics. 2005;28:
Rheum. 2004;51:40 – 48.
21 Philbin EF, Ries MD, Groff GD, et al. Osteoarthritis as a determi-
2 Felson DT, Zhang Y, Hannan MT, et al. The incidence and natural
nant of an adverse coronary heart disease risk profile. J Cardiovasc Risk.
history of knee osteoarthritis in the elderly: the Framingham Osteo-
1996;3:529 –533.
arthritis Study. Arthritis Rheum. 1995;38:1500 –1505.
22 Wolfe F. Determinants of WOMAC function, pain and stiffness
3 Felson DT, Naimark A, Anderson J, et al. The prevalence of knee
scores: evidence for the role of low back pain, symptom counts, fatigue
osteoarthritis in the elderly: the Framingham Osteoarthritis Study.
and depression in osteoarthritis, rheumatoid arthritis and fibro-
Arthritis Rheum. 1987;30:914 –918.
myalgia. Rheumatology (Oxford). 1999;38:355–361.
4 Corti MC, Rigon C. Epidemiology of osteoarthritis: prevalence, risk
23 Philadelphia Panel Evidence-Based Clinical Practice Guidelines on
factors, and functional impact. Aging Clin Exp Res. 2003;15:359 –363.
Selected Rehabilitation Interventions for Shoulder Pain. Phys Ther.
2001;81:1719 –1730.
5 De Filippis L, Gulli S, Caliri A, et al. Epidemiology and risk factors in
osteoarthritis: literature review data from "OASIS" study [in Italian].
24 Puett DW, Griffin MR. Published trials of nonmedicinal and non-
Reumatismo. 2004;56:169 –184.
invasive therapies for hip and knee osteoarthritis. Ann Intern Med.
1994;121:133–140.
6 Felson DT, Zhang Y, Hannan MT, et al. Risk factors for incident
radiographic knee osteoarthritis in the elderly: the Framingham Study.
25 Deal CL, Schnitzer TJ, Lipstein E, et al. Treatment of arthritis with
Arthritis Rheum. 1997;40:728 –733.
topical capsaicin: a double-blind trial. Clin Ther. 1991;13:383–395.
7 Lachance L, Sowers MF, Jamadar D, Hochberg M. The natural
26 Bradley JD, Heilman DK, Katz BP, et al. Tidal irrigation as treat-
history of emergent osteoarthritis of the knee in women. Osteoarthritis
ment for knee osteoarthritis: a sham-controlled, randomized, double-
Cartilage. 2002;10:849 – 854.
blinded evaluation. Arthritis Rheum. 2002;46:100 –108.
8 Messier SP, Loeser RF, Mitchell MN, et al. Exercise and weight loss in
27 Chang RW, Falconer J, Stulberg SD, et al. A randomized, controlled
obese older adults with knee osteoarthritis: a preliminary study. J Am
trial of arthroscopic surgery versus closed-needle joint lavage for
Geriatr Soc. 2000;48:1062–1072.
patients with osteoarthritis of the knee. Arthritis Rheum. 1993;36:289 –296.
9 Christensen R, Astrup A, Bliddal H. Weight loss: the treatment of
choice for knee osteoarthritis? a randomized trial. Osteoarthritis Carti-
28 Moseley JB, O'Malley K, Petersen NJ, et al. A controlled trial of
lage. 2005;13:20 –27.
arthroscopic surgery for osteoarthritis of the knee. N Engl J Med.
2002;347:81– 88.
10 Manninen P, Riihimaki H, Heliovaara M, Suomalainen O. Physical
exercise and risk of severe knee osteoarthritis requiring arthroplasty.
29 Towheed TE, Judd MJ, Hochberg MC, Wells G. Acetaminophen for
Rheumatology (Oxford). 2001;40:432– 437.
osteoarthritis. Cochrane Database Syst Rev. 2003:CD004257.
11 Sandmark H, Vingard E. Sports and risk for severe osteoarthrosis of
30 Mannoni A, Briganti MP, Di Bari M, et al. Epidemiological profile
the knee. Scand J Med Sci Sports. 1999;9:279 –284.
of symptomatic osteoarthritis in older adults: a population based studyin Dicomano, Italy. Ann Rheum Dis. 2003;62:576 –578.
12 Spector TD, Harris PA, Hart DJ, et al. Risk of osteoarthritis associ-
ated with long-term weight-bearing sports: a radiologic survey of the
31 Henry D, Lim LL, Garcia Rodriguez LA, et al. Variability in risk of
hips and knees in female ex-athletes and population controls. Arthritis
gastrointestinal complications with individual non-steroidal anti-in-
Rheum. 1996;39:988 –995.
flammatory drugs: results of a collaborative meta-analysis. BMJ. 1996;312:1563–1566.
