Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Measles surveillance national guideline, ethiopia




GUIDELINE ON
MEASLES SURVEILLANCE AND
OUTBREAK MANAGEMENT
3RD EDITION

GUIDELINE ON MEASLES SURVEILLANCE AND OUTBREAK MANAGEMENT 3RD EDITION
ETHIOPIAN HEALTH AND NUTRITION RESEARCH INSTITUTE FEDERAL DEMOCRATIC REPUBLIC OF ETHIOPIA
January 2012
Addis Ababa
TABLE OF CONTENTS
ACRONYMS
Acute Flaccid Paralysis
World Health Organization, Regional Office for Africa
Attack rate among unvaccinated persons
Attack rate among vaccinated persons
Case fatality rate
Ethiopian Health and Nutrition Research Institute
Enzyme linked Immuno-Sorbent Assay
Federal Ministry of Health
Human Immune Deficiency Virus
Immunoglobulin G
Immunoglobulin M
Proportion of cases among vaccinated individuals
Public health emergency Management
Proportion of population that is vaccinated
Proportion of vaccine preventable cases
Regional reference laboratory
Supplementary immunization activities
Technical Task Force (PHEM)
United Nation Children's Fund
Vaccine effectiveness
Viral transport medium
World Health Organization
Weakly incidence rate
The Ethiopian Health and Nutrition Research Institute, which is the technical arm of the Ministry of Health of the Federal Democratic Republic of Ethiopia, would like to express its appreciation and gratitude to all those who are directly involved in or indirectly contributed to the preparation of this guideline.
EHNRI would like to thank, all the members of the vaccine preventable diseases Technical Working Group members from FMOH, EHNRI, WHO,UNCEF, and MSF for realizing the preparation of this guideline.
Special thanks go to Public Health Emergency Management (PHEM) Center members for their active involvement and leading the overall activity of the Technical Working Group and also for writing and editing the guideline.
We thank WHO for financial contribution and facilitation of the printing of this guideline.
FOREWORD
Measles is one of the communicable diseases causing preventable mortality and morbidity in the country. Epidemiological surveillance of measles is a major public health strategy in prevention and control of disease.
Based on the mandate given by the Federal Ministry of Health to prepare and distribute health and health related guidelines and standards, this guideline is prepared by Public Health Emergency Management (PHEM) Center of Ethiopian Health and Nutrition Research Institute (EHNRI) with technical support from stakeholders.
The guideline on Measles Surveillance and Outbreak Management aims to provide health authorities, medical officers, and other health personnel involved in measles control at national, regional, woreda and local levels with a step-by-step manual for setting up and carrying out measles surveillance as well as on how to detect and control epidemics of measles disease as early as possible, and to strengthen the capacity for emergency response to epidemics of measles disease manage measles outbreaks. The Africa Region as well as Ethiopia is working towards measles elimination by 2020 (as indicated in Resolution AFR/RC61/WP/1: Measles elimination by 2020: A strategy for the African Region, 61st Regional Committee meeting 2011).
To develop this third edition of the guideline, technical documents and similar guidelines prepared by WHO African Region were referenced and contextualized to our setting. Field experiences from our county are also incorporated.
EHNRI hopes that this guideline meets the needs of health workers and the different partners who are participating in measles surveillance as well as outbreak management.
Amha Kebede (PHD)
A/Director General, EHNRI
1 INTRODUCTION TO MEASLES
1.1 Background to measles control
Measles is one of the communicable diseases still causing preventable
mortality and morbidity in the country.
In 2001, countries in the World Health Organization (WHO) African Region began accelerated measles control activities to reduce measles deaths by half by 2005 compared to the estimated number of measles deaths in 1999. Implementation of the recommended strategies led to a 75% reduction in estimated measles mortality in the African Region by 2005. Following this progress, in 2006 the African Region adopted a goal to achieve 90% measles mortality reduction by 2010 compared with the estimate for 2000. By 2008 in the African Region, reported measles cases decreased 93% and estimated measles mortality decreased 92% compared with 2000.The strategies include improving routine vaccination coverage, providing a second opportunity for measles vaccination through supplementary immunization activities (SIAs), improving measles-case management, and establishing case-based measles surveillance. Since 2002, Ethiopia adopted these regional goals and strategies and has been taking important steps to control measles. The Africa Region as well as Ethiopia is working towards measles elimination by 2020 (as indicated in Resolution AFR/RC61/WP/1: Measles elimination by 2020: A strategy for the African Region, 61st Regional Committee meeting 2011).
The National Immunization Programme was established in the 1980s, and currently delivers service through static and outreach sites nationwide. The current routine immunization schedules recommend a dose of measles vaccination at 9 months of age. The WHO UNICEF coverage estimates for measles vaccination for Ethiopia also indicate an increase from 37% in 2000 to around 80% in 2010.
1.2 Mode of transmission
Measles is an acute, highly contagious viral disease caused by measles virus.
This highly contagious virus is transmitted primarily by respiratory droplets or
airborne spray to mucous membranes in the upper respiratory tract or the
conjunctiva. Common source outbreaks associated with airborne transmission of measles virus have been documented.
The measles virus is a member of the genus Morbillivirus of the Paramyxoviridae family. The virus appears to be antigenically stable—there is no evidence that the viral antigens have significantly changed over time. However, sequence analysis of viral genes has shown that there are distinct lineages (genotypes) of wild-type measles viruses. When considered along with epidemiological information, identification of a specific virus genotype can suggest the origin of an outbreak. The measles virus is sensitive to ultraviolet light, heat, and drying. The virus has a short survival time (<2 hours) in air or on objects and surfaces.
Humans are the only natural hosts of measles virus. Although monkeys may become infected, transmission among them in the wild does not appear to be a mechanism by which the virus persists in nature.
The risk factors for measles virus infection include: infants who lose passive antibody before the age of routine immunization, children with vitamin A deficiency and immunodeficiency due to HIV or AIDS, leukemia, alkylating agents, or corticosteroid therapy, regardless of immunization status and children who travel to areas where measles is endemic or contact with travelers to endemic areas. Malnourished and young children are at higher risk of developing complications and mortality from measles infection.
1.3 Clinical features of measles
1.3.1 Pathogenesis
Measles is a systemic infection. The primary site of infection is the respiratory
epithelium of the nasopharynx. Two to three days after invasion and
replication in the respiratory epithelium and regional lymph nodes, a primary
viremia occurs with subsequent infection of the reticuloendothelial system.
Following further viral replication in regional and distal reticuloendothelial
sites, there is a second viremia, which occurs 5 to 7 days after infection.
During this viremia, there may be infection of the respiratory tract and other
organs. Measles virus is shed from the nasopharynx beginning with the
prodrome until 3 to 4 days after rash onset.
1.3.2 Incubation period and period of infectivity
The incubation period is approximately 10–12 days from exposure to the
onset of fever and other nonspecific symptoms and 14 days (with a range of
7–18 days),from exposure to the onset of rash.
Measles can be transmitted from four days before rash onset (i.e., one to two days before fever onset) to four days after rash onset. Infectivity is greatest three days before rash onset. Measles is highly contagious. Secondary attack rates among susceptible household contacts have been reported to be 75%–90%. Due to the high transmission efficiency of measles, outbreaks have been reported in populations where only 3% to 7% of the individuals were susceptible. Whereas vaccination can result in respiratory excretion of the attenuated measles virus, person-to-person transmission has never been shown.
Prior to the availability of measles vaccine, measles infection was virtually universal. Infants born to mothers who have either had measles or been vaccinated are protected by trans-placental transferred antibody and Infants are generally protected until 5 to 9 months of age, this is passive immunity. Immunity following natural infection is believed to be life-long. Persons who have taken measles vaccine and have formed antibodies in response to the vaccine are also immune.
1.3.3 Symptoms and signs
Prodrome and general symptoms: measles infection presents with a two to
four day prodrome of fever, malaise, cough, and runny nose (coryza) prior to
rash onset. Conjunctivitis and bronchitis are commonly present. Although
there is no rash at disease onset, the patient is shedding virus and is highly
contagious. A harsh, non-productive cough is present throughout the febrile
period, persists for one to two weeks in uncomplicated cases, and is often the
last symptom to disappear. Generalized lymphadenopathy commonly occurs
in young children. Older children may complain of photophobia and,
occasionally, of arthralgia.
Koplik's spots may be seen on the buccal mucosa in over 80% of cases, if careful daily examinations are performed before rash onset. The lesions
appear one to two days before rash onset and persist for two or three days before disappearing soon after rash onset. Rash appear two to four days after the prodrome symptoms begin, a characteristic rash made up of large, blotchy red areas initially appears behind the ears and on the face. At the same time a high fever develops. The rash peaks in two to three days and becomes most concentrated on the trunk and upper extremities. The density of the rash can vary. The rash typically lasts from three to seven days and then fades in the same pattern as it appeared and may be followed by a fine desquamation. Whereas rash may be less evident in children with dark skin, desquamation generally is apparent. Some children develop severe exfoliation, especially if they are malnourished.
(7 to 18 days before rash)
(About 4 to 8 days)
-18 -17 -16 -15 -14 -13 -12 -11 -10 -9
Infectious Period
probable start of
Figure 1.The clinical course of measles and its relation to exposure and infectious period for active case
finding
1.3.4 Differential diagnosis
Laboratory support is essential for definitive diagnosis, especially during
periods of low measles incidence. Many illnesses are accompanied by fever,
rash, and a variety of non-specific symptoms. In examining for measles, it is
important to consider rubella, scarlet fever, exanthema subitum (roseola),
dengue fever, and the early stages of chickenpox in the differential diagnosis.
