Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Physics.isu.edu
The Radiological Accident in
Samut Prakarn
THE RADIOLOGICAL ACCIDENT
The following States are Members of the International Atomic Energy Agency:
AZERBAIJAN, REPUBLIC OF
REPUBLIC OF MOLDOVA
REPUBLIC OF TAJIKISTAN
IRAN, ISLAMIC REPUBLIC OF
RUSSIAN FEDERATION
BOSNIA AND HERZEGOVINA
KOREA, REPUBLIC OF
SYRIAN ARAB REPUBLIC
LIBYAN ARAB JAMAHIRIYA
THE FORMER YUGOSLAV
REPUBLIC OF MACEDONIA
DEMOCRATIC REPUBLIC
UNITED ARAB EMIRATES
UNITED KINGDOM OF
GREAT BRITAIN AND
DOMINICAN REPUBLIC
UNITED STATES OF AMERICA
FEDERAL REPUBLIC OF
The Agency's Statute was approved on 23 October 1956 by the Conference on the Statute of the
IAEA held at United Nations Headquarters, New York; it entered into force on 29 July 1957. TheHeadquarters of the Agency are situated in Vienna. Its principal objective is "to accelerate and enlarge thecontribution of atomic energy to peace, health and prosperity throughout the world''.
Permission to reproduce or translate the information contained in this publication may be
obtained by writing to the International Atomic Energy Agency, Wagramer Strasse 5, P.O. Box 100,A-1400 Vienna, Austria.
Printed by the IAEA in Austria
THE RADIOLOGICAL ACCIDENT
INTERNATIONAL ATOMIC ENERGY AGENCY
VIC Library Cataloguing in Publication Data
The radiological accident in Samut Prakarn. — Vienna : International Atomic
Energy Agency, 2002.
1. Radiation injuries—Samut Prakan (Thailand : Province).
— Physiological effect. 3. Radioactivity — Physiological effect. 4. Nuclearindustry — Samut Prakan (Thailand : Province) I. International AtomicEnergy Agency.
The use of radioactive materials offers a wide range of benefits throughout the
world in medicine, research and industry. Precautions are, however, necessary to limitthe exposure of people to the radiation that is emitted. Where the amount ofradioactive material is substantial, as in the case of radiotherapy sources or industrialradiography sources, extreme care is needed to prevent accidents which may havesevere consequences. Nevertheless, in spite of the precautions taken, accidents withradiation sources continue to occur, although infrequently. As part of its activities onthe safety of radiation sources, the IAEA conducts follow-up reviews of such seriousaccidents to give an account of their circumstances and of the medical aspects, fromwhich organizations with responsibilities for radiation protection and the safety ofsources may learn.
A serious radiological accident occurred in Samut Prakarn, Thailand, in late
January and early February 2000 when a disused 60Co teletherapy head was partiallydismantled, taken from an unsecured storage location and sold as scrap metal.
Individuals who took the housing apart and later transported the device to a junkyardwere exposed to radiation from the source. At the junkyard the device was furtherdisassembled and the unrecognized source fell out, exposing workers there. Theaccident came to the attention of the relevant national authority when physicians whoexamined several individuals suspected the possibility of radiation exposure from anunsecured source and reported this suspicion. Altogether, ten people received highdoses from the source. Three of those people, all workers at the junkyard, died withintwo months of the accident as a consequence of their exposure.
Under the Convention on Assistance in the Case of a Nuclear Accident or
Radiological Emergency, the Thai authorities requested advice from the IAEA on themedical treatment of the exposed people. Subsequently, they invited the IAEA toassist in a review of the accident. The IAEA is grateful to the Thai authorities and thephysicians of the Samut Prakarn Hospital in Samut Prakarn Province and theRajavithi Hospital in Bangkok for their assistance in the preparation of this report.
The IAEA technical officers responsible for the preparation of this publication
were J.G. Yusko, B. Dodd and I. Turai of the Division of Radiation and Waste Safety.
EDITORIAL NOTE
This report is based on information made available to the IAEA by or through the
authorities of Thailand. Neither the IAEA nor its Member States assume any responsibility forconsequences which may arise from its use.
The report does not address questions of responsibility, legal or otherwise, for acts or
omissions on the part of any person.
The use of particular designations of countries or territories does not imply any
judgement by the publisher, the IAEA, as to the legal status of such countries or territories, oftheir authorities and institutions or of the delimitation of their boundaries.
The mention of names of specific companies or products (whether or not indicated as
registered) does not imply any intention to infringe proprietary rights, nor should it beconstrued as an endorsement or recommendation on the part of the IAEA.
Material made available to persons who are in contractual relation with governments is
copyrighted by the IAEA, as publisher, only to the extent permitted by appropriate nationalregulations.
BACKGROUND INFORMATION . . . . . . . . . . . . . . .
2.1. Radiation protection infrastructure . . . . . . . . . . . .
2.3. The non-licensed supplier . . . . . . . . . . . . . . . .
3.1. Description of the accident . . . . . . . . . . . . . . .
3.2. Discovery and notification . . . . . . . . . . . . . . . .
RADIOPATHOLOGICAL CONSIDERATIONS . . . . . . . . .
4.2. Treatment and clinical progression of patients
4.3. Treatment and clinical progression of patients
FINDINGS, CONCLUSIONS AND LESSONSTO BE LEARNED . . . . . . . . . . . . . . . . . . . . .
5.1. Operating organizations . . . . . . . . . . . . . . . .
5.3. International co-operation . . . . . . . . . . . . . . . .
CONTRIBUTORS TO DRAFTING AND REVIEW . . . . . . . . . .
A common use of high activity 60Co sources around the world is in the treatment
of cancer patients (radiotherapy). In Thailand alone there are 20 radiotherapy centres,which have a total of 25 teletherapy units. Intense beams of penetrating gammaradiation are needed to treat cancer; hence, high energy and high activity sources areused in specially designed machines to deliver the radiation dose in a controlled manner.
The intensity of the radiation decreases over time, however, and the sources need to bereplaced to avoid long treatment times. The services of specialist companies arenormally used to exchange the sources and maintain the equipment.
One company based in Bangkok, Thailand, possessed several teletherapy
devices without an authorization from the Thailand Office of Atomic Energy forPeace (OAEP). In the autumn of 1999, the company relocated the teletherapy headsfrom a warehouse it had leased to an unsecured storage location, also without theauthorization of the Thai authorities and without informing OAEP of this relocation.
In late January 2000, several individuals obtained access to the unsecured
storage location and partially disassembled a teletherapy head. They took the unit tothe residence of one of the individuals, where four people attempted to disassembleit further. The teletherapy head displayed a radiation trefoil and warning label.
However, the individuals did not realize that this indicated radioactive material, andthe warning label was not in a language they understood. On 1 February 2000, two ofthe individuals took the partially disassembled device to a junkyard in Samut Prakarn,Thailand, so that the component metals could be segregated and sold separately.
While a worker at the junkyard was disassembling the device using an oxyacetylenetorch, the source fell out of its housing, unobserved by either the junkyard workers orthe individuals involved.
By the middle of February 2000, several of the individuals involved had begun
to feel ill and sought medical assistance. Physicians at a local hospital recognized thesigns and symptoms of several of the patients and suspected that an unsecuredradiation source was the cause. They reported their suspicions to the regulatoryauthority (OAEP). Personnel from the regulatory authority, assisted by local publichealth personnel, searched for the source. When high radiation levels were found inthe vicinity of the junkyard, they secured the area to prevent further access. Anemergency response team was assembled, and by 20 February 2000 the source wasrecovered and transported to a secure storage area and the emergency terminated.
Examination showed that the source capsule had not been breached and there was nocontamination of the environment. The activity of the recovered source was estimatedat 15.7 TBq (425 Ci) of 60Co.
Under the Convention on Assistance in the Case of a Nuclear Accident or
Radiological Emergency, the Thai authorities requested advice from the IAEA on themedical treatment of the exposed people. The IAEA is authorized to establishstandards for radiation protection and for the safety of sources of radiation, and toassist in their application. The International Basic Safety Standards for Protectionagainst Ionizing Radiation and for the Safety of Radiation Sources (BSS) [1] establishthe requirements for protection and safety. It is presumed that States have an adequatelegal and regulatory infrastructure within which the requirements can be appliedeffectively. Requirements and guidance for the establishment of an appropriateinfrastructure and other relevant matters are issued in the IAEA Safety StandardsSeries (see also Ref. [2]).
For a number of years the IAEA has provided support and assistance under the
Convention on Assistance in the Case of a Nuclear Accident or RadiologicalEmergency, and conducted follow-up investigations upon request, in the event ofserious accidents involving radiation sources. Reports have been published on follow-up investigations of radiological accidents in San Salvador [3], Soreq [4], Hanoi [5],Tammiku [6], Goiânia [7, 8], Lilo [9], Yanango [10] and Istanbul [11]. The findingsand conclusions of these reports have provided a basis for learning lessons on safetyimprovements [12–14].
The Thai authorities subsequently invited the IAEA to assist in a review of the
accident. The objective of this report is to compile and disseminate information aboutthe causes of the accident, the subsequent emergency response and the early medicalaspects of the overexposures. With the dissemination of the lessons to be learned,Member States may be able to identify similar or precursor situations and take thenecessary actions to prevent comparable accidents from occurring.
The information in this report is intended for the use of national authorities and
regulatory bodies, emergency planners and a broad range of specialists, includingphysicists, technicians and medical specialists, and persons responsible for radiationprotection. The report ends with findings, conclusions and lessons to be applied inorder to help avoid such accidents in the future and to minimize the consequences ofany that do occur.
This publication gives an account of the events reported to have occurred
leading up to and following the accident, and the remedial measures reportedly taken
thereafter. A number of uncertainties remain in relation to these events. There mayalso be further developments in terms of health consequences for those severelyexposed.
The report also presents information relevant to licensees and operating
organizations involved in the supply, storage and transport of high activity radioactivesources. The findings of this report and lessons to be learned from this accident willalso be of interest to radiation protection staff and the medical community.
Background information about the radiation protection infrastructure in
Thailand, the company involved in the accident and details about the source areprovided in Section 2. An account of the reported events leading up to the accident,of the discovery of the accident, and of the emergency response to the accident,including the recovery of the source, the response by OAEP and the local publichealth authorities, as well as the IAEA's response in providing assistance, is providedin Section 3. The medical treatment of the severely exposed individuals is describedin Section 4 and is targeted towards physicians and other medical personnel.