13 Cooper C, Snow S, McAlindon TE, et al. Risk factors for the
incidence and progression of radiographic knee osteoarthritis. Arthritis
32 Hungin AP, Kean WF. Nonsteroidal anti-inflammatory drugs: over-
used or underused in osteoarthritis? Am J Med. 2001;110:8S–11S.
14 Cerejo R, Dunlop DD, Cahue S, et al. The influence of alignment
33 Griffin MR, Piper JM, Daugherty JR, et al. Nonsteroidal anti-
on risk of knee osteoarthritis progression according to baseline stage of
inflammatory drug use and increased risk for peptic ulcer disease in
disease. Arthritis Rheum. 2002;46:2632–2636.
elderly persons. Ann Intern Med. 1991;114:257–263.
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1315
34 Grace D, Rogers J, Skeith K, Anderson K. Topical diclofenac versus
54 Fransen M, McConnell S, Bell M. Therapeutic exercise for people
placebo: a double blind, randomized clinical trial in patients with
with osteoarthritis of the hip or knee: a systematic review. J Rheumatol.
osteoarthritis of the knee. J Rheumatol. 1999;26:2659 –2663.
35 Drazen JM. COX-2 inhibitors: a lesson in unexpected problems.
55 Peloquin LBG, Gauthier P, Lacombe G, Billiard J-S. Effects of a
N Engl J Med. 2005;352:1131–1132.
cross-training exercise program in persons with osteoarthritis of theknee: a randomised controlled trial. J Clin Rheumatol. 1999;5:126 –136.
36 Nussmeier NA, Whelton AA, Brown MT, et al. Complications of the
COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery.
56 O'Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on
N Engl J Med. 2005;352:1081–1091.
pain and disability from osteoarthritis of the knee: a randomisedcontrolled trial. Ann Rheum Dis. 1999;58:15–19.
37 Psaty BM, Furberg CD. COX-2 inhibitors: lessons in drug safety.
N Engl J Med. 2005;352:1133–1135.
57 Fitzgerald GK, Oatis C. Role of physical therapy in management of
knee osteoarthritis. Curr Opin Rheumatol. 2004;16:143–147.
38 Solomon SD, McMurray JJ, Pfeffer MA, et al. Cardiovascular risk
associated with celecoxib in a clinical trial for colorectal adenoma
58 Falconer J, Hayes KW, Chang RW. Effect of ultrasound on mobility
prevention. N Engl J Med. 2005;352:1071–1080.
in osteoarthritis of the knee: a randomized clinical trial. Arthritis CareRes. 1992;5:29 –35.
39 Topol EJ. Arthritis medicines and cardiovascular events: "house of
coxibs." JAMA. 2005;293:366 –368.
59 Altman RD. Criteria for classification of clinical osteoarthritis.
J Rheumatol Suppl. 1991;27:10 –12.
40 Gottlieb S. COX 2 inhibitors may increase risk of heart attack. BMJ.
2001;323:471.
60 Kellgren J, Lawrence J. Radiological assessment of osteoarthrosis.
Ann Rheum Dis. 1957;16:494 –501.
41 Hughes R, Carr A. A randomized, double-blind, placebo-controlled
trial of glucosamine sulphate as an analgesic in osteoarthritis of the
61 Bellamy N. WOMAC Osteoarthritis Index: A User's Guide. London,
knee. Rheumatology (Oxford). 2002;41:279 –284.
Ontario, Canada: no publisher identified; 1995.
42 Richy F, Bruyere O, Ethgen O, et al. Structural and symptomatic
62 Bellamy N. WOMAC: a 20-year experiential review of a patient-
efficacy of glucosamine and chondroitin in knee osteoarthritis: a
centered self-reported health status questionnaire. J Rheumatol. 2002;
comprehensive meta-analysis. Arch Intern Med. 2003;163:1514 –1522.
43 Brosseau L, Yonge KA, Robinson V, et al. Thermotherapy for
63 Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of
treatment of osteoarthritis. Cochrane Database Syst Rev. 2003;(4):
WOMAC: a health status instrument for measuring clinically important
patient relevant outcomes to antirheumatic drug therapy in patientswith osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
44 Yurtkuran M, Kocagil T. TENS, electroacupuncture and ice mas-
sage: comparison of treatment for osteoarthritis of the knee. Am J
64 Bellamy N, Buchanan WW, Grace E. Double-blind randomized
controlled trial of isoxicam vs piroxicam in elderly patients withosteoarthritis of the hip and knee. Br J Clin Pharmacol. 1986;22(suppl
45 Welch V, Brosseau L, Peterson J, et al. Therapeutic ultrasound for
osteoarthritis of the knee. Cochrane Database Syst Rev 2001;(3):CD003132.
65 Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a
new measure of exercise capacity in patients with chronic heart failure.