Moreover, there are other conditions that may present in a similar form,
including erythema infectiosum (fifth disease), enterovirus or adenovirus
infections, toxic shock syndrome, rickettsial diseases, and drug
hypersensitivity reactions. Modified forms of measles, with generally mild
symptoms, may occur in infants who still have partial protection from
maternal antibody, and occasionally in persons who only received partial protection from the vaccine.
1.3.5 Complications
Many children experience uncomplicated measles. However, in about a third
of the cases, measles is followed by at least one complication caused by
disruption of epithelial surfaces and immunosuppression. These include
pneumonia, ear and sinus infections, mouth ulcers, persistent diarrhea, and
upper airway obstruction from croup (laryngo-tracheo-bronchitis). Less
common complications include corneal drying that could progress to
ulceration (keratomalacia) and blindness, protein energy malnutrition,
convulsions and brain damage. Complications are more common in young
children below 5 years of age and complication rates are increased in persons
with immune deficiency disorders, malnutrition, vitamin A deficiency, and
inadequate vaccination. Immuno-compromised children and adults are at
increased risk for severe infections and super infections. Unless managed
early and aggressively, these complications may lead to death within the first
month after the onset of rash. The case fatality from measles is estimated to
be 3 – 5% in developing countries but may reach more than 10% in outbreaks
especially when it is compounded by malnutrition.
1.3.6 Case fatality
In Ethiopia, the expected case-fatality rate is between 3% and 6%; the highest
case-fatality rate occurs in infants 6 to 11 months of age, with malnourished
infants at greatest risk. These rates may underestimate the true lethality of
measles because of incomplete reporting of outcomes of measles illness. In
certain high-risk populations, case-fatality rates as high as 30% have been
reported in infants aged less than 1 year of age.
Malnutrition (including vitamin A deficiency), underlying immunodeficiency and lack of access to medical care are all factors leading to the high case-fatality rates observed in many parts of the world.
2 ACCELERATED MEASLES CONTROL STRATEGIES
In 2001, countries in the World Health Organization (WHO) African Region began accelerated measles control activities to reduce measles deaths by half by 2005 compared to the estimated number of measles deaths in 1999. Implementation of the recommended strategies led to a 75% reduction in estimated measles mortality in the African Region by 2005. Following this progress, in 2006 the African Region adopted a goal to achieve 90% measles mortality reduction by 2010 compared with the estimate for 2000. By 2008 in the African Region, reported measles cases decreased 93% and estimated measles mortality decreased 92% compared with 2000.Since 2002, Ethiopia adopted these regional goals and strategies and has been taking important steps to control and ultimately to eliminate measles by 2020.
Strategies for sustained measles morbidity and mortality reduction:
• Routine immunization of > 90% of children aged 9 to 11 months; • Provide a second opportunity for measles vaccination; • Case-based measles surveillance; • Improved case management including provision of vitamin A.
Periodic measles outbreaks occur when a large number of susceptible accumulate in a community. Susceptible accumulate through time even in the setting of high routine measles vaccination coverage.
2.1 Routine immunization
Measles vaccination is one of the most cost-effective interventions available.
Since measles vaccine was developed in 1958, it has saved the lives of
millions of children throughout the world. Measles vaccine is made from a
live attenuated virus. When children are correctly administered 0.5 ml of
potent live attenuated measles vaccine subcutaneously, serologic studies
have demonstrated that measles vaccines induce sero-conversion of 85% at 9
months and above 95% after 12 months of age. The peak antibody response
occurs 6 to 8 weeks after infection or vaccination. Immunity conferred by
vaccination against measles has been shown to persist for at least 20 years
and is generally thought to be life-long for most individuals.
The National Immunization Programme in Ethiopia was established in the 1980s, and currently delivers service through static and outreach sites nationwide. The current routine immunization schedule recommends measles vaccination at 9 months of age. The WHO/UNICEF coverage estimates for measles vaccination in Ethiopia indicate an increase from 37 % in 2000 to 82% in 2010.
Efforts should be made to strengthen routine immunization with the target of reaching more than 90% of infants 9 to 11 months of age with measles vaccine. Increasing and sustaining measles routine coverage over 90% is essential for achieving a sustainable reduction in measles mortality and achieving the 2012 pre-elimination goal set by WHO/AFRO. Activities to improve routine immunization coverage include:
Planning and implementation of regular immunization sessions at fixed and outreach immunization sites.
Regular analysis of routine immunization data and taking corrective action to ensure a sustained increase in the coverage of measles vaccination, concentrating on the communities / children not vaccinated.
Special strategies for reaching the un-reached.
Reduction of missed opportunities and dropout rates.
Training to improve management of immunization services at all levels.
Improving supportive supervision.
Design and implementation of information education and communication activities and materials.
2.1.1 Vaccine storage
The current Federal Ministry of Health guidelines recommend measles
vaccine to be stored at minus 20oC at the national store and between 2oC to
8oC at health facility level. Reconstituted measles vaccine should be kept cool
and protected from direct sunlight and discarded after 6 hours, or at the end
of the immunization session, whichever comes first.
2.1.2 Contraindication of the vaccine
Measles vaccine can be safely and effectively administered to children with
mild acute illnesses, such as low fever, diarrhea, and upper respiratory tract
infections. However, severely ill children with high fever should not be
vaccinated until they have recovered.
2.1.3 Adverse events following immunization
Approximately 5% to 15% of infants vaccinated with measles vaccines may
develop a low-grade fever beginning 7–12 days after vaccination and lasting
for one to two days; approximately 5% develop a generalized rash beginning
7–10 days after vaccination and lasting for one to three days. These reactions
are generally mild and well tolerated. Neurological complications following
vaccination are reported to occur in less than 1 in 1 million vaccinations. The
benefit of using the vaccine clearly outweighs the costs associated with
having the disease, both in human and monetary terms. Vaccine used after 6
hours of reconstitution may result in toxic shock syndrome and death.
2.2 Second opportunity for vaccination
A second opportunity for vaccination is giving the chance for immunization of
measles for the second time to children who may not have got the vaccine or
failed to develop protection. Those who are not immune to measles could be
identified only by testing measles specific IgG antibody levels; however since
tests to detect antibody levels are much more expensive than measles
vaccine and measles vaccine is a very safe vaccine, immunization activities to
provide second opportunity should be given to all people in the targeted age
group.
The sero-conversion rate of measles vaccine at 9 month of age is85%, accordingly, even in regions where routine immunization coverage is high, some children from each birth cohort remain susceptible to measles. When large numbers of susceptible children accumulate over time, periodic outbreaks may occur in well vaccinated woredas. The second opportunity for measles immunization is required to protect those children who have never been vaccinated and those who were vaccinated but did not develop the immunity. The second opportunity can be provided through supplementary immunization activities (SIA) or through routine immunization.
As Ethiopia has not reached over 90% coverage on the first dose of measles, it is not recommended to start a routine second dose. Therefore the country is using the option of SIAs and has conducted a catch-up and several follow-up campaigns to increase measles immunity. When Ethiopia achieves over 90% routine measles vaccination coverage for 3 consecutive years, a second routine dose may be considered as an alternative to periodic campaigns.
2.3 Case-based measles surveillance
One of the four important strategies to quickly identify cases and respond to
suspect outbreaks involves case-based measles surveillance. In this system,
each case is reported using an individual case-report form, and a blood
specimen is obtained to test for measles immunoglobulin M (IgM). Measles
case-based surveillance data is collected using the standard case based
investigation form (sPHEM Case based Reporting form).
Measles case-based surveillance is part of the national PHEM system and a key component of the measles control program. It is a system whereby every suspected measles case should be detected, reported and undergo laboratory investigation (or the first five cases in the case of outbreaks).
Measles is an immediately reportable disease under the national PHEM system. The case should be investigated with serum specimen collection at first contact with the health worker, but within 28 days of rash onset.
The primary objectives of measles surveillance are to:
Detect continuing measles transmission in an area;
Identify, investigate, and manage outbreaks;
Predict outbreaks by identifying geographic areas and age groups at high-risk; and
Evaluate vaccination strategies in order to improve measles control.
2.3.1 Measles standard case definitions
The surveillance system must be sensitive enough to identify circulating measles virus in the community. Use of the standard case definition for
suspected measles cases is the primary tool in the surveillance system to ensure early detection of any suspected cases.
Measles suspected cases at community level: A community member should
report any person with rash and fever to a health worker and also advise the
person to go to a health facility.
Suspected measles case: Any person with fever and maculopapular (non-
vesicular) generalized rash and cough, coryza or conjunctivitis (red eyes) OR
any person in whom a clinician suspects measles.
CORYZA (RUNNY NOSE) CONJUNCTIVITIS
Confirmed measles case: A suspected case with laboratory confirmation
(positive IgM antibody) or epidemiologically linked to confirmed cases in an
outbreak.
Epidemiologically linked case: A suspected measles case that has not
had a specimen taken for serologic confirmation and is linked (in
place, person and time) to a laboratory confirmed case; i.e., living in
the same or in an adjacent district with a laboratory confirmed case
where there is a likelihood of transmission; onset of rash of the two
cases being within 30 days of each other.
When a cluster of three or more cases from a woreda or health-facility
catchment area (potentially including the neighboring woreda) is laboratory
confirmed, subsequent cases from that woreda, occurring within 30 days are
considered confirmed by epidemiological linkage, and further blood sample
collection is not required. However, all cases should be line listed with the
prepared format and submitted to the next level and stored in the database.
