Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Microsoft word - ajpms
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
COMPARISION OF TWO ANAESTHETICTECHNIQUES IN DAY CARE
Richa Chandra*
, Juhi Saran
Department of Anaesthesia and Critical care, Shri Ram murti Smarak Institute of Medical Sciences Bareilly India.
Corresponding author's Email: [email protected]
The preset study was undertaken on 80 patients ASA grade I and II for day care surgeries having procedures lasting less than 30 min. The patients were divided into two groups of 40 patients each which was again divided into to two subgroups a and b. One a who were receiving two antiemetic drugs and others b who were not receiving any antiemetic drugs.Both group received same techniques for induction with Midazolam 1 mg, Fentanyl 1-2mcg per kg and Propofol 2mg per kg.First group was maintained with Propofol 75-150mcg per kg per minute with oxygen33% and Nitrous oxide 67% mixture in spontaneously breathing patients with face mask. Second group was maintained with variable rate of Isoflurane 1-4%, and Oxygen 33% -Nitrous oxide 67% mixture. Hemodynamic parmeters were similar in both groups. Recovery in terms of modified Alderate Score was noted. Both groups have almost similar recovery. 1 patient in-group Ib and 3 patients' in-group II b had nausea of which one has vomiting also. It was corrected with injection Ondansetron. The incidence of nausea is around5%in1b and 15% in2b. The incidence of vomiting in-group is around 5%, which is not significant. So to conclude both the techniques are similar in terms of recovery. There is no use of antiemetic drugs, in short day care surgeries in ASA Gr I-II patients, if we are using Propofol induction and Propofol maintenance technique.
KEYWORDS: Recovery, Modified Alderate Score, PONV, Ambulatory surgery
---------------------------------------------------------------------------------------------------------------------------------------------
INTRODUCTION Ambulatory surgery offers a number of advantages for patient, healthcare provider's third party payers and even
hospitals. Patients' benefit from ambulatory surgery because it decreases patient, s separation from their home and
family environment and decreases their like lihood of contracting hospital acquired infections and postoperative
complications. Compared with traditional hospital admissions, there are less preoperative medications following
ambulatory surgery. Unlike inpatient surgery, ambulatory surgery does not depend on the availability of a hospital
bed. The cost is 75% lower than for similar in patient care and the efficiency of the operative rooms appears to be
significantly increased.[1] Anesthesia for day care surgery should ensure a rapid recovery with swift return to street
fitters. Furthermore it is of paramount importance to keep the patient complication free.Anesthesia technique should
include smooth and rapid induction,intraoperative amnesia and analgesia,good surgical conditions ,short recovery
period and free of side effects.But increasing awareness about the importance of patient satisfaction on daycare basis
make Post Operative Nausea and Vomiting [PONV] an increasingly significant problem in postoperative care. PONV
in unpleasant for the patient and may delay discharge from the ambulatory surgical unit or result in unexpected
overnight hospitalization.[2,3] Incidence reported varies between 20%-30%
At present Propofol TIVA [total intravenous anesthesia] is more expensive than inhalational anesthesia with
Isoflurane and Nitrous Oxide. But it could be cost effective because the costs of treating PONV and of increased
1 P a g e
Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
recovery room stay after inhalational anesthesia offset the additional drug acquisition costs of Propofol TIVA.
Propofol has become the drug of choice for induction of anesthesia in the outpatient setting. Propofol infusions are
also becoming increasing by popular for maintenance of outpatient anesthesia.[4]
MATERIALS AND METHODS
After approval by the hospital ethical committee ASA Grade I and Grade II patients aged. Between 15 to 45 years
undergoing short operative lasting less than 30 minutes, e.g. D and C, Cystoscopy, Implant removal etc were taken up
in the study after taking an informed consent from the patients A thorough history was elicited including any history
of major illness or disease, any history of drug allergy, or history of previous anesthesia exposure, history of PONV
and any other personal history was asked for. General physical examination and systemic examination of each patient
was performed to exclude any inter current disease. Investigations-Patients were investigated routinely for complete
blood count, blood urea, urine routine and microscopy, ECG, CXR and BT & CT. Exclusion Criteria- ASA grade III
or IV, history of alcohol or drug abuse, history of allergic reactions to drugs, history of motion sickness, history of
PONV, use of antiemetic drugs in last 24 hours of surgery, patients below 18 years and above 65 years, emetogenic
surgeries.80 patients (40) in each group taken up for study. No premedication was given to the patients. On arrival in
operation theater, standard monitoring devices were attached e.g. ECG, NIBP, pulse oximetry.All patients received
oxygen via facemask for 2-3 minutes before induction of general anesthesia. All patients received 500ml Ringer
Lactate before induction in preoperative room. Patients were randomly assigned to one of the anesthetic technique
groups.