46 Ettinger WH Jr, Burns R, Messier SP, et al. A randomized trial
Can Med Assoc J. 1985;132:919 –923.
comparing aerobic exercise and resistance exercise with a healtheducation program in older adults with knee osteoarthritis: the Fitness
66 Ouellet D, Moffet H. Locomotor deficits before and two months
Arthritis and Seniors Trial (FAST). JAMA. 1997;277:25–31.
after knee arthroplasty. Arthritis Rheum. 2002;47:484 – 493.
47 Baker KR, Nelson ME, Felson DT, et al. The efficacy of home based
67 Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve
progressive strength training in older adults with knee osteoarthritis: a
strength and physical function in patients with osteoarthritis: a ran-
randomized controlled trial. J Rheumatol. 2001;28:1655–1665.
domised controlled trial comparing a gym based and a hydrotherapybased strengthening programme. Ann Rheum Dis. 2003;62:1162–1167.
48 Deyle GD, Henderson NE, Matekel RL, et al. Effectiveness of
manual physical therapy and exercise in osteoarthritis of the knee: a
68 Maitland GD. Peripheral Manipulation. Boston, Mass: Butterworth-
randomized, controlled trial. Ann Intern Med. 2000;132:173–181.
Heinemann; 1991:1–128, 221–289.
49 Petrella RJ, Bartha C. Home based exercise therapy for older
69 Evjenth O, Hamberg J. Muscle Stretching in Manual Therapy: A Clinical
patients with knee osteoarthritis: a randomized clinical trial.
Manual. Milan, Italy: New Intherlitho; 1988:7–12, 89 –147.
J Rheumatol. 2000;27:2215–2221.
70 Maitland G, Hengeveld E, Banks K, English K. Maitland's Vertebral
50 van Baar ME, Dekker J, Oostendorp RA, et al. Effectiveness of
Manipulation. 6th ed. Boston, Mass: Butterworth-Heinemann; 2001:
exercise in patients with osteoarthritis of hip or knee: nine months'
follow up. Ann Rheum Dis. 2001;60:1123–1130.
71 Wallin D, Ekblom B, Grahn R, Nordenborg T. Improvement of
51 van Baar ME, Dekker J, Oostendorp RA, et al. The effectiveness of
muscle flexibility: a comparison between two techniques. Am J Sports
exercise therapy in patients with osteoarthritis of the hip or knee: a
randomized clinical trial. J Rheumatol. 1998;25:2432–2439.
72 Hicks JE. Exercise in patients with inflammatory arthritis and
52 Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for
connective tissue disease. Rheum Dis Clin North Am. 1990;16:845– 870.
patients with osteoarthritis of the knee: a randomized controlled
73 DiNubile NA. Strength training. Clin Sports Med. 1991;10:33– 62.
clinical trial. J Rheumatol. 2001;28:156 –164.
74 Bandy WD, Irion JM, Briggler M. The effect of static stretch and
53 van Baar ME, Assendelft WJ, Dekker J, et al. Effectiveness of exercise
dynamic range of motion training on the flexibility of the hamstring
therapy in patients with osteoarthritis of the hip or knee: a systematic
muscles. J Orthop Sports Phys Ther. 1998;27:295–300.
review of randomized clinical trials. Arthritis Rheum. 1999;42:1361–1369.
1316 . Deyle et al
Physical Therapy . Volume 85
. Number 12 . December 2005
75 Bandy WD, Irion JM, Briggler M. The effect of time and frequency
84 Watterson JR, Esdaile JM. Viscosupplementation: therapeutic mech-
of static stretching on flexibility of the hamstring muscles. Phys Ther.
anisms and clinical potential in osteoarthritis of the knee. J Am Acad
Orthop Surg. 2000;8:277–284.
76 Bandy WD, Irion JM. The effect of time on static stretch on the
85 Huskisson EC, Donnelly S. Hyaluronic acid in the treatment of
flexibility of the hamstring muscles. Phys Ther. 1994;74:845– 850;
osteoarthritis of the knee. Rheumatology (Oxford). 1999;38:602– 607.
discussion 850 – 852.
86 Ayral X. Injections in the treatment of osteoarthritis. Best Pract Res
77 Barr S, Bellamy N, Buchanan WW, et al. A comparative study of
Clin Rheumatol. 2001;15:609 – 626.
signal versus aggregate methods of outcome measurement based on
87 Leopold SS, Redd BB, Warme WJ, et al. Corticosteroid compared
the WOMAC Osteoarthritis Index. J Rheumatol. 1994;21:2106 –2112.
with hyaluronic acid injections for the treatment of osteoarthritis of
78 Ludica CA. Can a program of manual physical therapy and super-
the knee: a prospective, randomized trial. J Bone Joint Surg Am.
vised exercise improve the symptoms of osteoarthritis of the knee.
J Fam Pract. 2000;49:466 – 467.