Measles death: For surveillance purposes, a measles death is defined as any
death from an illness that occurs in a confirmed case or epidemiologically
linked case of measles within one month of the onset of rash. The immediate and delayed complications of measles (like pneumonia, persistent diarrhea) may manifest and lead to death much later after the disappearance of the rash. Measles deaths are usually under-reported.
It is important to ask about recent fever rash illnesses to all children being brought to health facilities with pneumonia and diarrhea to ensure appropriate case management. Equally it is important to encourage caretakers of measles to return for follow-up treatment should complications occur.
2.3.2 Reporting, analyzing, and interpreting data
Surveillance data should be analyzed on a weekly basis at each level (i.e.
health facility, woreda, zone, region and national).
Surveillance data analysis is essential to:
Describe the characteristics of measles cases in order to understand the reasons for the occurrence of the disease and develop appropriate control measures;
Predict potential outbreaks and implementing vaccination strategies in order to prevent outbreaks;
Detect and investigate outbreaks timely to ensure proper case management, and determine why outbreaks have occurred (e.g. failure to vaccinate, vaccine failure, accumulation of susceptible persons).
Monitor progress towards achieving disease control and elimination goals;
Using the routine surveillance data, conduct detailed analysis looking into all cases of measles that are confirmed by laboratory or by epidemiological linkage, or are clinically compatible by person, place and time and look for trends and unusual changes.
The minimum expected data handling and analysis includes:
Monitoring of the timeliness and completeness of surveillance reporting at all levels;
Monitoring main and supplementary surveillance performance indicators at zone, regional and national level;
Following the trends of measles using the basic epidemiological dimensions:
o Time: What are the dates of rash onset among cases? Allows the
creation of the epi-curve.
o Person: What are the characteristics of the cases (e.g. age, sex,
vaccination status)?
o Place: Where do cases live? Where are the most affected
areas/localities? Allows the mapping of the geographical extent of the outbreak (e.g. spot map or table with attack rates by district).
Data completeness
Every week start data analysis by assessing the data completeness using the
following formula:
Health facilities in your area are all the institutions that are required to
report to you i.e. hospitals, health center and health posts. In order to get a
correct epidemiological meaning completeness should be 80% or above.
Pattern of disease
Weekly and monthly tabulation of reported suspected cases using the
measles specific person analysis table; analysis of age group, vaccination
status, outcome (alive/dead), IgM results of measles cases and deaths should
be made at health facility woreda, zonal, regional and national levels. This
helps to determine what populations are at risk for the disease according to
their host characteristics (age, sex) or exposures (vaccination status,
residence, etc.). Such an analysis is also used to estimate an attack rate (by
age grouping, by geographic area) and the case fatality rate (as a measure of
the quality of case management).
Spot Map
A spot map showing those
cases
laboratory-confirmed and epidemiologically
according to their place of residence to be compared with vaccination coverage data
reporting sites. If the size of the population varies between the areas you are comparing, a spot map (which shows numbers of cases) can be misleading. In such an instance, area-specific attack rates with an area shade map helps
Figure 2.spot map showing Measles Cases Distributions in line
to better understand the with measles vaccination coverage
situation.
Epi-curve
A measles epi-curve shows the number of cases by the date of rash onset. In
routine surveillance, an epi-curve depicts the occurrence of cases by using a
histogram of the number of cases by their week of onset. This curve provides
a simple visual display of the intensity of cases over time, highlighting the
burden of disease (including identification of an outbreak) and seasonality. In
outbreaks, an epi-curve is also used, usually using the day of rash onset to
describe the evolution of the disease in a defined geographical area.
Case Fatality Rate (CFR)
The case fatality rate is the proportion of cases resulting in death. To find the
case fatality rate, divide the number of deaths by the number of cases, and
multiply by 100.CFR can be calculated on weekly, monthly or yearly basis.
CFRs should be estimated by age-group, if possible.
Note: The total number of cases is equal to total cases alive plus total deaths.
Attack Rate (AR)
Attack rate is an incidence rate (for measles usually expressed as a percent),
used predominately when the population is exposed to an increased measles
risk for a limited period of time, such as during an outbreak. It relates the
number of measles cases in the population at risk and reflects the extent of
outbreak. An attack rate is calculated as follows:
Age-specific Attack Rate (ASAR)
If age-specific data are available for the area of the outbreak, age-specific
attack rates can also be calculated as follows:
Note: The most at risk population are children under the age of 5 years. The
ASAR0-4 can be calculated using the estimated proportion of the total
population under-five and subsequently compared to the risk for the whole
population (crude AR). This will highlight the level of risk in under-fives
compared to the total population. Age-specific attack rates also allow
comparisons of measles in age groups with different population sizes (0-<5
years vs. 5-<15y)
Weekly Incidence Rate (WIR)
A weekly incidence rate shows the rate at which new cases occur within a
given period of time (usually one week). WIR can be expressed per hundred
persons (percentage) or per 1,000 persons.
2.3.3 Laboratory investigation
During the first contact made by a health worker with the suspected case, the
health worker must make every effort to obtain the basic information,
epidemiologic and clinical data, and a blood sample.
Internationally there are four recommended techniques for collecting specimens from suspected measles cases. In Ethiopia, currently blood sample (serum specimen) and nasopharyngeal swab samples are the two sample types collected. A blood sample is for measles-specific IgM detection and a nasopharyngeal swab sample is collected for virus isolation in order to identify the genotype of the measles virus in a particular outbreak. WHO recommends the IgM indirect ELISA method for rapid confirmation of measles cases. The test can be run in one day so that results can be returned in a timely manner. The laboratory result has to be sent to the users to the maximum within 7 days.
Filter paper method dried blood sample is another method used to test for the presence of measles-specific IgM; and sample of patient urine is used to do virus isolation for genotyping. This method is not currently used in Ethiopia.
A small proportion of samples may give indeterminate results on IgM testing. All measles laboratories are expected to re-test measles IgM indeterminate samples, and to perform rubella IgM testing on all measles IgM indeterminate and IgM negative specimens.
Blood sample collection
While IgM ELISA tests are more sensitive between days 4 and 28 days after
the onset of rash, a single serum sample obtained at the first contact with the
health care system within 28 days after onset is considered adequate for
measles surveillance. The measles specific IgM antibody starts to increase in
the serum with the appearance of rash and can be detected in good titer for
the first 28 days following rash onset while IgG should persist throughout the
life of the previously infected person.
Measles IgM antibodies are markers of recent infection or vaccination. As both infection and vaccination stimulate an IgM response, the child's
vaccination history is important in the interpretation of the test result. Any person with measles IgM positive results who has had history of measles vaccination in the 30 days preceding the collection of the serum sample is not considered to be a laboratory confirmed case of natural measles infection, but IgM positive due to vaccination.
Procedure for Specimen Collection
Collect 5 ml blood by veni puncture into a sterile tube labeled with patient
identification and collection date. To separate the serum from red cells, one
of the following three methods described below can be employed. To prevent
bacterial over-growth, ensure that the serum is poured into a clean glass test
tube. The test tube does not need to be sterile, just clean.
If a centrifuge is available:
o Let the blood sit for 30-60 minutes, then centrifuge the specimen
at 2000 revolutions per minute (rpm) for 10-20 minutes and pour off the serum into a clean tube.
If no centrifuge is available:
o Let the blood sit at an angle for at least 60 minutes (without
shaking or being driven in a vehicle), then pour off the serum into a clean glass tube.
o If a refrigerator is available, put the sample in a refrigerator for
4-6 hours until the clot retracts, then pour off the serum the next
morning. Do not freeze the whole blood.
Label the serum test tube, and the label should contain patient identification (name, address), date of specimen collection.
If there are more cases collect sample in a similar way for at least 5 of them and separate the serum, put the serum in separate, labeled test tubes.
Storage and transportation of the specimen
To transport the specimen keep the serum specimen in a vaccine carrier at 4 -
8°C to prevent bacterial over-growth. If multiple samples, put each test tube
in a separate plastic bag and keep them in the same vaccine carrier which has four conditioned ice packs in four of its sides.
The specimen and a copy of the completed case investigation form should arrive at the nearest designated regional or national measles laboratory within three days of collection. A case investigation reporting form should be kept in the same vaccine carrier with different plastic bag. (Currently IgM testing is being done only at EHNRI measles laboratory, but it is planned to expand it to regional laboratories.)
Before transport of serum samples to the national measles laboratory make sure that:
The case investigation form is complete and approved by nearby health institution, woreda health office or zonal health department (four copies).
Obtain approval or support letter from the concerned health facility, woreda health office, or zonal health office.
The health professional transporting the sample should have an identification card.
An adequate blood sample is a sample collected in the first 28 days following
the onset of rash (upon first contact with a suspected measles case) and in
good condition.
Adequate volume for serologic testing (at least 2ml);
Not turbid from possible contamination;
Not desiccated upon arrival at the laboratory; and
Transported in a vaccine carrier (with ice packs) at 2°C to 8°C.
Serum from
suspected measles
Measles IgM test
Positive
Negative
Confirm measles
Rubella IgM test
positive
Positive
Negative
Confirm rubella
positive
Figure 3.Laboratory testing of serum specimen (collected <28 days)
Nasopharyngeal sample collection
Nasopharyngeal or throat swabs are collected during measles outbreak to
identify the measles genotype. The swab samples should be collected within
the first five days after the onset of rash from the first five cases
encountered. The purpose of nasopharyngeal sample collection is for
isolation of measles virus from the specimens to genetically sequence the
measles virus responsible for the outbreak. Analysis of viral nucleotide
sequences allows classification of measles isolates according to probable
geographic origin.