Findings, conclusions and lessons to be learned are presented in Section 5.
2. BACKGROUND INFORMATION
2.1. RADIATION PROTECTION INFRASTRUCTURE
The Office of Atomic Energy for Peace (OAEP) is the body responsible to the
Thai Atomic Energy Commission for Peace (AEC). The AEC is the regulatoryauthority for Thailand and was established by the Atomic Energy for Peace Act,1B.E. 2504 (1961) and B.E. 2508 (1965), and Ministerial Regulation No. 1 (1961), No.
2 (1961), No. 3 (1961), No. 4 (1968), No. 5 (1973) and No. 6 (1974). These acts andregulations involve several ministries, commissions and offices in the regulation ofradiological safety, and the structure is such that it apparently resulted in gaps oroverlapping roles for certain regulatory activities.
1 Atomic Energy for Peace Act (B.E. 2504 (1961) and B.E. 2508 (1965)) is the basic
legislation for the regulation of nuclear and radioactive materials and industrial uses of X rays.
Medical uses of X rays are regulated by the Ministry of Public Health, under MinisterialRegulation No. 4 (B.E. 2511) of the same Act.
The Thai AEC has eight subcommittees, one of which deals with the licensing
of radioisotopes and nuclear materials. It also has responsibility for the developmentand promotion of atomic energy as well as for regulatory needs. All theresponsibilities of the AEC are carried out by the OAEP.
The Ministry of Science, Technology and Environment is involved in
administering the personnel, budget and facility management, as well as research anddevelopment activities conducted by the OAEP.
Reporting to the AEC is a Subcommittee for Licensing of Radioisotopes and
Nuclear Materials. This is composed of OAEP members, and carries out its functionsunder the mandate of Ministerial Regulation No. 2 (B.E. 2504). The Health PhysicsDivision within the OAEP conducts regulatory activities through its LicensingSection and its Radiation Protection Section.
The OAEP is responsible for about 650 licences for the possession and use of
radioactive materials in Thailand. Licences generally are valid for one year. Thelicensing process involves the regulatory authority in determining the safety andadequacy of the facility where the radioactive materials are intended for use andchecking that the qualifications of the users are satisfactory. The OAEP reports thatin general inspections are intended to be carried out annually. The inspection priorityis based on the level of risk the radioactive material presents, according to anunofficial classification2 by the OAEP. It also depends on the availability of personnelresources to accomplish this task. Moreover, the OAEP issues licences for the importand export of radioactive materials. At the time of the accident, eight inspectors wereresponsible for checking all radiation source licensees, and the OAEP reported that,as a consequence of their workload, the annual performance inspections of licenseescould not be performed effectively.
According to the Atomic Energy for Peace Act, no fees are imposed on
licensees. If a licence is withdrawn and the licensee still possesses radioactivematerial, OAEP guidelines provide options for the licensee. The licensee may decideto keep a disused source at a storage location authorized by the OAEP, to transfer itto an authorized legal person, or to send it to be disposed of at the OAEP. For the lastchoice, a licensee from the private sector must pay the OAEP to recover and store theradioactive material. However, with the authorization of the OAEP, the licensee maytransfer or otherwise dispose of the radioactive materials to an authorized legal personas a means of terminating use and the licence. According to OAEP regulations, oneof the requirements of a licence is that licensed sources are not to be relocated withoutthe OAEP's authorization.
2 For example, priorities were based on source strength and use, and were ranked in the
following (descending) order: radiography; teletherapy and brachytherapy; irradiation forsterilization and preservation.
The OAEP had begun a review of its regulations and of the requirements
imposed on its licensees in the late 1980s. Starting in 1989, it began imposingconditions on the training requirements for personnel and for improved safety andsecurity measures and storage conditions, as well as for the use of radiologicalinstrumentation and for personal dosimetry services. The OAEP stated that it hadused then extant IAEA guidelines as its basis for these changes.
2.2. THE LICENSED HOSPITAL
The device involved in the accident was installed originally at a hospital in
Bangkok (RT hospital) in 1969. In 1981, after patient treatment times becameimpractical, a new source was installed. The new source had an initial activity of196 TBq (5300 Ci) of 60Co, and it was this new source that was ultimately involvedin the accident.
Following replacement of the source in 1981, the hospital did not obtain any
further service from Siemens, the manufacturer of the teletherapy unit and source.
The local Siemens agent who had been contracted to do maintenance on the unit laterdeclared bankruptcy. The teletherapy unit was reported to have been taken out ofservice in 1994, presumably when the patient treatment times again became too longto be practical.
2.3. THE NON-LICENSED SUPPLIER
When the unit was removed from service, Siemens was no longer
manufacturing 60Co teletherapy units. The hospital contacted Nordion, amanufacturer of teletherapy devices in Canada, through its agent in Thailand (KSECompany) to supply a new teletherapy unit. However, Nordion could not accept thereturn of the disused source to Canada since it was not the original manufacturer. Thismeant that the hospital would have been left with a disused source to manage andcontrol, as required by the regulatory body. Since the hospital did not have sufficientstorage space for the old teletherapy unit containing the disused source, it sold thedevice and source to the new supplier agent (KSE Company). The hospital reportedlydid not inform the OAEP of the transfer of this radiation source and KSE did notinform the OAEP of its possession of the disused radiotherapy unit.
At this time KSE already possessed one therapy unit, imported from Canada in
1974 for a physician. The physician, however, had asked the company to store it until
he found a suitable facility3 in which to install it. The OAEP had issued a licence in1988 for the company to store this teletherapy unit in a warehouse that they leased inthe Bangkok area.
In 1993, KSE notified the OAEP of its need to expand its storage facility in
Bangkok for more foreseeable disused (teletherapy) units. Before the OAEPresponded to this request, KSE modified the notification by proposing to move thedisused sources it had acquired to a new storage location in Petchaboon Province,approximately 400 km north of Bangkok. This new proposal described the intendedfacility as a storage building to be constructed on empty land. The regulatoryauthority felt that the location was not sufficiently secure, and advised the companyto store the sources in or around Bangkok. The OAEP reportedly informed thecompany of its radiation protection guidelines and also advised the company either toobtain a licence for the sources or to transfer its sources to the OAEP for storage.
In 1996, KSE applied to the OAEP for a licence to export two 60Co sources to
Nordion. These two other sources were also spent teletherapy sources which had beenin storage and were to be shipped back to Canada. An OAEP inspection, performedprior to the shipment of these sources, apparently disclosed that KSE had three othersources in addition to the licensed source which belonged to the physician.
KSE thus had four radiation therapy units in the warehouse. One belonged to
the above mentioned physician and had been in storage since 1974. Two other units(one originally from Japan and the other from Germany) had been used ingovernment medical institutions and were transferred to KSE when they were nolonger of use. The fourth unit was that imported from Siemens in 1969 (butcontaining the replacement source dating from 1981).
Early in 1999, KSE was notified that its lease of the warehouse was to be
terminated. The company was obliged to relocate the four sources that it possessed.
The company returned the source belonging to the physician and notified the OAEPafter the relocation. However, without reportedly obtaining authorization from theOAEP or notifying it, KSE moved the other three sources to a car parking lot that wasowned by KSE's parent company. It was from this location that one of the sourceswas reportedly stolen. According to local residents, the sources were moved to the carparking lot in October 1999.
The car parking lot had been used by KSE's parent company to store new
vehicles after their assembly in Thailand but was vacant at the time of the accident. Aportion of the lot was roofed to protect vehicles. The source housings were storedunder the roofed area. The car parking lot was fenced (with galvanized steel sheet);however it was not secure. Gaps had been made in the fences and residents of
3 The OAEP had denied a licence for a proposed facility citing inadequate and/or
apartments across the street played football in the open space of the parking lot nearthe stored sources.
2.4. THE DEVICE AND ITS SOURCE
The device involved in the accident was a Gammatron-3 teletherapy unit,
manufactured by Siemens of Germany. It was originally exported to Thailand in 1969and had undergone at least one source change. The last change occurred in 1981,when a source of 196 TBq (5300 Ci) was installed. At the time of the accident, theactivity was estimated to be 15.7 TBq (425 Ci).
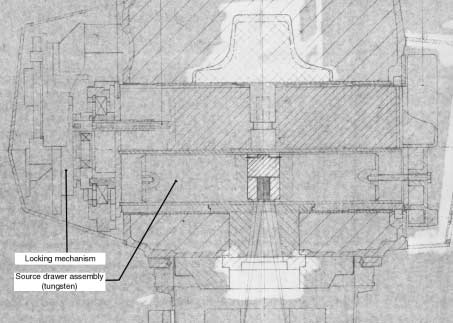
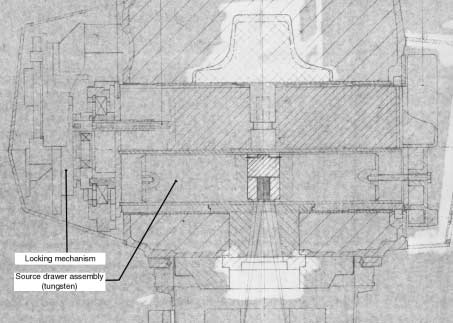
The source holder (and shield) is of lead surrounded by stainless steel. It is
cylindrical, 42 cm long by 20 cm diameter. The lead is 5 cm thick, with a weight of97 kg, within a stainless steel casing that weighed an additional 30 kg. Figure 1 showsthe teletherapy unit head and its source assembly.
FIG. 1. The Siemens Gammatron-3 teletherapy head (cutaway side view). The lighter area inthe centre is the source. Note the two cylindrically shaped objects around the source.
3. THE ACCIDENT
3.1. DESCRIPTION OF THE ACCIDENT
Patient 1 (P1)4 (a 40 year old male5) and P2 (a 25 year old male), who were
working as scrap collectors, claimed that on 24 January 2000 they bought some scrapmetal (which included part of a teletherapy head) and took it home for dismantlingfor resale. P1 used a motor driven cart (known in Thailand as a tricycle) as the vehiclefor carrying the materials. The batch of scrap metal was kept in an open space about100 m from P1's residence until the end of January 2000 (Fig. 2).
FIG. 2. Map of the sites (1: car parking lot; 2: P1 residence; 3: junkyard; 4: hospital).