GROUP I All 40 patients received Midazolam 1 mg, Fentanyl 1-2 mcg per Kg and dynapar 40mg intravenously at
the time of induction. Patients were induced with Propofol infusion at the variable Propofol 2 mg per kg
intravenously and maintained with Propofol infusion at the variable rate of 75-150 mcg per kg minute intravenously
with Nitrous Oxide 67% and oxygen 33% mixture in spontaneously breathing patients with facemask. This groups I
was again divided into 2 subgroups i.e. I a and I b.
GROUP Ia - Patients in this group received two antiemetic drugs [Ondansetron 4mg and Metoclopramide 10 mg
GROUP Ib- Patients in this Subgroup did not receive any antiemetic drugs.
GROUP II- In this group all 40 patients received Midazolam 1 mg, Fentanyl 1-2µg per kg and dynapar 40 mg
intravenously. Patients were induced with Propofol 1 2mg per kg IV and maintained with variable rate of Isoflurane
1-4% I combination with 67% nitrous oxide and 33% oxygen. This group was again divided into two sub groups i.e.
IIa and2b .
GROUP IIa- Patients in this subgroup received two antiemetic drugs Ondansetron 4mg, Metoclopramide 10mg
intravenously.
GROUP IIb- Patients in this subgroup will not receive any antiemtic drugs. All patients were allowed to breathe
spontaneously. Absence of purposeful movements and tachypnea (i.e. RR<20 bpm) were considered optimal
intraoperative analgesia.
OBSERVATION: Data was managed in an excel spreadsheet. Quantitative values were assessed for approximately
normal distribution Subsequently each of those variables was summarized by mean and standard deviation. Mean
values for quantitative variables among all the four subgroups uses compared using one way analysis of variance. For
2 P a g e
Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