Procedure
Nasopharyngeal swabs are obtained by applying a prepared swab to the
nasopharynx and firmly rubbing the nasopharyngeal passage and throat with
sterile cotton swabs to dislodge epithelial cells. The swabs are then placed in
sterile viral transport medium (VTM) in labeled screw capped tubes, (you may
need to break the tip of the swab handle to fit the VTM tube).The VTM can be
obtained from the National Measles Laboratory at EHNRI.
Storage and transportation of the specimen
Nasopharyngeal swabs are prepared with transport tubes containing viral
transport media. The specimens should be refrigerated and transported to
the National Measles Laboratory using conditioned ice packs (2 to 80C) within
48 hours of specimen collection. If arrangements cannot be made for rapid
shipment, swabs should be shaken in the medium. Note that the case
investigation form should be completed for the cases from which
nasopharyngeal swabs are collected.
Dried blood sample using filter paper techniques
This sample collection method is not yet in practice in Ethiopia. The samples
collected through this method are used for IgM testing. Like serum samples
this should also be collected any time between the first and 28 days after the
onset of rash. The dried blood sample using a filter paper method is as
effective as the venous blood in terms of sensitivity. It is also more
convenient for specimen collection and transportation.
Label the filter paper with the necessary information for identification
For finger prick, the hand should be warm and relaxed. The patient's fingers should be straight but not tense. Clean the puncture site with an alcohol swap and allow the site to dry.
Use a clean gloved thumb to press lightly against the palmar surface of the finger moving from the top of the knuckle to the tip of the finger. With the thumb's gentle pressure at the tip of the finger, place the lancet at the side of the fingertip.
Press the lancet firmly against the finger or heel and allow the tip to penetrate the skin by 2 mm.
Dispose of the used lancet into a sharps container.
Wipe away the first drop of blood with a clean piece of dry gauze.
Allow one drop to fall onto each circle of the filter paper. Fill at least three circles and four if possible. Ensure that the blood soaks completely through the paper covering the complete area of the circle.
Do not hold the filter paper against the puncture site.
Storage and transportation of the specimen
Allow the filter paper to dry thoroughly (at least 15-20 minutes) before
enclosing in a bag or storing. Drying stabilizes the IgM and reduces the chance
of microbiological contamination.
Wrap each dried blotting paper in paper foil, or plastic to prevent possible cross contamination.
Store each filter paper out of the sunlight and preferably inside a plastic bag to protect it from dust and moisture.
Store if possible in a cool place and transport to the laboratory as quickly as possible under reverse cold chain.
Urine for virus isolation
Urine sample collection method is also not yet in practice in Ethiopia.
Samples may be collected from 5 cases of an outbreak within 5 days of onset
of rash. Ten to fifty milliliters of urine is adequate. First passed morning
specimens are preferable.
Mid-stream urine sample should be collected in sterile urine bottles.
Label the container with name, address, and date of collection
Complete the case investigation form
Storage and transportation of the specimen
Urine sample should be kept at 4 to 80C before shipment;
If centrifuge is available, centrifuge at 500g (approximately 1500 rpm) for 5 minutes;
Supernatant should be discarded and sediment re-suspended in 1ml of virus transport medium;
Do not freeze the sediment if it can be shipped within 48 hours;
Urine should not be frozen before centrifugation and separation of cells;
Place the urine bottles in zip lock bags and secure (use separate bags for individual samples);
Place the plastic bags in the vaccine carrier with ice pack;
Transport the urine sample at the earliest (within 24 hrs);
Follow the same procedure that is followed for shipping blood.
2.3.4 Measles case classification
Upon investigation, all suspected measles cases should be classified into one
of the three mutually exclusive categories, i.e., laboratory confirmed cases,
epidemiologically confirmed (linked) cases, or compatible. Measles IgM
antibody negative cases are classified as discarded cases.
Laboratory-confirmed case is a suspected case which has laboratory results
indicating infection (measles IgM positive or isolation of a measles virus).
Epidemiologically-linked case is a suspected case, which has contact with
laboratory confirmed case or another epidemiologically-confirmed case.
Compatible case is a suspected case which has not been adequately
investigated.
Discarded case is a suspected case which, upon adequate investigation that
includes a blood specimen collected in the appropriate time frame, lacks
serologic evidence of a measles virus infection.
IgM negative
Adequate blood
Laboratory
IgM positive
confirmed
Clinical /
compatible
(if repeat remains
Suspected
measles case
Confirmed by
laboratory
No adequate
confirmed IgM
blood specimen
positive case
(or no blood
Clinical /
compatible
laboratory
Figure 4.Measles case classification flow chart
2.4 Measles case management and contact tracing
2.4.1 First contact with cases
The activities at the first contact should occur as follows:
1. As soon as a healthcare worker suspects measles infection, the
patient or his/her parents should be informed and convinced to give information about the patient and provide informed consent for taking of blood specimen
2. Immediately notify and take case investigation forms and fill it
accurately and completely.
3. Get specimen collection kits to take blood for laboratory investigation
take blood specimen or find someone who can draw blood specimen from the patient and collect blood sample.
4. Ask about additional suspected cases in the home, adjacent homes,
or in the neighborhood. Remember that some cases may be in either the incubation period or early stages of the illness.
5. It is important that the families know whom to contact if a rash
should occur. In addition, a visit/call should be made after a few days to ask if any new suspected cases have occurred in the household.
6. All families should be advised to keep the patient at home and to
allow only indispensable visitors until the rash disappears to minimize the number of people exposed to infection.
7. Ask the family if they know when/where the patient got the illness. It
will be necessary to explain the incubation period to them, and that after exposure occurs it takes about 7-18 days for symptoms to start. It may be necessary to remind them that they have been exposed to someone who did not have a rash, as measles is highly contagious before the rash appears.
8. Visit adjacent homes (for example, within a radius of 300 to 500
meters around the case or in the same block or village and ask, in person, whether any case of fever and rash has occurred during the previous month.
9. Investigate any reports of rash illness. It may be necessary to visit
clinics, homes, or other possible places of exposure to see if there has been a rash illness and to fully investigate the case.
10. Preschools, nurseries, schools, church groups, etc., in the area should
be visited to find out if any fever and rash illnesses have been occurring.
11. Send pamphlets and/or verbally notify the neighborhood, preschools
and schools, and local leaders that there is a suspected case in the area, and that anyone aged between 9 months and 1 year who has not been vaccinated needs to be vaccinated as soon as possible.
2.4.2 Clinical assessment
To ensure that cases with severe complications is properly treated,
Ask if the person has had:
A change in the level of consciousness, feeding or drinking;
Cough, convulsions, diarrhea, ear pain;
Discharge from eyes or loss of vision.
Examine the person for:
Rapid pulse, wasting, sore red mouth;
Dehydration (thirst, sunken eyes, skin pinch goes back slowly);
Pneumonia (rapid breathing, chest in drawing);
Ear infection (draining pus, red/immobile eardrum);
Eye disease (pus; corneal ulcer, perforation, clouding).
Classify the severity of the measles case:
Uncomplicated measles: a person with none of the signs or
symptoms of complicated disease.
Complicated measles: a person with measles and at least one of the
sign or symptom of complicated disease listed below.
tracheobronchitis, otitis media, malnutrition, corneal ulceration and blindness (due to vitamin A deficiency), stomatitis, acute encephalitis
o Long-term complications: increased susceptibility to other
infections, blindness, or sub-acute sclerosing pan encephalitis.
2.4.3 Treating uncomplicated measles
Generally vitamin A should be given to all measles cases, irrespective of whether it has previously been administered for prophylaxis or given during routine immunization activities. There is no specific anti-viral drug against measles. Therefore, manage all cases symptomatically with supportive measures.
Provide 2 doses of Vitamin A over 2 days as indicated in elow.
Table 1.Recommended vitamin A doses and schedule for treatment of measles cases
Age in Months
Dose to be Given
(Immediately on Diagnosis)
Control fever by keeping the child cool and giving antipyretics, as required.
Advise mothers to treat the child at home as long as no complications develop. Discourage visitors.
Advice mothers to provide nutritional support: continue breast feeding or give weaning foods and fluids at frequent intervals and treat mouth ulcers.
Instruct mothers to return for further treatment if the child's general condition worsens or any of the danger signs develop and explain to mothers that there is an increased risk of diarrhea, acute respiratory infections and other infections in the weeks following measles and encourage them to seek medical advice early.
2.4.4 Treating complicated measles
Refer and/or hospitalize case for further management according to Integrated Community Case Management (ICCM) or Integrated Management of Neonatal and Childhood Illness (IMNCI) protocols.
Follow the above recommendations for case management of uncomplicated measles, ensure 2 doses of vitamin A are given.
Vitamin A administration is particularly important to minimize the risk
of potentially blinding eye lesions: in this situation, a third dose of
vitamin a should be given 2-4 weeks after the second dose using the
same dosage and age as in
Clean eye lesions and treat with tetracycline eye ointment (for corneal lesions, cover the eye with a patch).
Clean ear discharge and treat with antibiotics.
Assess and treat if there is malnutrition and diarrhea with sufficient fluids and a high quality diet.
Treat pneumonia with appropriate antibiotics.
Refer suspected encephalitis to hospital.
Try to isolate admitted cases as much as possible. Make sure that all other children aged 6 to 59 months have had 2 doses of measles vaccine, at least one month apart, if they are in the hospital at the same time as the suspect measles case.
3 MEASLES OUTBREAK INVESTIGATION
For timely measles outbreak investigation, it is imperative that routine measles data is collected, collated and analyzed regularly. Outbreaks occur when the accumulated number of susceptible individuals is greater than the critical number of susceptible individuals for a given population to sustain transmission. Approximately 15% of children vaccinated at nine months of age and 5%of those vaccinated at 12 months of age fail to seroconvert, and are thus not protected after vaccination. In addition, cases may be identified from multiple health facilities in the same woreda within 30 days, if regular analysis is not done, outbreak detection may be delayed.