4 Pn = Patient identification number; see Table II for a brief description of the
5 The names of the patients have been omitted to maintain confidentiality.
On 1 February 2000, P1, together with P2, P3 (a 19 year old male) and P4 (a
23 year old male and younger brother of P1's wife), reportedly tried to dismantle part6of the cylindrical metal piece of the teletherapy head, which was covered by stainlesssteel. This action took place at P1's residence. P2 and P4 worked for about an hourtrying to separate the steel and the lead using a hammer and chisel. Most of this workwas done by P2. They were able only to crack the weld seam, whereupon they noticedan oily liquid seep out. They could, however, see the lead inside the stainless steelbox.
P1 then told them to stop and decided to take the metal to a junkyard for sale
there. P1 and P3 brought the lead cylinder and other metal pieces to a junkyardlocated at Soi Wat Mahawong, Samut Prakarn Province. On the trip from P1's home,which took about 30 minutes, P3 was sitting in the cart with his (right) leg drapedover the cylindrical metal piece (Figs 3 and 4).
FIG. 3. The teletherapy head with the missing source drawer assembly.
6 This part was later discovered to be the source drawer of the teletherapy unit.
FIG. 4. Cylindrical pieces from the source assembly (the item at left is hollow; it previouslysurrounded the 60Co source).
At the junkyard, P1 reportedly requested P5 (a 23 year old male), a junkyard
employee, to cut open the cylinder with an oxyacetylene torch. Another junkyardemployee, P6 (an 18 year old male), was working nearby, positioned behind P5. P5successfully cut open the stainless steel box and the lead cylinder. He saw yellowsmoke which "smelled bad" and saw two metal pieces from inside the cylinder fall tothe ground. P5 picked up these pieces and weighed them in his hands. He laterreported that his hands felt "itchy" from handling these pieces. These metal piecesfrom the cylinder were kept at the junkyard. P5 felt uneasy about the smoke andstopped cutting, but could not completely dismantle the stainless steel and leadmaterials. P7 (a 45 year old female and owner of the junkyard) watched the work andtold P1 to take the cylinder back to his residence to continue the work there. P1 tookthe items back and left them in his vehicle overnight. On the way back to hisresidence on 1 February 2000, P1 started to experience severe headache and nausea.
P3 also felt nauseous and felt an itching sensation on his legs. P5 and P6 started tofeel dizzy, had bad headaches and not long afterwards started to vomit. P1 and P3successfully separated the metal into 40 kg of stainless steel and 72 kg of lead and P1reportedly brought these to the junkyard for sale on 2 February 2000.
P5 and P6 did not work on 3–4 February 2000 because of the Chinese New Year
holiday. P6 went home during this holiday. His father subsequently said that his sonhad looked ill, had lost his appetite and lost weight, and had a sunburn type burn on
his skin. Although P5 and P6 felt sick, they resumed work again on the next workingday, 7 February 2000.
On 12 February 2000, P7 reportedly asked P1 to sell the lead at another place,
presuming that the metal P1 had brought might be the cause of the illness of heremployees. She also asked another scrap collector to throw away the two smallcylindrical metal pieces. P1 had developed a burn on his hands, swollen fingers andan itchy palm, and went to see a doctor in a private clinic.
On 15 February 2000, P1 visited the outpatient clinic of the Samut Prakarn
Hospital for an examination. A blood sample was taken and the doctor requested himto return the next day when the blood examination results would be ready. Upon hisreturn, on 16 February 2000, P1 was admitted to the hospital. His burned hands wereswollen and had become darkened. He had nausea, vomiting and some localized lossof hair.
Meanwhile, P5 and P6 had been suffering from diarrhoea, which was being
controlled by medication.7 P5 felt weak and had a fever. He had lost weight, his hairwas falling out and he had burned hands. He too went to see a physician at the SamutPrakarn Hospital because of these symptoms. After a physical examination was madeand a blood sample was taken, he was admitted to Samut Prakarn Hospital on16 February 2000.
On 17 February 2000, P7, the junkyard owner, took P6 to Samut Prakarn Hospital
because of his weakness, weight loss and hair loss and he was admitted. When P7expressed her concern about her workers to the physician, he reportedly suggested thatsomething unusual was occurring at the junkyard. Subsequently, P7 took P9 (a 33 yearold female) to Samut Prakarn Hospital, where she was admitted for observation. P9 wasa maid to both P7 and P8, as well as a part time worker at the junkyard.
Later, P7 and her husband P8 (a 44 year old male), who were both feeling weak,
went to see a physician at Bangkok General Hospital. Blood samples taken from P7and P8 both showed low white blood cell counts, and a bone marrow aspiration wasperformed on both patients. At this time, the physician decided not to have P7admitted to the hospital, but P8, who had severe nose bleeding, was admitted. Duringthis time, P7 also reportedly mentioned that a stray dog that had often been in thejunkyard had died.
In summary, P1, P2, P3 and P4 were the individuals who had reportedly
obtained the teletherapy head on or about 24 January 2000. P5, P6, P7, P8 and P9were workers at the junkyard, including the owner, P7, and her husband, P8. P9 wasthe maid as well as a part time worker at the junkyard who lives with P7 and P8. Theirresidence is situated across the street from the junkyard. Finally, P10 is the 75 year
7 Since the diarrhoea was being controlled by medication, the radiation dose received
by these individuals was probably less than 10 Gy, although it will have exceeded 6 Gy.
old mother of the owner, who also lived with her daughter (P7) and son in law (P8).
P10 was attending to the workers at the junkyard regularly.
By 17 February 2000, P1, P5 and P6 had been admitted to Samut Prakarn
Hospital and P8 had been admitted to Bangkok General Hospital.
3.2. DISCOVERY AND NOTIFICATION
P1 and P5 had been seen at the surgical ward of Samut Prakarn Hospital. Both
had swollen fingers and were nauseous and vomiting. P5 also had a low white bloodcell count. P6 was seen at the medical ward, also showing nausea and vomiting, andhe also had a low white blood cell count. The physicians reviewed the cases of thesethree individuals who were demonstrating very similar symptoms. This led them tothe realization that these patients may have been exposed to ionizing radiation. Oncoming to this conclusion, at around 11:10 local time on 18 February 2000, one of thephysicians called the OAEP about the three patients and expressed his concern abouta possible unsecured radiation source in the environment.
The OAEP reported that, upon receipt of the call, they immediately dispatched
two officers (health physicists) who arrived at the Samut Prakarn Hospital at 12:30 on18 February 2000 to investigate the cases further. The OAEP officers met with thetreating physicians and with patients P5 and P6. The physicians provided the officerswith a description of their patients' symptoms and repeated their suspicion that anunsecured radiation source was present in the local environment. P7 was later calledto the hospital for questioning.
From the information provided by P7, the OAEP officers, jointly with local
public health officers, initiated a search to find the two small metal pieces that hadbeen given to the other scrap collector. This was done in the belief that one of thesesmall metal pieces was the source. The officers met the scrap collector and togetherthey went to search a public U-shaped concrete drainage point identified by the scrapcollector as the place where he had dumped the small pieces. They found the smallmetal pieces, but a radiation survey showed that they were not radioactive.
Since these two pieces of metal were not the radiation source, the officers went
to check the junkyard. During their journey towards the junkyard the officers had theirradiation detectors switched on. Around 19:00 on 18 February 2000, while drivingthrough one of the streets of Samut Prakarn district in the direction of the junkyard,they noted a significant increase in radiation levels (about 20 times normal). Theycontinued moving through two small back streets for about another 150 m or so untilthey reached the junkyard. There, a radiation level of about 1 mSv/h was measured atthe side entrance of the yard, confirming the presence of an intense gamma source. Atthis point they recognized that this was a serious radiological accident and called forassistance (Figs 5–7).
Unshielded source
Radiation levels encountered at the junkyard.
FIG. 6. Plan of the junkyard and its vicinity.
Elevated view of the junkyard. Scrap piles are on the left; the building in the centre
is the junkyard office, the building across the street is the residence of P7 and P8 (junkyardowner and husband) in which P9 (maid and part time junkyard worker) and P10 (mother ofP7) also resided.
3.3. RESPONSE AND RECOVERY
Recognizing the seriousness of the radiological situation, the OAEP officers
called upon an emergency response team. A command and co-ordination post wasthen established in the vicinity of the junkyard. In addition to a radiation level survey,contamination surveys were also carried out. No contamination was found. From thissurvey, the emergency response team concluded that the accident involved a sealedradioactive source of unknown size, either from an industrial radiography device orfrom a medical treatment machine. The radiation level survey found a dose rate of upto 10 Sv/h in the junkyard around the pile of scrap where the source was located.
Reportedly, the evacuation of residents was considered by both the OAEP and
the public health authorities. They reviewed the radiation survey data and concludedthat evacuation was not necessary as the radiation was isolated and confined only tothe junkyard, and, in their judgement, evacuation would cause confusion or panicamong those affected. Therefore, swift action to abate the problem was the preferredcourse. Accordingly, the local area was cordoned off at a radiation level of 300 µSv/h,which occurred about 10 m from the junkyard. Access to the junkyard was restrictedand the street outside was closed to traffic. The very high radiation level prevented theemergency response team from getting close enough to pinpoint the exact location ordetermine the physical shape of the source among the scrap material.
Further field operations to locate the source continued throughout the night
until 04:00 on the morning of 19 February 2000. The operation was recorded with avideo camera. It was then decided to suspend operations until later that morning andthe police secured the entire area (Fig. 8).
Later on the morning of 19 February 2000, the local public health authorities
resumed recovery operations at the junkyard. At approximately 150 m from thejunkyard, a dose rate of 1.7 µSv/h was measured. This level increased to 200 µSv/h onthe sidewalk across from the junkyard at a distance of approximately 20 m from thesource.
Meanwhile, the emergency response team recovery operation resumed its
activities at the OAEP. Personnel watched the videotapes taken the previous nightand planned the retrieval operations, and gathered the necessary tools and equipmentfor the source recovery. The team then returned to the junkyard around 14:00. Afterdiscussions with the local public health authorities and with the provincial civildefence group, a retrieval plan was agreed upon. Actual source retrieval operationscommenced around 16:00. The planning included rehearsals using a dummy object inorder to familiarize emergency response team members with the tools and techniquesfor retrieving the unknown source when it was finally located.
The Samut Prakarn Provincial Civil Defence Unit assisted in making available
the necessary machines and equipment (a mechanical excavator, a back hoe and largespotlights). The support of the local fire brigade was also obtained.
FIG. 8. Back hoe/front loader moving a lead barrier for use in recovery operations (takenfrom a video image).