88 Kirwan J. Is there a place for intra-articular hyaluronate in osteoar-
79 Mohomed NN. Manual physical therapy and exercise improved
thritis of the knee? Knee. 2001;8:93–101.
function in osteoarthritis of the knee. J Bone Joint Surg Am. 2000;82:
89 Kroesen S, Schmid W, Theiler R. Induction of an acute attack of
calcium pyrophosphate dihydrate arthritis by intra-articular injection
80 Fisher NM, Kame VD Jr, Rouse L, Pendergast DR. Quantitative
of hylan G-F 20 (Synvisc). Clin Rheumatol. 2000;19:147–149.
evaluation of a home exercise program on muscle and functional
90 Pullman-Mooar S, Mooar P, Sieck M, et al. Are there distinctive
capacity of patients with osteoarthritis. Am J Phys Med Rehabil. 1994;73:
inflammatory flares after hylan g-f 20 intra-articular injections?
J Rheumatol. 2002;29:2611–2614.
81 Chamberlain MA, Care G, Harfield B. Physiotherapy in osteoarthro-
91 Gosal HS, Jackson AM, Bickerstaff DR. Intra-articular steroids after
sis of the knees: a controlled trial of hospital versus home exercises. Int
arthroscopy for osteoarthritis of the knee. J Bone Joint Surg Br. 1999;81:
Rehabil Med. 1982;4:101–106.
82 Flanagan T, Green S. The concept of maintenance physiotherapy.
Aust J Physiother. 2000;46:271–278.
83 Flanagan T, Coburn P, Harcourt P, et al. Justifying the on-going
physiotherapy management of long-term patients. Man Ther. 2003;8:
254 –256.
Physical Therapy . Volume 85 . Number 12 .
Deyle et al . 1317
Physical Therapy Treatment Effectiveness for
Osteoarthritis of the Knee: A Randomized
Comparison of Supervised Clinical Exercise and
Manual Therapy Procedures Versus a Home
Program
Gail D Deyle, Stephen C Allison, Robert L Matekel,
Michael G Ryder, John M Stang, David D Gohdes,
Jeremy P Hutton, Nancy E Henderson and Matthew B
Garber
PHYS THER. 2005; 85:1301-1317.
This article cites 86 articles, 20 of which you can accessfor free at:
This article has been cited by 16 HighWire-hostedarticles:
Information
Information for Authors
Source: http://www.physiopoint.cc/fileadmin/images/inhalt/knee_OA_RCT_Deyle_2005.pdf
J Korean Neurosurg Soc 43 : 143-148, 2008 Incidence and Risk Factors of Acute Yoon-Sik Oh, M.D.1 Postoperative Delirium in Geriatric Dong-Won Kim, M.D.2 Hyoung-Joon Chun, M.D.1 Hyeong-Joong Yi, M.D.1 Objective : Postoperative delirium (POD) is characterized by an acute change in cognitive function and canresult in longer hospital stays, higher morbidity rates, and more frequent discharges to long-term care facilities.In this study, we investigated the incidence and risk factors of POD in 224 patients older than 70 years ofage, who had undergone a neurosurgical operation in the last two years.Methods : Data related to preoperative factors (male gender, >70 years, previous dementia or delirium, alcoholabuse, serum levels of sodium, potassium and glucose, and co-morbidities), perioperative factors (type ofsurgery and anesthesia, and duration of surgery) and postoperative data (length of stay in recovery room,severity of pain and use of opioid analgesics) were retrospectively collected and statistically analyzed.Results : POD appeared in 48 patients (21.4%) by postoperative day 3. When we excluded 26 patients with
Bull. Hiroshima Inst. Tech. Research Vol.49(2015)27-33 Inhibitory effect of cadmium on competitive nodulation ability of Bradyrhizobium japonicum Takashi OZAWA* and Kenji IJIRI** (Received Oct. 23, 2014) Competitive nodulation abilities of Bradyrhizobium japonicum strains USDA110ET and A1017ET were significantly depressed by growing the strains in yeast extract-mannitol broth supplemented with 2 μM CdCl2. Soybean seedlings were co-inoculated with each test strain and its competitor strain 138NR, and the bacteria in nodules formed on 21 days old plant roots were identified by the antibiotic resistant markers. Cell surface hydrophobicity of each test strain increased by growing the strains with 2 μM CdCl2, though definite increase in bacterial attachment to plant root surface was hindered by excessive secretion of exopolysaccharides of the strains. Polyacrylamide gel electro-phoresis revealed that growing the test strains in the medium with 2 μM CdCl2 induced the produc-tion of lipopolysaccharides of small molecular sizes. The results in this study suggest that cadmium of low concentration causes the weakening of competitive nodulation ability of rhizobia through in-hibition of the lipopolysaccharide synthesis.