All suspected outbreaks should be investigated and confirmed by collecting blood specimens from the first five reported cases. You also need to take nasopharyngeal swabs from 5 cases to isolate viruses and document strains. The remaining suspected measles cases (epidemiologically linked) should be line-listed (sand sent to the next higher level.
A measles outbreak is defined as follows:
Suspected measles outbreak: Occurrence of five or more reported suspected
measles cases in one month in a defined geographic area such as a kebele,
woreda or health facility catchment area.
Confirmed measles outbreak: Occurrence of three or more laboratory
confirmed measles cases in one month in a defined geographic area such as a
kebele, woreda or health facility catchment area.
A measles outbreak can be suspected when:
A health facility reports an increase in the number of cases;
An unusual increase in the number of cases is noted during data analysis;
Five suspected measles cases or three confirmed measles cases reported;
Communities report an unusual number of cases or deaths;
When you detect an outbreak, conducted further investigation in order to:
Identify and manage additional cases that have not yet been reported;
Identify the source or the cause of the outbreak;
Control and prevent further spread of the outbreak;
Identify gaps in the immunization program that need to be addressed to prevent further spread of the disease.
Rumors notifications of
"a measles outbreak"
Organise to take at least 5 serum
speciemns for serological confirmation
Less than 3 cases IgM positive
3 or more cases IgM positive
Not a measles outbreak
Confirmed measles outbreak
Stop taking blood specimens for serologic
confirmation in the woreda until the end of the
Continue case based investigation and taking
outbreak
blood specimenns for serologic confirmaiton
from all suspected cases in the woreda
Take Naso-Pharyngeal swabs for viral isolation
from 5 cases (within the first 5 days of the onset
of rash) if not collected earlier
Manage cases, supplement with Vit A
Conduct active case search in the
community/adjacent Health Facilities/ districts
.Line list cases and analyze data
Figure 5.Diagrammatic presentation of measles outbreak
In order to guide appropriate response measures to a suspected measles outbreak, an outbreak investigation should be conducted. In investigating an
outbreak, both speed of the investigation and getting the correct answers are essential. To satisfy both requirements follow the following 10 steps:
1. Prepare for field work 2. Establish the existence of an outbreak 3. Verify the diagnosis 4. Define and identify cases 5. Analyze data collected in terms of time, place and person 6. Develop hypotheses 7. Evaluate hypotheses 8. Refine hypotheses and carry out additional studies 9. Implement control and prevention measures 10. Communicate findings
The steps are presented here in conceptual order. In practice, however, several may be done at the same time, or they may be done in a different order. For example, control measures should be implemented as soon as the source and mode of transmission are known, which may be early or late in any particular outbreak investigation.
3.1 Prepare for field work
In order to enhance the capacity to respond to measles outbreaks the Public
Health Emergency Management taskforce or an outbreak coordination
committee at woreda level should immediately get together to agree on the
need to investigate the suspected outbreak. Upon receipt of a report of a
suspected outbreak, activate the multidisciplinary outbreak investigation
team (rapid response team) and initiate outbreak investigation within 3
hours.
The role of the committee is to mobilize the resources needed and to coordinate the measles outbreak assessment, implementation and evaluation of the response. The committee should also ensure that the following actions are carried out:
Laboratory confirmation of the outbreak;
Ensure adequate clinical management of cases;
Intensify surveillance and notification of suspected cases;
Assess the risk of a large outbreak with high morbidity and mortality;
Investigate a confirmed measles outbreak;
Implement recommended control and preventive measures (including vaccination activities);
Ensure effective community involvement and public awareness.
The rapid response team might consist of:
A clinician who will both verify patients' clinical symptoms and train health care workers in good case management;
A lab technician who will take serum sample and train healthcare workers in correct sampling procedures;
An expert in information, education and communication who will assess how the community reacts to the disease and define and disseminate key health education messages; and
An epidemiologist who will initiate data collection and assess surveillance procedures.
Before leaving for the field, the team should:
Read and know about the suspected disease
Gather the supplies and equipment that are needed:
o Required formats(PHEM case based form, Measles line list,
House to House rapid monitoring of measles vaccine coverage, Measles risk assessment tool, Daily Epidemic Reporting Format for woreda and Region)
o This guideline and other reading materials o PHEM guideline o Laboratory equipment needed to take samples o Communication equipment o Drugs for initial response like vitamin A, tetracycline eye
ointment, anti-pyretic, and oral antibiotics)
o Data analysis tools (laptop)
Make necessary administrative and personal arrangements for travel,
Consult with all parties to determine each team members' role in the investigation and who your local contacts will be once you arrive on the scene.
3.2 Establish the existence of outbreak
Existence of an outbreak is established if the outbreak definition described
above is fulfilled. If a health facility suspects a measles outbreak, according to
the PHEM guideline the health facility should notify the woreda within 30
minutes. The woreda should notify the zone within another 30 minutes. The
zone should notify the region within another 30 minutes. And the region
should notify the Federal PHEM level within another 30 minutes. The total
time to report to the federal level should be within 2 hours.
3.3 Verify the diagnosis
The goals in verifying the diagnosis are:
Ensure that the problem has been properly diagnosed and
Rule out laboratory error as the basis for the increase in diagnosed cases.
When verifying the existence of an outbreak early in the investigation, you must also identify as accurately as possible the specific nature of the disease. Examine patients at the health facility and review records to confirm that the signs and symptoms meet the standard case definition. Review laboratory results for the people who are affected. If you are at all uncertain about the laboratory findings, a laboratory technician should review the techniques being used. Collect sample to isolate the organism or identify the evidence for infection.
3.4 Identify additional cases
Conduct active searches for unreported cases collect data on additional cases
using the line list form. Collect information on suspected cases using the line
listing form and make sure that the first five cases have PHEM case-based
reporting forms completed and blood specimens collected. Contact tracing
should be conducted in the communities where cases are identified to
determine if there are additional symptomatic individuals.
3.5 Analyze data collected in terms of person, p lace and time
Once you have collected some data, you can begin to characterize an
outbreak by time, place, and person. In fact, you may perform this step
several times during the course of an outbreak. Characterizing an outbreak by
these variables is called descriptive epidemiology. The data collected during
an investigation should be analyzed to determine why the outbreak occurred.
The data will help to identify in which group the susceptible individuals have
accumulated. This will allow corrective measures to be taken. Although a
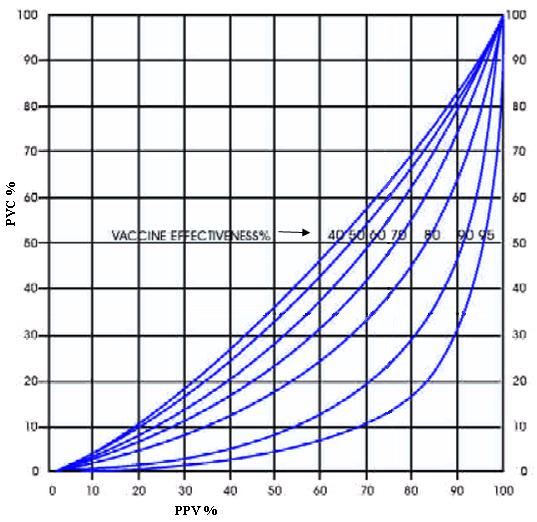
measles outbreak may occur despite high levels of immunization, it is usually
due to a failure to vaccinate. A high proportion of vaccine preventable cases
(PVPC) in an outbreak would suggest that a failure to vaccinate children is a
significant factor. Spot maps, demographic information and age-specific
attack rates can help to identify reasons for a failure to vaccinate.
Data analysis at this step will help you:
Learn what information is reliable and informative (e.g., the same unusual exposure reported by many of the people affected) and what may not be as reliable (e.g., many missing or "don't know" responses to a particular question).
Provide a comprehensive description of an outbreak by showing its trend over time, its geographic extent (place), and the populations (people) affected by the disease. This description lets you begin to assess the outbreak in light of what is known about the disease (e.g., the usual source, mode of transmission, risk factors, and populations affected) and to develop causal hypotheses.
Table 2.Example of analysis of measles cases distribution by Woreda (place) and age group (person),
zone X, 15-Jan-2012
Case(Percent) by age group
Age Specific AR
Characterizing by time traditionally, the time course of an outbreak is shown
by drawing a graph of the number of cases by date of rash onset. This graph,
called an epi-curve gives a simple visual display of the outbreak's magnitude
and time trend.
An outbreak curve provides a great deal of information.
You will usually be able to tell where you are in the course of the outbreak, and possibly, to project its future course.
You have identified the disease and know its usual incubation period; you may be able to estimate a probable time period of exposure and can then develop a questionnaire focusing on that time period.
To draw an epi-curve, you first must know the time of onset of illness for each person. The number of cases is plotted on the y-axis of an epi-curve; the unit of time, on the x-axis.
esaC of 80
Date of Onset
Figure 6.Example of an epi-curve of measles cases
Data collection, reporting, and analysis are done on daily and weekly basis. Consistently use reporting weeks that is the same as the surveillance week (i.e. Monday to Sunday) for all data collected during the outbreak.
Indicate with arrows the following dates on the epi-curve (dates that match those in the district logbook of suspected outbreaks and rumors.
Probable date of first case (found retrospectively as a result of the investigation)
Date first case was seen at a health facility
Date woreda was notified of the outbreak
Date woreda investigated the outbreak
Date woreda notified /zone region national level of the outbreak.