To clear a path to the location of the source within the junkyard, a heavy iron
fenced entry gate and some scrap were removed with the help of a mechanicalexcavator. This excavator was also used to place a lead wall 5 cm thick by 1 m wideby 2 m high near the source to provide some shielding to individuals trying to findand recover the source. The dose rate behind this shield was reduced more thantwenty-fold. Spotlights and two closed circuit television (CCTV) cameras andmonitors were installed to facilitate the operation (Fig. 9).
As some of the participants in the recovery operation insisted on wearing lead
aprons for protection against the radiation emitted from the source, lead apronssuitable for diagnostic radiological procedures were obtained and worn by some ofthe team members. Note, however, that the protection afforded by these lead apronsis not adequate against the highly penetrating photons from the 60Co source. Theymay even slow down an individual's movements, which may result in increasedexposure. Moreover, the aprons may provide a false sense of security. Reportedly, theOAEP did not agree with the use of the lead aprons, but acquiesced in order to easeworkers' fears.
To gain access to the suspected location of the source, large pieces of scrap near
the source location were removed with a long grasping tool. In the process, each piecewas surveyed using a teledetector to ensure that there were not unexpectedly highradiation levels. Smaller pieces of metal on the ground that were in the likely vicinity
View of the junkyard rigged for night time operations (taken from a video image).
of the source also needed to be screened as part of the sorting process. For thispurpose, an ad hoc scrap screening system was improvised.
Pieces of scrap would be removed from the pile using an electromagnet at the
end of a 5 m bamboo pole and brought to a large washtub in which the high rangeradiation dose rate probe was placed. The detector output was led into its surveymeter by means of a 30 m long cable, and the operator would watch the meter readoutto determine whether he had picked up the actual source. The emergency responseteam calibrated this improvised system in their planning exercises. Located near thewashtub was a lead shielded container (of thickness 8.5 cm) into which the source, iffound, could be placed. After six operations of removing scrap metal, much of theoverburden metal was removed. The exact location of the source could still not bedetermined, however, owing to pieces of metal nearby.
Finally, in an effort to locate the source accurately, a fluorescent screen was
used. The fluorescent screen was of a size suitable for image intensification fordiagnostic X ray films. However, even with the floodlights turned off, the moonlightwas so bright that the source could not easily be located with the fluorescent screen.
Personnel had to wait until the moonlight had diminished for suitable darkness inwhich to use the screen accurately. At around 21:00 on 19 February 2000, the positionof the source within the remaining pile of scrap was accurately determined. However,many pieces of scrap metal still surrounded the source (Fig. 10).
FIG. 10. A luminescent screen was used to determine the location of the source accurately(taken from a video image).
Having now located the source, OAEP emergency response team personnel
innovated a means of retrieving it by attaching an electromagnet to a length ofbamboo. Other grasping tools were not long enough to afford adequate personnelprotection, and spending time trying to grapple the source with tongs would haveresulted in personnel receiving radiation doses from the intense radiation field.
On 20 February 2000 at 00:20, the source, which had been estimated to be
about 4 cm long and 2.5 cm in diameter, was retrieved. Tongs 2 m in length were usedto pick up the source and place it into a lead shielded container (Fig. 11). Theradiation levels in the scrap pile and the yard were surveyed again after removal ofthe source and container. Only background radiation levels were found, confirmingthat the source had been successfully removed. In situ gamma spectrometry wasperformed and the source was identified to be 60Co. The source activity was estimatedat roughly 15.7 TBq (425 Ci).
The source was transported to safe storage at the OAEP on 20 February 2000.
The lead container containing the source was placed under 4.5 m of water in what wasformerly a spent fuel storage pool (Fig. 12).
Individual thermoluminescent dosimeters (TLDs) were employed for dose
control purposes during the source recovery operations, and the results of thedosimetry are summarized in Table I. The maximum individual dose recorded for theemergency workers was reported as 32 mSv.
FIG. 11. Transfer of the retrieved source to a shielded transport container (taken from a videoimage).
FIG. 12. Storage location of the retrieved source.
During the operation to retrieve the source, the emergency response team was
informed that three radiation machines had been found in a parking lot in a suburbanarea of Bangkok. They dispatched officers to this site to assess the situation. Aftervisual and radiological inspection, the OAEP officers concluded that these machineswere 60Co teletherapy units and that the lead cylinder that would have contained thesource was missing from one of the units. It was later confirmed that this was the lead
TABLE I. DOSES RECEIVED DURING RECOVERY OF THE SOURCE
Number of individuals in group
10–20 620–32 6
cylinder involved in the accident. On 21 February 2000, all three machines (two ofwhich contained sources) were removed to be kept at the OAEP for temporary storage(Fig. 13).
During this whole operation, the OAEP emergency response team was given
full support by the Samut Prakarn Provincial Civil Defence Unit and by the SamutPrakarn Provincial Public Health Care Unit.
3.4. INVOLVEMENT OF THE IAEA
On 21 February 2000, the OAEP contacted the IAEA and, under the terms of
the Convention on Assistance in the Case of a Nuclear Accident or RadiologicalEmergency, described the accident and the successful recovery of the source. Thiswas followed by additional reports to the IAEA on 31 March and 26 April 2000 whichprovided information on the total number of previously unsecured disusedradiotherapy sources and the total number of victims of the accident and their medicalstatus. The second report also informed the IAEA of three subsequent fatalities and
FIG. 13. The three teletherapy heads at the car parking lot. The unit in the foreground was thedevice from which the source drawer assembly (containing the source) was removed.
the results of the screening of the population in the vicinity of the accident site thatwas conducted by the Ministry of Public Health.
On 24 February 2000, the Permanent Mission of Thailand in Vienna, on behalf
of the Thai Government, requested that the IAEA dispatch a team of experts inmedicine and radiation protection to share its expertise with the Thai authorities inBangkok. The IAEA acknowledged receipt of the request under the terms of theConvention on Assistance in the Case of a Nuclear Accident or RadiologicalEmergency and assembled a team, which arrived on 26 February 2000 and stayedfor a week. The team consisted of two IAEA staff members trained in radiationprotection and emergency response management and three medical doctorsfrom Japan who specialize in the treatment of radiation victims. The teamdiscussed the situation with the OAEP and others involved and provided feedbackand advice as appropriate, particularly with further regard to the care and treatmentof the injured.
In addition, the IAEA prepared this report with the assistance of representatives
from the OAEP and the attending physicians from Rajavithi Hospital.
4. RADIOPATHOLOGICAL CONSIDERATIONS
This section provides details of the radiopathology for the people who were
exposed, and is intended to be of interest primarily to medical staff.
From the description of the accident provided (see Section 3), it can be seen
that, although part of the teletherapy unit was reportedly removed on 24 January 2000and taken to a location near the residence of P1, the source remained in a shieldedcondition. Only on 1 February 2000 did P1 and his friends try to separate the deviceinto smaller components. Therefore, the sequence of severe radiation exposuresbegan on 1 February 2000. Section 3.1 provides a description of the signs andsymptoms displayed by the accident victims in the early stages of the accident.
Owing to the accident's occurrence in a populated area, and also owing to the
length of time until the radiation source was discovered and recovered, there wereseveral groups of people exposed. Those who obtained the source (P1–P4: Group 1)and the junkyard workers and relatives (P5–P10: Group 2) received the largestradiation doses. Some of the scrap collectors received severe localized radiationinjuries (as evidenced by the radiation burns presented); however, their whole bodydoses were around 2 Gy. The individuals at the junkyard received greater total bodyradiation doses due to their prolonged exposure to the 60Co source. Four of these
individuals (P5–P8) received doses of more than 6 Gy.8 Three of these four personsdied within two months of the accident as a consequence of their severe radiationinjuries.
Many of the victims in Groups 1 and 2 visited an outpatient clinic of Samut
Prakarn Hospital with symptoms of weakness, epilation and radiation burns, andhistories of nausea, vomiting or diarrhoea (see Table II).
The third group consists of other individuals who lived in the vicinity of the
junkyard and whose radiation doses, as estimated later, were not as significant as forthose who worked on or near the source. The fourth group includes personnel of theOAEP and others who worked in the response and recovery unit. Their whole bodyradiation doses, as described in Section 3.3, did not exceed 32 mSv for the durationof the accident response.
TABLE II. IDENTIFICATION CODES, AGE, GENDER AND EARLY CLINICALDATA OF THE ACCIDENT VICTIMS
Clinical symptoms and signs
Burns, nausea, vomiting,epilation, amputation
Burns, nausea, vomiting,epilation
Burns, nausea, vomiting, epilation
Burns, nausea, mild vomiting
Junkyard employee
Burns, nausea, vomiting,epilation, diarrhoea, epistaxis,fever; death on 18 March 2000
Junkyard employee
Nausea, vomiting, epilation,diarrhoea, fever; death on9 March 2000
Nausea, vomiting, epilation,diarrhoea
Nausea, vomiting, epilation,epistaxis; death on 24 March 2000
Nausea, vomiting, headache,
8 Doses estimated from clinical findings.
For Group 1, on the basis of an evaluation of the prodromal signs and
symptoms, significant non-homogeneous whole body irradiation occurred. Estimatesof the doses received are: P1: 2 Gy; P2: 2 Gy; P3: 2 Gy; and P4: 1 Gy.
Both P1 and P3, however, showed severe localized radiation burns. P1's burns
were confined primarily to his hands, while P3 presented burns to his hands and alsoa larger radiation burn on the posterior-lateral side of his right leg, near the knee9.
Patient P1 suffered the most severe radiation burns on both his hands, affecting allfingers and half of the palmar surfaces. The other three (P2–P4) also had seriousradiation burns: to the hands and fingers (P2), to two fingers and the right knee region(P3), and to the fingers only (P4).
Group 3 consisted of 1872 individuals who live within 100 m of the junkyard.
Various services were provided to these individuals, including checkups (862individuals, 46%), blood examinations (782 individuals, 42%), information andadvice (907 individuals, 48.5%). Of this group, 258 individuals lived within 50 m ofthe location of the source and are being followed up by the Ministry of Public Healthfor any latent effects. Within this distance of 50 m, there were five pregnant women, oneof whom decided to have an abortion. This woman had received counsel from the RoyalCollege of Radiologists in Thailand that the risk of having an abnormal baby was low.
The patients from Group 1 were first admitted and treated at Samut Prakarn
Hospital, where there was medical care available for both the haematologicaltreatment and the necessary restorative plastic surgery for their severe, yet localized,radiation injuries. The patients in Group 2 had suffered severe whole body exposureand, although some were admitted either to Samut Prakarn Hospital or to BangkokGeneral Hospital, they were subsequently transferred to Rajavithi Hospital, wherebetter facilities for their treatment were available. Rajavithi Hospital is the designatedtreatment hospital for radiological accidents in Thailand.