comparing the two main groups ‘paired t test' were applied. SPSS statistical software was used for data analysis. In this study p value less than 0.005(p<0.05) have been considered as stastickally significant. All patients were randomized and followed up to the time of discharge with no dropouts Total 80 patients[40] in each group were studied.
Table:1 Types of surgeries
Dilatation and curettage
Incision and drainage
Table:2 Demographic Data
MeanAnaesthesia 20.25*6.39
surgical 18.27*6.35
Total surgical time from incision to placement of dressing was noted. Total anaesthesia time was considered from induction to discontinuation of anaesthetics.On awakening from anesthesia, patients were revaluated at 1-minute intervals with respect to their ability to meet specific (fast track) discharge criteria.Recording of following at 5 minutes interval was done.-Mean arterial pressure,Heart rate,Oxygen saturation,Respiratory rate
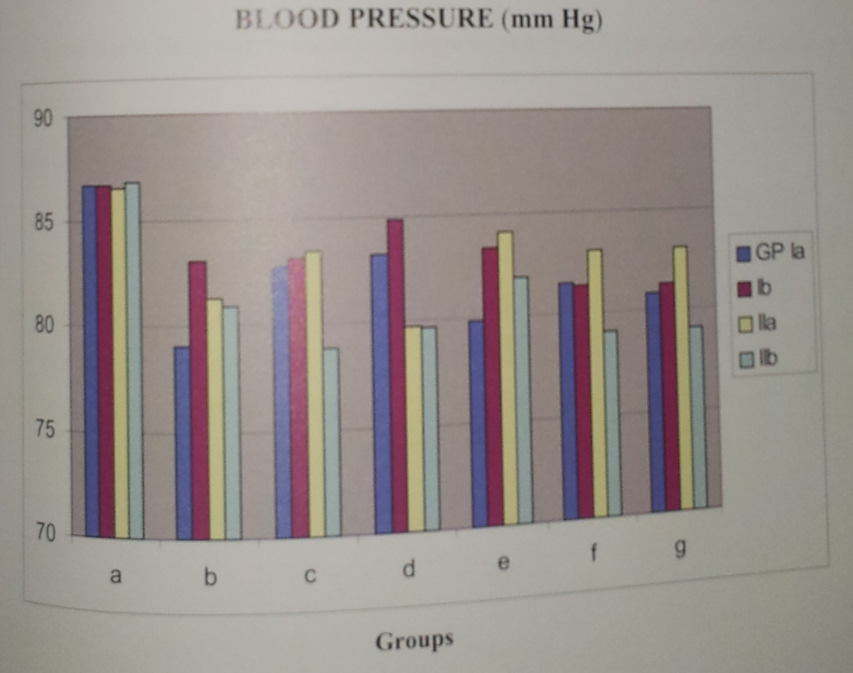
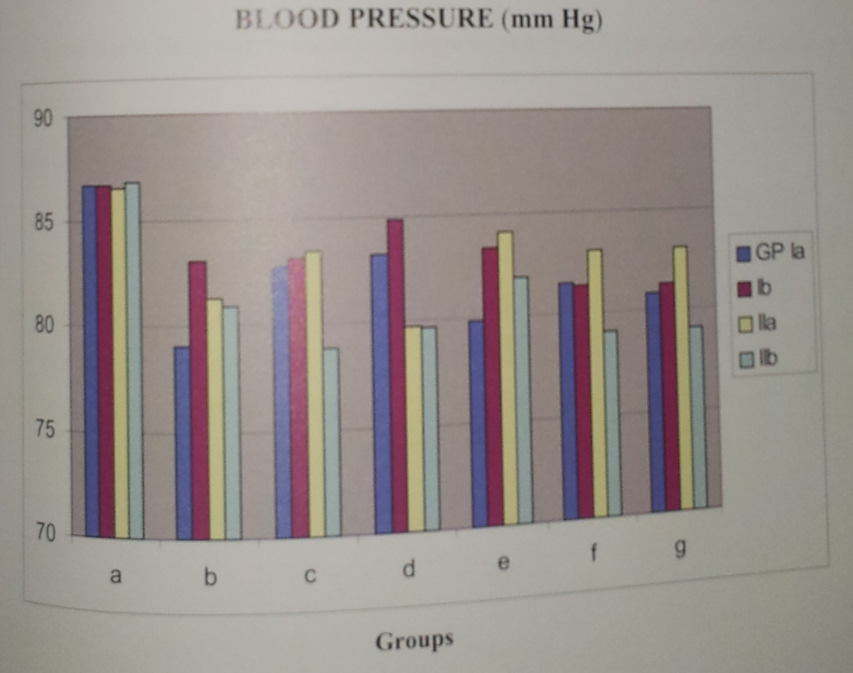
Blood Pressure remained stable without much change from the baseline in all four groups during the procedure and postoperatively. Hypotension was defined as fall in blood pressure of more than 20% of the base line.In our study, induction of anesthesia with Propofol produced a fall in B.P. initially in one case without significant change in the heart rate. Mostly patients were of young age group of [18-55 yrs], ASA I-II group .We did short procedures of < 30 minutes duration without major fluid shifts, so we considered pre operative fasting [sometimes up to 12 hours] the main cause for this fall in BP. Subsequently we started pre loading of every patient with Ringer lactate 500ml before induction.Only one patient showed drop in blood pressure in group la, which was improved with injection Mephenteramine. 6 mg and Ringer Lactate 500 ml.
Mean BP was recorded preoperatively among the sub groups la and lb were 77.60 and 85.3500 mm of Hg. The mean BP in subgroups lla and llb were 86.9500 and 81.1000 mm of Hg. So both groups were comparable.