Date intervention started
Also do the following calculations and their interpretations: Case fatality rate (CFR), attack rate (AR), age specific attack rate(ASAR) and weekly incidence rate (WIR).The quality and reliability of the data is an important element to consider when interpreting the information.
3.6 Develop hypothesis
In real life, we usually begin to generate hypotheses to explain why and how
the outbreak occurred when we first learn about the problem. But at this
point in an investigation, after you have interviewed some affected people,
spoken with other health officials in the community, and characterized the
outbreak by time, place, and person, your hypotheses will be sharpened and
more accurately focused. The hypotheses should address the source of the
agent, the exposures that caused the disease.
When there is measles outbreak the hypothesis is on the cause of the
outbreak, either because of failure of vaccination or vaccine failure.
3.7 Evaluate hypothesis
The next step is to evaluate the credibility of your hypotheses. There are two
approaches you can use, depending on the nature of your data: 1)
comparison of the hypotheses with the established facts and 2) analytic
epidemiology, which allows you to test your hypotheses.
You would use the first method when your evidence is so strong that the hypothesis does not need to be tested. The second method, analytic epidemiology, is used when the cause is less clear. With this method, you test your hypotheses by using a comparison group to quantify relationships between various exposures (usually vaccination status) and the disease. There are two types of analytic studies: cohort studies and case-control studies. Cohort studies compare groups of people who have been exposed to suspected risk factors with groups who have not been exposed. Case-control studies compare people with a disease (case-patients) with a group of people without the disease (controls). The nature of the outbreak determines which of these studies you will use.
In most measles outbreaks, descriptive epidemiology combined with
laboratory results are sufficient to adequately evaluate a hypothesis that a
measles outbreak has occurred.
3.8 Refine hypothesis and carry out additional measures
When analytic epidemiological studies in steps above do not confirm the
hypotheses, reconsider your hypotheses and look for new vehicles or modes
of transmission.
Even when your analytic study identifies an association between an exposure and a disease, you often will need to refine your hypotheses. Sometimes you will need to obtain more specific exposure histories or a more specific control group.
When an outbreak occurs, whether it is routine or unusual, you should consider what questions remain unanswered about the disease and what kind of study you might use in the particular setting to answer some of these questions. The circumstances may allow you to learn more about the disease, its modes of transmission, the characteristics of the agent, and host factors. While epidemiology can implicate vehicles and guide appropriate public health action, laboratory evidence can confirm the findings.
3.9 Implement control and prevention measures
Even though implementing control and prevention measures are listed at this
step, in real outbreaks, prevention and control measures should begin as
soon as possible. In all measles outbreaks, the activities of strengthening
routine immunization, raising awareness of vaccination and effective case
management should be a top priority.
The following actions should be taken immediately:
Manage cases effectively to prevent complications: Case management depends on the severity of the disease. Suspected measles cases should be kept away from young unvaccinated children for the duration of communicability.
Inform the general public about the outbreak and the outbreak response: Health messages should include the importance of case management and encourage parents to get their unvaccinated under five children vaccinated.
Enhance surveillance to identify additional suspect cases.
Alert all health facilities neighboring woredas/zones about the suspected measles outbreak. Local physicians and traditional healers, and schools should also be visited to detect possible cases.
Strengthen routine immunization in areas at high risk for infection (e.g., in areas with low routine measles coverage, and crowded areas).
Assess the risk of extensive outbreak and based on the assessment result conduct outbreak response immunization (either selective or nonselective).
3.9.1 Implement case management
Make the necessary arrangements to provide appropriate and adequate case
management to all measles cases. This includes the provision of vitamin A,
the provision of supportive treatment, and the specific treatment of measles
complications. Complicated and severe measles cases will need to be
hospitalized for the purpose of intensive case management and require
isolation from other patients as much as possible. (For the details of case
management see part 2.4 above).
3.9.2 Reinforce routine vaccination
A measles outbreak provides the opportunity to identify program weaknesses
causing the outbreak and a chance to correct them. As soon as a measles
outbreak is suspected, and before laboratory confirmation of the suspected
measles cases, the following steps should be taken to reinforce routine
vaccination:
District staff, health-facility staff and partners should rapidly identify priority areas within the affected district (e.g. communities with low vaccination coverage and at high risk of morbidity and mortality).
Jointly work on strengthening the available district immunization work plans.
Locate health centers conducting immunization sessions that may need additional staff or vaccine supplies.
Organize corrective measures such as additional outreach services to communities with a high proportion of unreached children.
3.9.3 Implement Selective or Nonselective Vaccination
Selective vaccination aims to increase population immunity by focusing upon
quickly increasing measles coverage for unvaccinated children.
Nonselective vaccination aims to increase population immunity by y focusing
upon quickly increasing measles coverage for all children regardless of
vaccination status.
As part of the outbreak investigation, a risk assessment should be provided to guide the choice between selective and nonselective vaccination.
Assess risk of a large outbreak with high morbidity and m ortality
As soon as the outbreak is suspected, the risk of a large outbreak with high
morbidity and mortality must be assessed. This assessment is needed to
determine what type of vaccination response (selective or nonselective) is
most appropriate to control the outbreak.
Evaluate the susceptibility of the population and potential for spread both in the affected woreda and neighboring woredas (use table of calculating the accumulated susceptible )
Evaluate the risk factors for further transmission, morbidity and mortality in the areas (other than accumulated susceptible the risk factors are: a high level of malnutrition in the woreda, presence displaced population, measles surveillance gaps, measles outbreak season, adjacent woreda affected by measles all increase the risk factors for measles transmission and measles mortality.
If the assessment result is a low risk of an extended outbreak – use a selective vaccination strategy, but if the risk assessment result is high, use non selective vaccination strategy.
Table 3. Risk factors to consider in choosing nonselective rather than selective vaccination in a confirmed
measles outbreak
Explanation
The pool of susceptibles (all ages) is greater than 2/3rd
of the annual birth cohort of children. Use Annex 1, Measles Risk Assessment Tool for the last 5 years calculation of susceptiables.
Emergency levels of severe acute malnutrition
Outbreak in neighboring woreda
Population movements into an area where prior
vaccination status is uncertain (displacements)
In the absence of the above risk factors (possibly due
to lack of accurate assessment data), in an intense measles outbreak with over 100 cases within 3 months (within a woreda) and/or prolonged >3 months duration, non selective measles outbreak response immunization should be considered on a case by case basis.
Where there is a large pool of susceptible individuals, a small number of
confirmed measles cases may forecast a large outbreak that may be
interrupted by a timely nonselective vaccination intervention.
In some cases, due to high population vulnerability, a small number of cases
may be associated with increase case fatality or complication rates that may
be prevented by a timely nonselective vaccination intervention.
Even with a low risk assessment, an intense or prolonged outbreak with a
significant number of cases point to the need to increase immunity through
vaccination.
Selective vaccination
This is used when the risk for an extended outbreak is relatively low and/or
the capacity to conduct a wider vaccination campaign is low. As soon as a
measles outbreak is confirmed, the following steps should be taken.
Enhance social mobilization activities to inform the affected communities about the suspected outbreak, inform the age group of previously unvaccinated children being targeted for selective measles vaccination, and where parents should bring their at-risk children for vaccination.
Vaccinate all children (6 to 59 months of age) presenting to a health facility or a vaccination site without a written history of measles vaccination. Children receiving measles vaccine before the age of nine months must be revaccinated after the age of nine months (with at least a one-month interval between the doses).
Vaccinate hospitalized children.
Ensure availability of sufficient supplies. Use stock management records to determine available quantity and location of vaccine, auto-disable syringes and other supplies (e.g. diluents, mixing syringes, cold-chain equipment, antibiotics and vitamin A) that are available immediately for use. Estimate and request the additional supplies needed so that activities are not interrupted due to supply stock outs.
Typically selective vaccination targets children aged 6 months to 59 months
with no history (verbal or written) of prior vaccination. However should the
outbreak investigation indicate a different target group, e.g. evidence of
most cases being under 4 years or a significant number of cases being up to
10 years of age, a different age group should be considered.
Nonselective mass vaccination
As soon as the outbreak is confirmed, and if the risk assessment results
indicate that there is a high risk of a large measles outbreak, then
nonselective vaccination should be planned. Zonal, regional, and/or national
authorities (in case of bordering woredas) should coordinate the scale of a
nonselective campaign based on a wider risk assessment.
For additional resource mobilization beyond local capacity, the Regional Health Bureau should communicate its plan to national level PHEM by sending the findings of risk assessment and line listing data. At national level, mobilization of vaccines and injection materials will be coordinated through PHEM-TTF. The PHEM-TTF will evaluate the ability to mobilize external
resources for the operational and logistical aspects of the campaign; and determine if the vaccine and other supplies can be made available at the time needed based.
If there are sufficient resources to carry out a safe and timely vaccination campaign, then a mass vaccination campaign should be carried out in the targeted areas (affected and neighboring areas as determined by the risk assessment). If routine vaccination stocks are used, the plan should include replenishment stocks.
For the nonselective mass vaccination response, the timing, target age group and area for vaccination should be defined as outlined below.
Routine vaccination coverage and coverage during SIAs in each birth cohort;
Age specific attack rates; or the distribution of cases by age;
Absolute number of cases;
Geographical distribution of the disease.
Once the decision to intervene with nonselective vaccination is made, using the SIA micro planning guideline, a micro-planning exercise should be performed to determine the vaccine, logistics, staffing and communication needs for location to be targeted for the campaign. The response should target both outbreak-affected areas and adjacent areas in which the risk assessment shows a high risk of spread.