4.2. TREATMENT AND CLINICAL PROGRESSION OF PATIENTS
IN GROUP 1 (P1–P4)
Patient 1
P1 was admitted to Samut Prakarn Hospital with burns on his hands on
16 February 2000. Figure 14 shows hard blisters on his swollen hands with maceratedand infected skin, on 23 February 2000, day 23 after exposure.
9 Recall that P3 had been in the tricycle cart with his right leg draped over the metal
cylinder which contained the source.
FIG. 14. Hard blisters on the swollen hands and fingers of P1 on day 23, 23 February 2000.
Note the sharp demarcation lines on both the palmar and dorsal sides.
His general clinical symptoms and complete blood count were normal. His
burned hands were treated with antibiotic intravenously (Cloxacillin, 4 g/d), Trental(400 mg) and dressings. He occasionally had a low grade fever. His white blood cellcount and platelet count progressively decreased, then administration of granulocytecolony stimulating factor (G-CSF) was started (500 µg/d, which was 10 µg/kg perday) on 29 February 2000. On 2 March 2000, he was transferred to Rajavithi Hospitalwith fever, skin peeling from both hands, and low white blood cell count and plateletcount.
At Rajavithi Hospital, he was treated with a combination of G-CSF (1000 µg/d,
which was 20 µg/kg per day on 3 and 4 March, and 500 µg/d, which was 10 µg/kgper day, on 5 March 2000) and granulocyte macrophage colony stimulating factor(GM-CSF) at 300 µg/d, and other treatments he received were as at Samut PrakarnHospital. His white blood cell count and platelet count increased, and he was takenoff G-CSF and GM-CSF on 6 March 2000 (see Fig. 15).
The antibiotic was changed from Cloxacillin to Cefazolin 3 g/d because he still
had fever. After this, his fever abated.
The radiation burns experienced by P1 caused him severe pain. Dressing and
debridement of the wound areas continued. On 2 March 2000, wet desquamation wasfound on the first to fourth fingers of both hands, and a dry eschar had developed overthe distal parts of the thumbs and index fingers of both hands, the more severe escharbeing on the left index finger. After dressing with silver sulphadiazine andadministration of Cephalosporin, skin grafting was performed on his left hand on15 March 2000, using skin from his left thigh. The skin graft was mainly successful,except for his left index finger, where the graft sloughed and the flexor tendon wasexposed. He requested to be discharged from the hospital on 24 March 2000, and thiswas done, reportedly against medical advice.
He was readmitted to Rajavithi Hospital on 27 March 2000 owing to continued
pain in the area of the graft. The graft on the second and third fingers of his left handhad failed, and surgeons noted that the second finger was deeply necrotic. Figure 16shows his left hand after debridement on 28 March 2000 with the exposed flexortendon in the middle phalanx of the second finger.
Dry desquamation was noted on the wound on his right hand. An abdominal
flap on his left hand was attempted on 30 March 2000. The flap was detached on20 April 2000. An angiogram of the right forearm and hand showed normalvasculature and staining, so this was treated with physical therapy.
Patient 2
The radiation burns to P2 were less severe. He was admitted to Samut Prakarn
Hospital on 20 February 2000 with a low platelet count (from a study initiated on19 February 2000). He also had evidence of burns at the distal phalanges and palmar
G-CSF: 4 mg
29 Feb.–05 Mar.
02 Mar.–05 Mar.
Platelets 150 000–350 000
White blood cells4300–11 000
No. of blood cells per mm
FIG. 15. Haematological chart for P1 while in hospital.
FIG. 16. Condition of the left hand of P1 eight weeks after exposure. Note the exposed flexortendon in the middle phalanx of the second finger and adjacent soft tissue necrosis.
surfaces of both hands and a huge hard blister on the right hypothenar (Fig. 17),epilation and low fever.
P2 was treated with Cloxacillin antibiotic (2 g/d orally), Trental and, on 29
February 2000, G-CSF (500 µg/d) when his white blood count decreased. He wasalso treated with platelet concentrate (ten units) as his platelet count was lower than20 000/mm3.
P2 was transferred to Rajavithi Hospital on 2 March 2000 with wounds on both
hands, a wound to the hypothenar eminence of his right hand with a ruptured blister(diameter 4 cm) and a red, peeling thenar eminence on his left hand. His white bloodcell count remained low (1800), so administration of GM-CSF (300 µg/d) was begunon this date. On 3 March 2000, there were many blisters on both palms, with thelargest (approximately 5 cm × 6 cm) on the right hypothenar area.
Both G-CSF and GM-CSF were discontinued when his white blood cell count
increased. By 9 March 2000, most blisters had healed spontaneously, except for thelargest one which appeared to be a chronic wound (Fig. 18).
FIG. 17. Appearance of the hands of P2 three weeks after exposure. Note the dry desquamationof swollen fingers and both palms, with a large hard blister on the right hypothenar.
FIG. 18. Wet desquamation (rupture of huge blister) on the right hypothenar of P2 sevenweeks after exposure.
P2 was discharged from the hospital on 11 March 2000, with biweekly
appointments made for follow-up. By 7 April 2000, the wound on the right hand wasdecreasing in size and extent (diameter about 1 cm), but on 19 April 2000 at a follow-up check swelling in both hands was noted.
Patient 3
P3 was admitted to Samut Prakarn Hospital on 20 February because of a low
platelet count from a study initiated the previous day. He also demonstrated burns atthe distal phalanges of the second and third fingers of his right hand and a 30 cm longburn near his right knee. On 23 February 2000, an extended necrosis of the epidermiswas observed on the lateral side of his right thigh just above the knee, while belowknee level a 5 cm × 8 cm area demonstrated wet desquamation (Fig. 19).
P3's wounds were treated with Cloxacillin antibiotic (2 g/d orally), Trental and
G-CSF. He was also given a platelet transfusion (ten units) when his platelet count fellbelow 20 000/mm3.
On 3 March 2000, P3 was admitted to Rajavithi Hospital. Second degree burns
were seen on the index and middle fingers of his right hand, as well as a 30 cm longwet desquamation in the popliteal area of his right knee (Fig. 20).
FIG. 19. Extended necrosis and wet desquamation on the lateral side of the right leg of P323 days after exposure.
FIG. 20. Wet desquamation 30 cm long in the popliteal area of the right knee of P3 five weeksafter severe local exposure.
P3 was treated with a combination of G-CSF (250 µg/d) and GM-CSF (300 µg/d).
These were discontinued when his white blood cell and platelet counts increased.
P3 was discharged on 12 March 2000, with biweekly appointments made for
follow-up. On 17 March (seven weeks after exposure), his extended wound hadbecome infected below the knee (Fig. 21).
On 24 March 2000, he was readmitted to the hospital. His finger wound had
already healed but the (now) 28 cm × 30 cm radiation wound to his right poplitealfossa had deepened so much that it had to be debrided. A skin graft was performedon 27 March 2000 using skin from the left thigh. Although for a few days the graftappeared to have been successful, on 2 April 2000 it had to be opened. P3 wasdischarged three days later, reportedly at his own request. He returned after twoweeks when he was experiencing severe pain in his leg. The areas showed signs ofmassive infection and incipient necrosis (Fig. 22). Debridement was performed again.
Patient 4
P4 also demonstrated burns on his right second finger and left fourth finger
upon admission to Samut Prakarn Hospital. He was treated there and was transferredto Rajavithi Hospital on 3 March 2000 together with P3. Treatment at RajavithiHospital consisted of 2 g/d of Cloxacillin antibiotic, Trental and wound dressing. He
FIG. 21. Appearance of the popliteal area for P3 seven weeks after severe local radiationexposure.
FIG. 22. Massive infection and beginning of necrosis of the extended wound on the right legof P3 on 19 April 2000, 11 weeks after exposure.
was discharged on 7 March 2000 and scheduled for biweekly follow-up visits. Onfollow-up visits on 31 March and 3 May 2000, his wounds were healed. However, thenails of the second and fourth fingers of his right hand had sloughed off owing to theradiation burns to the fingers. Hypopigmentation and the absence of fingernails werenoted in a checkup on 3 May 2000.
4.3. TREATMENT AND CLINICAL PROGRESSION OF PATIENTS
IN GROUP 2 (P5–P10)
Patient 5
P5 was admitted to Samut Prakarn Hospital on 16 February 2000 with
burned and swollen hands. On 17–18 February, his white blood cell count was100 mm–3, his platelet count was in the range 40 000–50 000 and he had a highfever (Fig. 23).
The antibiotic Cefpirome was administered (2 g/d). When he was transferred to
Rajavithi Hospital on 19 February, he had already suffered alopecia, fatigue and highfever. Radiation burns "like a sunshine burn" had appeared on both hands, face andanterior chest. Antibiotic treatment and G-CSF (500 µg/d: 10 µg/kg per day) anddressing of the burn areas were continued. Fever was controlled but he had epistaxisthat needed nasal packing. His lips and tongue were severely swollen (Fig. 24).
P5's white blood cell count could not be increased and approached zero, so the
dosage of G-CSF was increased to 1000 µg/d (20 µg/kg per day). A bone marrowaspiration performed on 23 February 2000 showed severe aplasia, but a chromosomalstudy could not be completed because no metaphases were apparent. Fever returnedon 24 February 2000, when apthous ulcers were noted at the tip of his tongue. Hiswhite blood cell count was still very low, so the antibiotic was changed to 3 g/dCeftazidime plus 300 mg/d Netilmicin, together with GM-CSF (300 µg/d).
Prophylactic antifungal drugs were also administered.
His burned hands were swollen on 25 February 2000 and the skin started
peeling off by 28 February. Diarrhoea returned on 2 March and by 6 March 2000 hecould not take food orally. He still had fever and a haemoculture test was positive(Enterococci), so nutrients were provided through a nasogastric tube. Antibioticswere changed according to the results of a sensitivity test. He continued to have lowwhite blood cell and platelet counts (Fig. 23) and needed single donor platelets daily.
On 15 March 2000, tachypnea was noted and lung crepitation was detected, sobreathing was assisted by a respirator. By 17 March 2000, he had lost consciousnessand his blood pressure was dropping. P5 died on 18 March 2000, 47 days afterexposure, owing to septic shock. His heart blood culture tested positive forEnterococci.