Children receiving measles vaccine before the age of nine months during a
campaign must be revaccinated after the age of nine months (with at least a
one-month interval between the doses), since the efficacy of vaccine
administered before nine months of age is likely to be low.
3.9.4 Measles prevention and control measures in emergencies
Humanitarian emergencies, such as a flood leading to large population
displacement, increase the health needs of children and adolescents and
must be addressed quickly to prevent in unnecessary mortality. Measles,
specifically, is too often one of the major causes of child deaths in
humanitarian emergencies and further contributes to excess morbidity and
mortality by reducing immunity, exacerbating malnutrition, and increasing vitamin A deficiency. Vaccinating children against measles during emergencies is among the most cost-effective preventive public health measures and a priority health intervention.
Measles immunization, together with vitamin A supplementation, is recommended by WHO and UNICEF as a primary response intervention following an emergency. Immunization should include all children from 6months through 14 years of age. If scarce resources make this impossible, all children aged between six months and five years must be immunized as a minimum. The scope of any outbreak response immunization activity should be based on local epidemiological data available to identify the age-group affected and geographic extent of the outbreak, vaccine availability and funding In Ethiopia, due to the risk of polio importation, if the emergency includes persons entering the country, polio (OPV) vaccination is also strongly recommended for children up to 5 years of age.
3.10 Communicate the findings
The data should be analyzed rapidly to determine the extent and severity of
the outbreak, vaccine effectiveness, potential risk factors for measles
infection, and possible causes of the outbreak. Communicate the findings of
the assessment immediately to those who needs to know either orally or in
written report.
You should present your findings in scientifically objective fashion, and you should be able to defend your conclusions and recommendations.
You should also provide a written report that follows the usual scientific format of introduction, background, methods, results, discussion, and recommendations. By formally presenting recommendations, the report provides a blueprint for action. It also serves as a record of performance, a document for potential legal issues, and a reference if the health department encounters a similar situation in the future. Finally, a report that finds its way into the public health literature serves the broader purpose of contributing to the scientific knowledge base of epidemiology and public health.
Whenever outbreaks of measles are controlled, woreda health managers should ensure that the PHEM outbreak investigation report is completed and the process of outbreak investigation and response is properly documented and analyzed at country level.
The woreda rapid response team is expected to write and submit a report within 24 hours of investigation while the summary of the outbreak should be submitted within 2 weeks of the investigation. Since the outbreak may be protracted, data collection and regular updates will have to continue weekly until the outbreak is over. An outbreak investigation report helps to summarize and document the process and results of the investigation. Such reports are crucial for evaluation of the response and to give feedback to concerned bodies.
The outbreak is declared over when there are no additional cases reported during 2 incubation periods (or approximately 4 weeks).
The feedback process and mechanisms in measles surveillance are identical to the AFP surveillance model. Feedback concerning surveillance performance and results should be given in written form on-site supervisory visits and during the periodic surveillance review meetings.
4 EFFECTIVE COMMUNICATION FOR BEHAVIOR
In measles surveillance changing social and individual attitude and behavior by providing the community with relevant information, education and motivation through appropriate channels including interpersonal and participatory methods is crucial. As health workers and communities learn about measles the information should result in behavior change characterized by the following:
Unawareaware concerned knowledgeable motivated to change practicing a trial of behavior practicing sustained behavior change.
This continuum shows that it is a long process and requires sufficient time. Enabling factors such as providing friendly discussion is important.
Behavioral change communication involve the following
An interactive process with communities, and health professionals;
Integrated into an overall program;
Designed to develop tailored messages and approaches using a variety of communication channels;
A process that helps to develop positive behaviors; and
To promote and sustain behavior change.
When interacting with health professionals and communities, two-way participatory communication is advisable. Make sure that the information to be conveyed is at their level of understanding. Provide regular feedback in the form of supervision and written reports. Encourage health workers to read guidelines and other materials to increase their awareness.
Make sure behavior will improve health;
Provide necessary enabling factors;
Identify beliefs that might influence the person's attitude;
Find out whether the influences operate on the individual, family, community or higher levels;
Key messages for the community are the following:
Among the vaccine-preventable diseases, measles is a leading cause of mortality.
Measles can lead to blindness, deafness, brain damage, and death.
Measles vaccine is safe and effective.
Take children who develop measles symptoms to the nearest health facility for treatment to prevent complications.
Report immediately any person with rash and fever to the nearest health facility.
Routine measles vaccination at nine months of age and a second dose of measles vaccine during campaigns are necessary to prevent measles outbreaks.
Children have the right to be protected against measles by vaccination.
5 MONITORING AND EVALUATION
Monitoring and evaluation is needed to assess the outcome and impact of measles control activities. The following aspects need to be monitored
Routine immunization program indicators
Surveillance indicators
Laboratory proficiency
Outbreak investigation reporting and follow-up
Laboratory confirmation of outbreaks
5.1 Immunization coverage survey
Coverage levels of successive birth cohorts can be monitored regularly from
the reported data. Reported data are at times unreliable; hence there is a
need for independent coverage evaluation surveys to validate reported
coverage levels. Correct estimates of measles coverage levels are essential to
determine community immunity levels and plan for SIAs (to provide second
opportunity) in an attempt to reduce susceptible populations.
5.2 Surveillance indicators
To assure high-quality surveillance, the surveillance system must be
monitored regularly and systematically, using a set of formal indicators.
Regular feedback to everyone involved in the surveillance system using
monitoring indicators is important to assure sustainability and refinements to
the system
Primary indictors
Annualized detection rate of non-measles febrile rash illness (Target >2 case non-measles febrile rash cases per 100,000 populations per year).
Proportion of woredas that have reported at least one case of measles (or >1 reported case per 100,000 population) with a blood specimen per year (Target >80%).
Supplementary indicators
Proportion of reported measles cases with a blood specimen collected within 28 days of rash onset (Target >80%) [Exclude epidemiologically linked cases from the denominator].
Annualized rate of investigation (with blood specimens) of suspected measles cases (Target >2 case investigated with blood specimen per 100,000 populations per year).
Timeliness of health facility weekly reporting to the woreda level within the specified time period. (Target: at least 80% of reports received within the specified period).
Proportion of measles outbreaks investigated with a blood specimen from the first five cases (Target: at least 80% of measles outbreaks investigated with blood specimen collection).
Timeliness of suspected measles case investigation (Target: at least 80% of suspected cases investigated within three days following notification).
Proportion of outbreaks for which Nasopharyngeal specimen is collected (Target at least 80% of outbreaks)
Specimen collection and shipment
Specimen collection and shipment require careful monitoring to ensure proper testing of samples in the laboratory.
Proportion of cases with adequate specimen (One blood specimen collected within 28 days of onset of rash). Target: >80%
Proportion of specimens arriving at the laboratory in "good condition" ("good condition" means that upon arrival there are frozen ice packs or ice, or a temperature indicator (showing <8°C) in the container, the specimen volume is adequate (at least 2 ml of serum), there is no evidence of leakage, and appropriate documentation (laboratory request/reporting form) is completed). Target: 90%
Timeliness of serum/ dried blood specimens arriving at laboratory (Target: at least 80% of specimens arriving at the laboratory within three days of specimen collection).
Program indicator
Proportion of laboratory confirmed measles cases (Target: <10% of investigated suspected measles cases confirmed to be measles by serological testing).
5.3 Laboratory indicators
Timeliness of feedback of serology results from the laboratory to the national level (Target: at least 80% of results sent out by the laboratory to the national level within 7 days of receipt of specimens at the lab).
Proficiency testing of laboratories - Periodic proficiency testing requires ensuring working of measles laboratory as per WHO accreditation standards.
Proportion of representative serum specimens sent quarterly by the national laboratory to the WHO AFRO regional reference labs for re-confirmation as part of quality assurance measures (Target: at least 10% of specimens tested at national lab shared with the regional reference laboratory).
Proportion of concordance of measles IgM results between the national measles lab and the regional reference lab (Target: at least 90% concordance of results of shared specimens between the national and the regional reference laboratories).
Timeliness of feedback of serology results from the WHO AFRO regional reference laboratory (RRL) to the national measles laboratory (Target: at least 80% results sent to the national measles lab within 14 days of receipt of specimens at the RRL).
5.4 Outbreak monitoring &evaluation
Attack rate (AR): Attack rate is an incidence rate (usually expressed as a
percent), used only when the population is exposed to measles risk for a
limited period of time such as during an outbreak. It relates the number of measles cases in the population at risk and reflects the extent of outbreak.
Age-specific attack rate (ASAR): If population data are available for the area
of the outbreak, age-specific attack rates can also be calculated.
Case-fatality rate (CFR): Based on the case investigations and the total
number of confirmed cases, this rate calculates the proportion of deaths
among the total number of cases.CFR should be estimated by age-group, if
possible.
Proportion of vaccine-preventable cases (PVPC): It is also possible to
estimate the proportion of vaccine preventable cases. This is the number of
cases occurring in children who were not immunized or who were immunized
before the recommended age and not re-immunized at the correct age, as a
proportion of the total number of cases.
5.4.1 Immunization coverage survey during an outbreak
Routine immunization coverage successive birth cohorts can be monitored
regularly from the reported data. Reported data are at times unreliable;
hence there is a need for independent coverage evaluation surveys to
validate reported coverage levels. During outbreaks, when there is no routine
immunization data or there is concern that reported coverage levels may not
reflect population immunity, a rapid convenience surveys can be used to
assess the coverage of the local community (use Annex 1). Accurate estimates
of measles coverage levels are essential to determine community immunity
levels, perform risk assessments and plan for SIAs (to provide second
opportunity) to reduce susceptible populations.
5.5 Vaccine effectiveness
Vaccine effectiveness (VE) is the ability of a vaccine to provide protection
under the normal conditions of a public health vaccination program. Since no
vaccine is 100% effective, not all persons given measles vaccine are
necessarily protected against measles. Therefore, during a measles outbreak
the occurrence of measles cases among persons with documentation of measles vaccination should be expected. It is expected, when vaccination coverage is high, a significant proportion of cases may occur among vaccinated persons as the pool of susceptible individuals includes those who have been vaccinated but did not seroconvert. The occurrence of measles cases in vaccine persons often leads to doubts about the effectiveness of measles vaccine.
Several approaches can be used to estimate vaccine effectiveness. They include prospective cohort trials and case-control studies as part of an outbreak investigation. The difference between attack rates among vaccinated persons (ARV) and attack rate in those among the unvaccinated (ARU) is expressed as a fraction of the attack rate among unvaccinated persons (ARU). The calculation of vaccine effectiveness in these methods is follows:
But this method is time-consuming and often unnessesary. An estimate of VE can be obtained from outbreak and routine coverage data. This alternative method allows a rapid estimation of vaccine effectiveness when the proportion of cases occurring in vaccinated individuals (PCV) and the proportion of the population that is vaccinated (PPV) are known. It is calculated as follows:
The intersection of PPV and PCV is shown in the figure below. For example a PPV of 90% and PCV of 30% fall on the 90% vaccine effectiveness line.
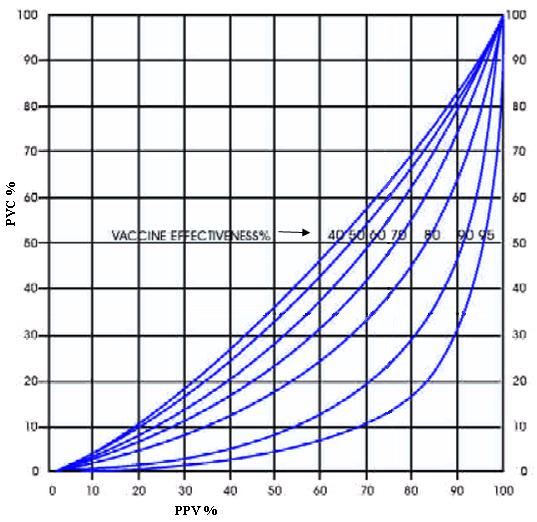
Figure 7. Relationship between percentages of cases vaccinated (PCV) and percentage of the population
vaccinated (PPV) for seven different percentage values of vaccine effectiveness (VE)
6 ANNEXES
Annex 1. Data collection and reporting formats
PHEM Case-based Reporting Format (CRF)
Woreda Suspected Outbreak and Rumor Log-book
Measles Line List
Measles Risk Assessment Tool
House to House Rapid Monitoring of Measles Vaccine Coverage
PHEM Case-based Reporting Format (CRF)
Reporting Health Facility:
Disease type (put tick mark )
Anthrax
Neonatal Tetanus
Hemorrhagic Fever
Name of Patient:
Date of Birth (DOB):
Age (If DOB unknown):
(if under 12 mos.)
M = Male, F = Female
Patient's Address:
Locating Information
Location when symptom started:
Current location:
If applicable or If the patient is neonate or child, please write full name of mother and father of the patient:
Date Seen at Health Facility:
Date Health Facility notified
Date of Onset:
Number of vaccine/TT doses received:
For cases of NNT* , Measles, Yellow Fever, and
Meningitis (For NNT, Measles, Yellow Fever – refer
Date of last vaccination:
immunizationcard & for Meningitis - ask history)
*For NNT cases please complete the additional case
investigation form (NNT, Measles, Yellow Fever and
Meningitis only)
Associated with epidemics?
In/Out Patient
Treatment given
Outcome of the patient at
the time of report:
Fill only if specimen is collected and sent to Lab
Date of specimen collection:
Date of specimen sent to lab:
Type of specimen:
(put tick mark )
Date form sent to woreda:
Name and signature of the person completing the form:
Signature
Telephone
For official Use only
ID Number:
Date form received at National/Regional level:
classification of
case
Classification for
Name and signature of the official:
Signature
Telephone
Woreda Suspected Outbreak and Rumour Log -book
Record verbal, media or written information about suspected epidemics, rumors or
reports of unexplained events
Measles Line List
Health Facility:
Date received:
Lab Tests
** Outcome
(A) Alive
o Patient
Comments
*Age in years if more than 12 months, otherwise write age in months (e.g. 9m)
**Indicate the complication in the comments.
Measles Risk Assessment Tool
Calculation of the accumulation of susceptible population for measles
outbreak
Additional factors to be considered when we asses risk of spread
are the following
Outbreaks of measles in adjacent districts
Peak season for measles transmission
Presence of special populations (like displaced population, refugees.) and living conditions that facilitate transmission
Drought affected area with high level of malnutrition
House to House Rapid Monitoring of Measles Vaccine Coverage
Reporting Health Facility:
Date of assessment
Number of
children age less
ated (card, Hx,
Reason for not
yearsinthe house other )
vaccinated
Other observation
Annex 2. Role of each Level in the Health System
The roles and responsibilities of health workers and authorities at various
levels of the health care system, in establishing and conducting measles
surveillance activities, are described below:
In order to strengthen the measles case-based surveillance, all regions should ensure that the surveillance system is organized as far as the community level and should discharge the following roles and responsibilities expected at each level.
Role of the Community and Family
Report any person with fever and rash to the nearest health facility.
Keep patients isolated.
Minimize visitors as much as possible.
Make sure that their children are vaccinated against measles.
Role of the Health Facility
Detect and report cases and outbreaks using the standard case definition.
Collect 5 ml of blood (or an appropriate sample of dried blood on filter paper) from all suspected individual measles cases.In outbreak settings (more than five suspected measles cases), specimens for measles IgM testing (serum or dried blood on filter paper) as well as throat swabs for virus isolation should be collected from the first five cases of suspected measles.
Begin case management for measles and its complications
Arrange for transport of specimens to EHNRI within 3 days of collection.
Ask the family about other persons with similar symptoms.
Monitor for other suspected cases.
Implement respiratory isolation of hospitalized measles cases.
Provide results back to family and community.
Ensure all admitted patients of 6 – 59 months of age have received two doses of measles vaccine, at least one month apart.
Collect, consolidate, analyze and interpret surveillance data.
Conduct active case search and sensitize community members and health workers.
Role of Woreda Health Office
The Woreda should coordinate activities of health facilities located in the
area.
Review case investigation form for timeliness and completeness.
Ensure blood/filter specimen is collected and sent to EHNRI from all individual suspected measles cases or from the first five cases during outbreaks.
Notify zonal/regional surveillance focal person.
Notify other health facilities in the Woreda.
Monitor the epidemic threshold.
Conduct a measles outbreak investigation promptly once the outbreak threshold is reached, including conducting active case finding in the community and line listing all identified cases.
Ensure that Naso-pharyngeal swabs are collected from the first five suspected measles cases during outbreaks in order to determine the circulating viral strain.
Provide feedback to health facilities and feed data forward to the next level (zone/region).
Analyze disease patterns and trends, interpret data, and report.
Do active case search and sensitize community members and health workers.
Role of Zone/Region
Support the Woreda and health facility.
Ensure that the surveillance guidelines are followed.
Monitor the surveillance performance using standard indicators.
Provide feedback to peripheral levels.
Supervise and provide technical support to woredalevel activities.
Monitor for the possible occurrence of an outbreak.
Analyze disease patterns and trends, interpret data, and produce routine reports.
Do active case search and sensitize community members and health workers.
Role of National Level and Regional Laboratories
Record the date the specimen arrives in the laboratory (EHNRI).
Confirm measles cases using ELISA within seven days of receipt of specimen at the National Laboratory (EHNRI and Regional labs).
Assign the epidemiologic tracking (EPID) number.
Analyze disease pattern and trends and interpret surveillance data in conjunction with the routine immunization coverage data, and produce routine reports.
Monitor the surveillance performance using standard indicators.
Use data to evaluate national objectives and to direct the control program.
Support the regions, zones and woredas.
Facilitate notification of laboratory results to Woreda (e.g., fax, phone, mail, radio).
Classify suspect measles cases.
Review technical and programmatic issues regularly.
Do active case search and sensitize community members and health workers
Source: http://www.moh.gov.et/documents/26765/28902/National+Measels+Guideline_2012/be976de6-2ccf-41a3-b204-9e089d3d216c;jsessionid=5B0D31230D1BF7B06F7C3D8DA40DF344?version=1.0
Available online at EPA Guidance on tobacco dependence and strategies for smoking cessation in people with mental illness T. Ru¨ther ,J. Bobes , M. De Hert T.H. Svensson K. Mann , A. Batra P. Gorwood H.J. Mo¨ller a Department of Psychiatry, Ludwig Maximilian University, Nussbaumstrasse 7, 80336 Munich, Germany b Department of Medicine, Psychiatry Area, University of Oviedo, Centro de Investigacio´n Biome´dica en Red de Salud Mental, Cibersam, Oviedo, Asturias, Spain
Uncaria tomentosa Family: Rubiaceae Common Names: cat's claw, unha de gatoParts Used: Vine bark, root Description Cat's claw (U. tomentosa) is a large, woody vine that derives its name from hook-like thorns that grow along the vine and resemble the claws of a cat. Two closely related species of Uncaria are used almost interchangeably in the rainforests: U. tomentosa and U. guianensis. Both species