Platelets 150 000–350 000
White blood cells 4300–11 000
No. of blood cells per mm
FIG. 23. Haematological chart for P5 while in hospital.
FIG. 24. Swollen lips and tongue of P5 on 22 February 2000, three weeks after severe wholebody exposure.
Patient 6
P6 exhibited alopecia, mucositis and swelling on both palms when admitted to
Samut Prakarn Hospital on 17 February 2000. His white blood cell count was100/mm3, so the antibiotic Cefpirome (2 g/d) was given. He was transferred toRajavithi Hospital on 19 February. He was weak and skin burn was noted on his faceand chest areas. Steroid cream was applied to the burned skin. Treatment therecontinued with the same antibiotic, together with 500 µg/d G-CSF. His fever wascontrolled but hair loss continued. A bone marrow aspiration was performed on22 February 2000, which showed severe aplasia. A chromosomal study could not becompleted because there was no metaphasic activity. On 25 February he was stillweak and a low grade fever returned. Alopecia and an ulcer developed by this dateabove his ear (Fig. 25) and an ulcer in his mouth was also noted.
P6's fever continued and the antibiotics had to be changed. An antifungal drug,
an antiviral drug and GM-CSF were added to his regimen. On 6 March 2000, he couldnot eat, so nutrients were administered through a nasogastric tube. On 7 March, hewas having difficulty breathing. A chest X ray showed right lobar pneumonia and ablood gas test showed metabolic acidosis, so a respirator was installed to helpbreathing. His blood pressure was dropping and bleeding was observed, emanating
FIG. 25. Severe alopecia and ulceration above the left ear of P6 on 22 February 2000.
from the upper gastrointestinal tract. Although he had been given Dopamine to raisehis blood pressure, supraventricular tachycardia of the type that needscardioconversion and acute renal failure were noted on 8 March 2000. On thefollowing day, 9 March 2000, a generalized clonic seizure was noted at 13:20, afterwhich his pupils were fixed dilated. Cardiopulmonary resuscitation was performedtwice on account of brachycardia but failed. P6 died at 19:38 that evening, on day 38after exposure, owing to septic shock. A heart blood culture test was positive forEnterococci.
Patient 7
P7, the owner of the junkyard, demonstrated feelings of weakness, alopecia,
anorexia and low white blood cell count when she presented herself at the outpatientclinic of Bangkok General Hospital on 17 February 2000. A bone marrow aspirationshowed pancytopenia and a biopsy showed slightly hypocellular marrow. She wastransferred to Rajavithi Hospital on 20 February 2000. Her white blood cell count waslow and her platelet count was less than 20 000, so she was treated with 500 µg/dG-CSF. Owing to excessive menstruation, she was provided with blood and platelettransfusions and hormonal therapy. Her white blood cell count fell to 100/mm3, so thedosage of G-CSF was increased to 1000 µg/d and prophylactic antibiotics
(Ciprofloxacin, 1 g/d orally) were administered. Her white blood cell count was stilllow, so GM-CSF (300 µg/d) was also given. A chromosomal study from peripheralblood was performed on 29 February 2000 but showed no metaphases. Also on thisdate she had fever with chills and looked pale. A physical examination foundsuspicions of haematoma at the rectal wall, so a septic evaluation was performed.
Packed red cell, single donor platelets and broad spectrum antibiotics (Ceftazidimeplus Netilmicin plus Metronidazole) were administered, and the dosage of GM-CSFwas increased to 600 µg/d (the upper limit), while the dosage of G-CSF was reducedto 750 µg/d. Her white blood cell and platelets slowly started recovering. Between 11and 14 March 2000, administration of G-CSF and GM-CSF was tapered off.
Antibiotics continued to be given for more than two weeks, owing to positivehaemoculture and pneumonia at the lingular segment of the left upper lung. She wasdischarged from the hospital on 28 March 2000 and biweekly appointments weremade for follow-up.
Patient 8
When P8 was admitted on 17 February 2000 to Bangkok General Hospital, he
was bleeding from his nose and had abdominal pain, diarrhoea, buccal mucositis andcheilitis. Severe aplasia was noted upon completion of a bone marrow aspiration andbiopsy that same day. His white blood cell and platelet counts were very low, soG-CSF (300 µg/d) was administered, starting on admission to hospital. On 20 February2000, antibiotics (Ceftazidime plus Amikacin) were started after a septic evaluationwas performed.
P8 was transferred to Rajavithi Hospital on 20 February demonstrating fever,
weakness, alopecia and skin burn on his face and chest. The dose of G-CSF wasincreased to 1000 µg/d and the antibiotics were continued. On 25 February 2000, apapulovesicular eruption diagnosed as Herpes zoster was spreading over his back anda fungal infection also appeared in his subaxillary region (Fig. 26).
Antiviral drugs (Zovirax, 200 mg six times per day for three days, then reduced
to 400 mg twice per day until 17 March 2000) and antifungal drugs (Sporal, 100 mgtwice per day for three days, then Ambisome 100 mg per day intravenously for twodays) were administered. The antifungal drug was administered as a prophylaxis.
Low grade fever continued and worsened to high fever ( 40°C), which continued inmid-March.
His white blood cell count could not be improved, despite the continued
administration of the G-CSF to which GM-CSF (600 µg/d) was added (intravenously).
Rusty looking sputum was noted by 18 March 2000, and chest pain developed on 19March. Ventilation was assisted on 21 March, when tachypnea was observed.
By 22 March 2000, greater tachypnea was noticed and pink frothy sputum seen,
which his physicians attributed to pulmonary oedema. He was moved to the intensive
FIG. 26. Viral infection (Herpes zoster) in the lower back (top) and fungal infection in thesubaxillary region (bottom) of P8 on day 25 after exposure.
care unit and placed on a ventilator. On 23 March 2000, additional oxygen-assistedbreathing was maintained, but he became stuporous and did not react to verbalcommands. His blood pressure dropped and both the heart rate and respiratory rateincreased. At 10:30 on 24 March 2000, P8 suffered cardiac arrest. He was pronounceddead at 10:50 (on day 52 post-exposure). His heart blood culture was positive forMorganella morganii, and a necropsy culture of his left lung was positive forStenotrophomonas maltophilia.
Patient 9
P9, who worked at the junkyard and also as a maid for P7 and P8, was seen on
19 February 2000 at Samut Prakarn Hospital after complaining of nausea, vomiting,decreased appetite and headache. She was transferred that day to Rajavithi Hospital,where alopecia and a slight fever were noted upon admission. A bone marrow aspirationand biopsy were performed on 22 February, in which severe aplasia was noted.
Complete blood examinations to note the progression of her white blood cell count wereperformed daily. The dosages of G-CSF and GM-CSF were adjusted to increase herwhite blood cell count as quickly as possible. On admission, G-CSF was administered,starting at 250 µg/d from 19 to 23 February, boosted to 500 µg/d on 24 February, andthen to 1000 µg/d from 25 February to 17 March 2000, when administration of this drugwas terminated. She was also given 300 µg/d of GM-CSF from 26 February to 5 March;this was increased to 600 µg/d from 6 to 15 March and was terminated on 16 March.
No metaphasic activity was noted in a chromosomal study performed on 29 February.
Additionally, she was given 500 mg of Ciprofloxacin twice a day from 24 February to16 March 2000 as a prophylactic antibiotic for neutropenic patients. Transient low gradefever due to an upper respiratory tract infection was also noted during her stay inhospital. She was discharged from the hospital on 25 March 2000 with biweeklyfollow-up appointments made. Also, owing to menstruation, she was given several unitsof platelets and hormonal therapy during her hospital stay.
Patient 10
P10, the mother of P7, was admitted to Samut Prakarn Hospital on 22 February
2000, having previously complained of nausea, vomiting and weakness. She also hada low white blood cell count. A slight fever was noted but the physical examinationperformed on this date was unremarkable. She was transferred to Rajavithi Hospitalon 25 February with no specific symptoms; she had been in the junkyard, however. Achromosomal study from peripheral blood performed on 29 February 2000 showed acomplex chromosomal abnormality, with ring chromosomes in some cells. Mildhypocellular marrow was noted on 1 March 2000 during a bone marrow aspiration,with lymphocytic series cells predominant. Megakaryocytes and erythroid and
myeloid series cells were slightly diminished. The doses of G-CSF and GM-CSFwere adjusted according to P10's white blood cell count each day. She was givenG-CSF at 250 µg/d from 25 February, 500 µg/d on 2 and 3 March, 1000 µg/d on4 and 5 March, 500 µg/d on 6 and 7 March, back to 1000 µg/d for 8–18 March,reduced to 500 µg/d on 19 and 20 March, and then the dose was further reducedto 250 µg/d for 21–23 March until it was terminated on 24 March. She was alsoadministered GM-CSF at 300 µg/d from 26 February through 5 March, 600 µg/dfrom 6 through 10 March, 500 µg/d from 11 through 18 March, 300 µg/d on 19 and20 March, with the termination of this treatment on 21 March. She was dischargedfrom the hospital on 28 March 2000 with biweekly appointments made for follow-up.
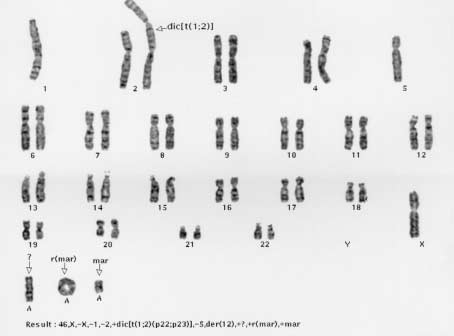
4.4. CHROMOSOMAL STUDY
A chromosomal study from bone marrow taken together with a bone marrow
smear on 22 February 2000 from P5 and P6 showed no metaphases. A bone marrowsample taken the same day from P9 showed a normal female chromosome (46, XX)with only three metaphases.
Samples of peripheral blood were drawn on 29 February 2000 from P5–P10.
The analysis showed no metaphases in the white blood cells of P5–P9. It was thusconcluded that the radiation doses these individuals had received had been sufficientto ablate leukopoiesis. On 1 March 2000, the bone marrow of P10 displayed acomplex chromosomal abnormality, presenting seven different patterns, includingring and dicentric chromosomes (Fig. 27).
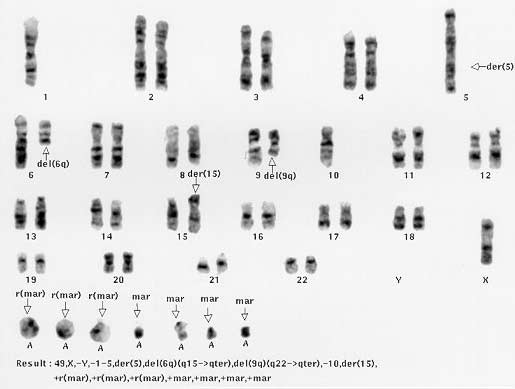
Peripheral blood samples from P2–P4 were taken on 14 March. P3 and P4
presented normal (46, XY) karyotypes, while P2 displayed eight different abnormalpatterns, including triple rings (Fig. 28). Some cells showed an unremarkablekaryotype. The varieties of the abnormalities shown in the peripheral blood, togetherwith the normal karyotypes, suggests a variation attributable to severe but localizedradiation exposure.
Despite the absence of metaphases in cultured lymphocytes from most of the
blood or marrow samples, severe chromosomal aberrations could have been detected(multiple rings, dicentrics). This could have allowed biological estimation of doses if thelaboratory had had its own in vitro calibration curve (see, for example, Refs [15, 16]).
5. FINDINGS, CONCLUSIONS AND LESSONS
TO BE LEARNED
The primary objectives of the IAEA's investigation of the accident in Samut
Prakarn were to: (a) ascertain the causes of the accident; (b) review the effectiveness
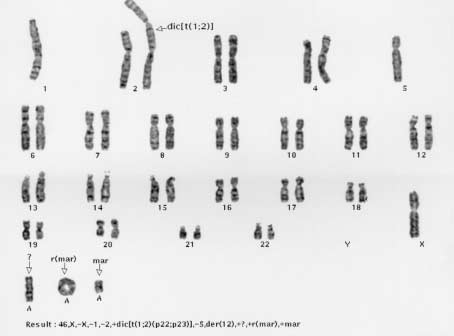
FIG. 27. Dicentric and centric ring chromosomes in the karyotype of P10 four weeks afterexposure.
of the response; (c) draw conclusions on the basis of the findings; and (d) considerthe lessons to be learned. A number of lessons are not unique to this accident butare worth reiterating in this report. The specific findings and conclusions from thisaccident are presented, together with the general lessons to be learned (in italics).
The contributory factors to the accident were as follows:
— There were difficulties in the disposition of disused radiation sources:
• there was no clear or effective end-of-life provision for the source involved;• the original manufacturer (in another country) no longer provided that
type of equipment or support for it, nor reportedly was willing to takeback the source;
• the local supplier was facing financial difficulties;• the vendor of replacement equipment was reportedly unwilling or unable
to accept the disused source.
— The national authority's workload reportedly limited its oversight of licensees.
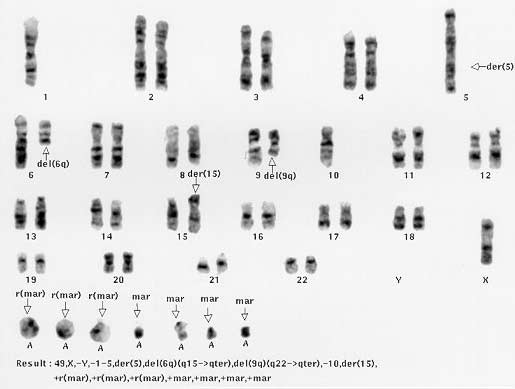
FIG. 28. Triple ring chromosomes in the karyotype of P2 six weeks after exposure.
— The licensee sold a disused source without notifying the regulatory authority of
the transfer.
— The recipient was not authorized to receive the source (or to possess the other
sources that it had).
— The recipient had relocated its radiation sources to an unsecured location.
— There were no warning signs in the local language on the source container.
— The unsecured device was disassembled and taken for sale as scrap metal.
5.1. OPERATING ORGANIZATIONS
The original licensee (a hospital) was replacing its teletherapy unit and had nosuitable space available to store the disused device. There were no provisions forreturning the disused source to the manufacturer. The hospital contracted with alocal supplier of similar equipment to handle the disused device (including thedisused source) and sold it without notifying the regulatory authority.
The local supplier company acquired and possessed radiation sources withouta valid authorization.
The local supplier company possessed radiation sources in long term storageand did not have satisfactory arrangements for prompt disposition of thedisused sources.
The local supplier company relocated its radiation sources to unsecuredstorage.
Insufficient security over the storage location allowed unauthorized access tothe radiation sources.
The BSS (Ref. [1], paras 2.34, IV.1, IV.15–IV.17) establish requirements forensuring that all radioactive sources are kept secure and require that thisfunction be the prime responsibility of the registrant or licensee as a legalperson. The BSS also require that registrants and licensees as legal personsmake a safety assessment of the protection and safety of radiation sources forwhich they are responsible (Ref. [1], paras IV.3–IV.7).
5.2. NATIONAL AUTHORITIES
The current national regulations in Thailand, although they had not been revisedor updated significantly since their promulgation, should have been sufficient tocontrol and regulate authorized legal persons, if fully implemented.
There was a lack of clear language in the regulations and licence requirementsestablishing the duties and obligations of authorized legal persons.
Regulatory authorities need to consider methods to ensure the continuity ofcontrol throughout the lifetime of a source. This may include establishinglicensing requirements for the future that take account of the disposal of thesource at the end of its useful life.
Reportedly, no clear instructions, including instructions relating to long termstorage or disposition, had been provided to the authorized legal persons, norhad there been any communication on such instructions with them.
National authorities need to review their legislative and regulatory systemsand, where necessary, make modifications to these systems in order to achievecompliance with the BSS. National authorities are encouraged to make use ofIAEA-TECDOC-1067 [2] in considering the implementation of the provisionsof the BSS. Such authorities may also find it useful to consider whether theregulatory system in their States is adequate to prevent a sequence of eventssuch as that described in this report and in other IAEA reports on radiologicalaccidents (see also Refs [3–11, 17, 18]).
At the time of the accident, the national inventory of radiation sources appearedto be incomplete.
Legal persons need to maintain accurate and current inventory records ofradiation sources, and the national authority needs to maintain records ofauthorized radiation sources under its authority [27]. While it is not at presenta requirement for a national inventory to be kept, the IAEA's Categorization ofRadiation Sources [19] provides guidance on the priorities for sources to beconsidered if such a task is undertaken.
The staffing of the national authority appears to have been insufficient to enableit to perform the necessary routine annual inspections or to follow upappropriately on the information that had come to its attention.
Routine inspections by the national authority have the potential for detectingnon-compliance with regard to the transfer and storage of radioactive sourcesand thereby preventing the precursor events to an accident [27].
The presence of a radioactive source was not detected at the junkyard, and theactions that were taken by the junkyard workers could have breached the integrityof the source or otherwise transferred the source to metal processing facilities.
National authorities need to develop strategies for detecting and dealing with‘orphan' radioactive sources. Workers such as dealers, processors andexporters of scrap metal, customs officers and border police who may beoccupationally or accidentally exposed to radioactive sources need to beprovided with suitable information and guidance (see, for example, Ref. [20]).
The sequence of events leading to this accident was similar to those describedor identified in other IAEA reports on radiological accidents. In particular, thereare significant parallels with the accident that occurred in Istanbul, Turkey, inDecember 1998–January 1999 [11]. The similarities are a cause for concernbecause the accident in Samut Prakarn could have been prevented by applyingthe lessons of the accident in Istanbul.
National authorities are encouraged to disseminate information on radiationaccidents widely to help prevent accidents of a similar nature in the future.
The Thai authorities appear to have an effective national emergency plan fordealing with radiation emergencies which involves local emergency servicessuch as the police and fire brigade.
The BSS (Ref. [1], para. V.1) presume that States will have determined inadvance the assignment of responsibilities for the management of interventionsin emergency exposure situations between the regulatory authority, nationaland local intervening organizations, and registrants and licensees. Nationalauthorities are encouraged to make use of IAEA-TECDOC-953 on Method forthe Development of Emergency Response Preparedness for Nuclear orRadiological Accidents [21] or IAEA-TECDOC-1162 on Generic Proceduresfor Assessment and Response During a Radiological Emergency [22].
Co-ordination by the Thai emergency response team in the source recoveryoperation included:
— Co-ordination with the local authority to bring the situation under control upon
recognizing the serious radiological threat to the public;
— Co-operation and co-ordination among the regulatory authorities, the local
public health office, local fire brigades and the provincial civil defence unit,resulting in the prompt availability of the requisite personnel, tools andequipment for immediate action.
A successful operation for recovery from an accident needs co-ordination withand co-operation among local authorities in the vicinity, resulting in a wellprepared and equipped rescue and recovery team.
(10) The Thai emergency response team's preparations to recover the source
— Experienced personnel with expertise in dealing with high radiation fields and
control of known contamination;
— The use of videotaping to assist in the review of the situation, training and
rehearsal for responding personnel, and planning of recovery strategies.
Emergency responders need to include personnel with diverse experience andqualifications. Modern communications media proved to be valuable and vitalto the successful recovery of the source.
(11) The Thai emergency response team used innovative means to achieve rapid
recovery of the source, which was in a difficult location. These included:
— Using fluorescent screens to pinpoint the location of the source;— Using a light bamboo rod instead of a much heavier metal pole for quick
moving and screening of scrap items;
— Utilizing a thick lead shield to reduce exposure of personnel during the
response and recovery.
Challenges need to be anticipated and prepared for in the management ofinterventions in emergency exposure situations. Preparedness and training arecrucial to the prompt abatement of a serious radiological threat, yet emergencyresponders need to maintain some flexibility and allow for innovation inresponding to challenging situations, including adapting equipment as necessary.
(12) Public concerns and misinterpretations [23–26] of the accident included the
— The Thai emergency response team was perceived as ‘not taking the matter
seriously' [23] with regard to the radiation hazard;
— The Thai emergency response team was perceived as being unprofessional and
lacking the necessary training;
— The bodies of the irradiated accident victims were perceived as being
Information needs to be given clearly and effectively for it to be understood bythe public. Adequate and effective communication with the news media can beimproved by, for example, having regular press briefings and updating themedia on the progress of events.
Lack of routine and effective public information about radiation and radioactivematerials can lead to misconception and distrust on the part of the public, whichcan lead to a situation where good scientific practice is not recognized.
(13) Representatives of the news media reportedly hampered or interfered with the
conduct of the recovery operations.
The designation of a single contact point for the news media during anemergency and recovery operations is suggested for all regulatory authorities,to allow responders to perform their functions and to prevent misunderstandingand confusion when information is obtained from several sources.
5.3. INTERNATIONAL CO-OPERATION
Thailand informed the IAEA of the accident and requested assistance as asignatory party to the Convention on Assistance in the Case of a NuclearAccident or Radiological Emergency, and the initial notification was followedby other reports.
As with this accident, the IAEA can provide assistance, upon request, toMember States in response to radiation emergencies, within the framework of
the Convention on Assistance in the Case of a Nuclear Accident or RadiologicalEmergency. It helps in preparing for the provision of assistance for the IAEA tobe informed of accidents as soon as possible.
The governments of all countries in which major radiation sources are used areencouraged to adopt the Convention on Early Notification of a NuclearAccident as well as the Convention on Assistance in the Case of a NuclearAccident or Radiological Emergency.
Preparation of this report has assisted in the recording of a comprehensiveaccount of the radiological and medical management of this radiation accidentby the national authorities.
National authorities are encouraged to share information on radiologicalaccidents with the IAEA and with other States in order to help prevent ormitigate the consequences of such accidents in the future.
The trefoil symbol on the source containers failed to convey the potentialradiation hazard. The signs and warning labels that were present were notunderstood by the individuals who gained access to these containers.
There is a need for an international review of the usefulness of the trefoilsymbol and the possible need for a more intuitively understandable warningsign for Category 1 or 2 sources. If words are used in addition to symbols, theyneed to be in a language which is understandable to the local public andworkers.
5.4. EQUIPMENT SUPPLIERS
Information about the type, size and shape of the radiation source or device wasnot readily available. The problem was compounded by the fact that a smallsource was lost in a large volume of scrap metal.
Information about the source, such as its type, activity and dimensions, wouldhave enabled response personnel to identify the source more readily for promptretrieval and recovery. Note that the IAEA, with the assistance of MemberStates, manufacturers and suppliers, is preparing a compendium of types ofradiation sources, intended to provide information concerning manufacturers,physical sizes of sources, radioactive material(s) used and activity ranges, yearof manufacture and information about their distribution.
It was possible to dismantle the teletherapy source housing readily withrelatively simple tools, which allowed individuals to be exposed to the highradiation field from the source.
Defence in depth and engineering controls designed into the construction ofshipping containers for teletherapy source housings could help to preventthe unauthorized removal of shielding and extraction of the source orexposure to it.
There was no provision for the return of the disused source to a different devicemanufacturer.
National authorities, working in co-operation with source or devicemanufacturers, need to pursue options for the safe return of spent or disusedsources to the manufacturer or to a different source or device manufacturer.
5.5. THE MEDICAL COMMUNITY
The individuals exposed in the accident in Samut Prakarn reported to hospitalsand outpatient clinics, but their original symptoms (diarrhoea, nausea andvomiting) were not initially diagnosed as being caused by radiation exposure.
Physicians need information on and training in the basic symptoms and signsof acute radiation exposure, both whole body and localized exposure, and thetypes of radiation sources that might cause such effects.
The IAEA, in co-operation with the World Health Organization, has preparedand distributed a poster and a leaflet on ‘How to Recognize and InitiallyRespond to an Accidental Radiation Injury'. These are intended to informphysicians on how to recognize a possible radiation injury from patients' signsand symptoms.
There was apparently no adequate biological dosimetry to assess the probablerange of the radiation doses received by the individuals involved.
A cytogenetic laboratory needs to be designated as the (national) biodosimetrylaboratory in a State in which radiation sources capable of causing severeradiation accidents are widely used. This laboratory needs to develop its owncalibration curves for the most common types of acute radiation overexposure,for example due to 60Co, 192Ir and 137Cs.
By means of adequate support and care, platelet transfusions and leukocytelineage stimulation (by G-CSF and GM-CSF), safe levels of blood cell countswere achieved for many of the accident victims.
The clinical evolution following this accident confirms that, even with rathersevere haematopoietic syndrome due to whole body irradiation with a dose ofseveral grays, it was not necessary to perform bone marrow transplantation.
Three individuals died of infectious complications within two months, despitethe efforts made by the specialized hospital in providing all available treatmentmodalities.
Immediate reverse isolation, coupled with the administration of antiviral,antibacterial and antifungal agents, needs to be considered if severe wholebody exposure is suspected.
FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS,INTERNATIONAL ATOMIC ENERGY AGENCY, INTERNATIONAL LABOURORGANISATION, OECD NUCLEAR ENERGY AGENCY, PAN AMERICANHEALTH ORGANIZATION, WORLD HEALTH ORGANIZATION, InternationalBasic Safety Standards for Protection against Ionizing Radiation and for the Safety ofRadiation Sources, Safety Series No. 115, IAEA, Vienna (1996).
FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS,INTERNATIONAL ATOMIC ENERGY AGENCY, OECD NUCLEAR ENERGYAGENCY, PAN AMERICAN HEALTH ORGANIZATION, WORLD HEALTHORGANIZATION, Organization and Implementation of a National RegulatoryInfrastructure Governing Protection against Ionizing Radiation and the Safety ofRadiation Sources, IAEA-TECDOC-1067, IAEA, Vienna (1999).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident in SanSalvador, IAEA, Vienna (1990).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident inSoreq, IAEA, Vienna (1993).
INTERNATIONAL ATOMIC ENERGY AGENCY, An Electron Accelerator Accident inHanoi, Viet Nam, IAEA, Vienna (1996)
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident inTammiku, IAEA, Vienna (1998).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident inGoiânia, IAEA, Vienna (1988).
INTERNATIONAL ATOMIC ENERGY AGENCY, Dosimetric and Medical Aspects ofthe Radiological Accident in Goiânia in 1987, IAEA-TECDOC-1009, IAEA, Vienna(1998).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident in Lilo,IAEA, Vienna (2000).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident inYanango, IAEA, Vienna (2000).
INTERNATIONAL ATOMIC ENERGY AGENCY, The Radiological Accident inIstanbul, IAEA, Vienna (2000).
INTERNATIONAL ATOMIC ENERGY AGENCY, Lessons Learned from Accidents inIndustrial Irradiation Facilities, IAEA, Vienna (1996).
INTERNATIONAL ATOMIC ENERGY AGENCY, Lessons Learned from Accidents inIndustrial Radiography, Safety Reports Series No. 7, IAEA, Vienna (1998).
INTERNATIONAL ATOMIC ENERGY AGENCY, Lessons Learned from AccidentalExposures in Radiotherapy, Safety Reports Series No. 17, IAEA, Vienna (2000).
INTERNATIONAL ATOMIC ENERGY AGENCY,
Biological Dosimetry:
Chromosomal Aberration Analysis for Dose Assessment, Technical Reports Series No.
260, IAEA, Vienna (1986).
INTERNATIONAL ATOMIC ENERGY AGENCY, Cytogenetic Analysis for DoseAssessment: A Manual, Technical Reports Series No. 405, IAEA, Vienna (2001).
INTERNATIONAL ATOMIC ENERGY AGENCY, Methods to Identify and LocateSpent Radiation Sources, IAEA-TECDOC-804, IAEA, Vienna (1995).
INTERNATIONAL ATOMIC ENERGY AGENCY, Handling, Conditioning andStorage of Spent Sealed Radioactive Sources, IAEA-TECDOC-1145, IAEA, Vienna(2000).
INTERNATIONAL ATOMIC ENERGY AGENCY, Categorization of RadiationSources, IAEA-TECDOC-1191, IAEA, Vienna (2000).
INSTITUTE OF SCRAP RECYCLING INDUSTRIES, Radioactivity in the ScrapRecycling Process: Recommended Practice and Procedure, ISRI, Washington, DC(1993).
INTERNATIONAL ATOMIC ENERGY AGENCY, Method for the Development ofEmergency Response Preparedness for Nuclear or Radiological Accidents, IAEA-TECDOC-953, IAEA, Vienna (1997).
INTERNATIONAL ATOMIC ENERGY AGENCY, Generic Procedures for Assessmentand Response During a Radiological Emergency, IAEA-TECDOC-1162, IAEA, Vienna(2000).
SONGPHOL KANJANACHUCHAI, "Didn't they realise the risks involved?" BangkokPost, 24 February 2000.
ANCHALEE KONGRUT, "Frightened residents force family to shift cremation site",Bangkok Post, 14 March 2000.
ANCHALEE KONGRUT, MONGKOL BANGPRAPA, "More objections to victim'scremation", Bangkok Post, 15 March 2000.
"Cobalt-60 victim laid to rest", Bangkok Post, 16 March 2000.
INTERNATIONAL ATOMIC ENERGY AGENCY, Code of Conduct on the Safety andSecurity of Radioactive Sources, IAEA/CODEOC/2001, IAEA, Vienna (2000).
CONTRIBUTORS TO DRAFTING AND REVIEW
Office of Atomic Energy for Peace, Thailand
Office of Atomic Energy for Peace, Thailand
Boonpadhanapong, T.
Rajavithi Hospital, Thailand
Chinudomsub, K.
Office of Atomic Energy for Peace, Thailand
International Atomic Energy Agency
Gerdvichai, W.
Samut Prakarn Hospital, Thailand
Jinaratana, V.
Rajavithi Hospital, Thailand
Nogueira de Oliveira, C.
International Atomic Energy Agency
Hiroshima University School of Medicine, Japan
Office of Atomic Energy for Peace, Thailand
Rerkamnuaychoke, B.
Ramathibodi Hospital, Thailand
Samut Prakarn Hospital, Thailand
Radiation Effects Research Foundation, Japan
Tanosaki, S.
National Institute of Radiological Sciences, Japan
International Atomic Energy Agency
Waniksumsombut, W.
Office of Atomic Energy for Peace, Thailand
International Atomic Energy Agency
International Atomic Energy Agency
Vienna, Austria: 11–15 December 2000
Source: http://www.physics.isu.edu/radinf/radiographer/Samut%20Prakarn%20sources.pdf
ACC/AHA/ESC Practice Guidelines ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias*—Executive Summary A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines
Hub 1 Final Report Adherence to Heart Failure Practice Guidelines in Primary and Secondary Care: A Mixed-Methods Study TECHNICAL DATA TITLE: Recap – Hub 1 Final Report EDITOR: Prof. dr. H.P. Brunner-La Rocca Drs. S. Bektas FHML, opleiding Geneeskunde Universiteit Maastricht. TEXTS: Belgium: Thomas More University College University Hospital Maastricht Maastricht University