3 P a g e
Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
Figure: 1 Blood Pressure record of different group with sub group:
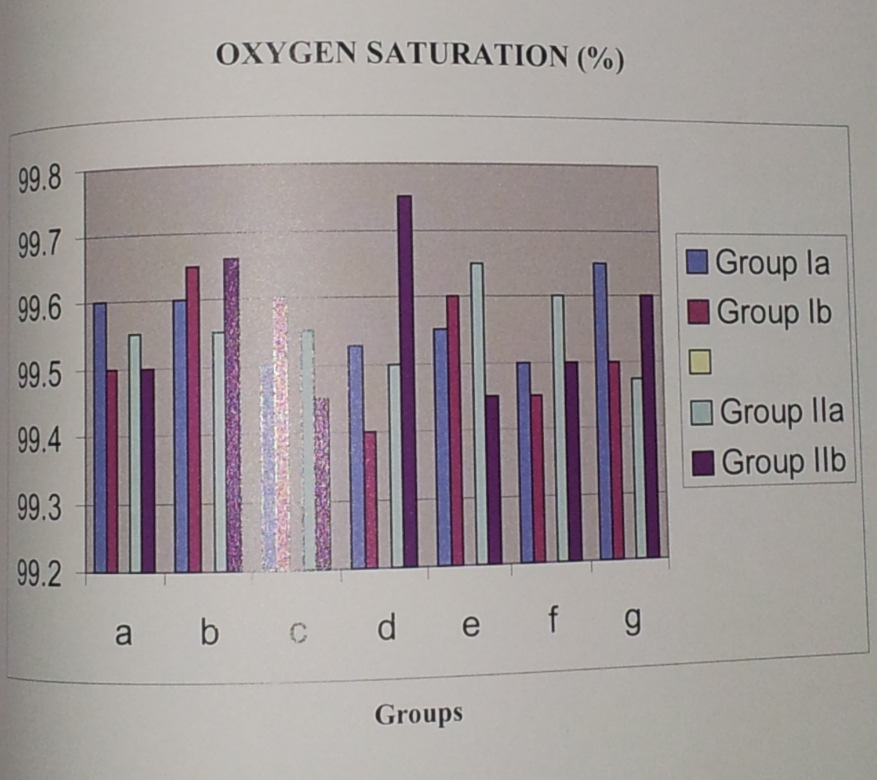
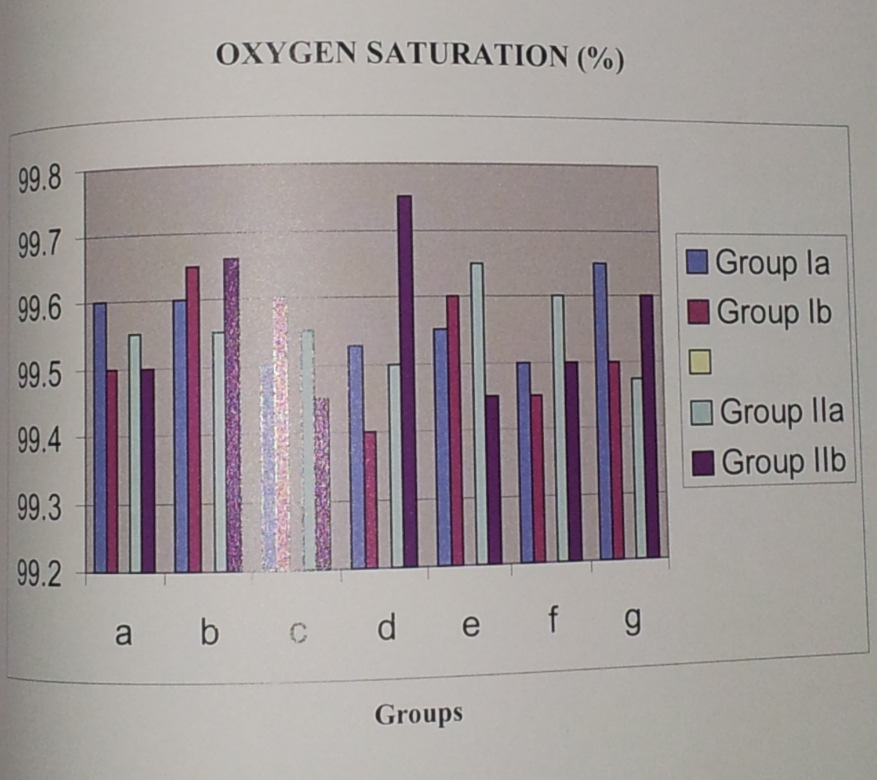
There was no stastically significant difference in oxygen saturation between these two subgroups at any stage during the study p> 05. The preoperative oxygen saturation of all groups were comparable and these was no statistically significant difference between them, P value > 0.05. Although mostly patients in Propofol infusion, group had apnea which was corrected by mask ventilation.
Figure: 2 Oxygen saturation (%) of different group
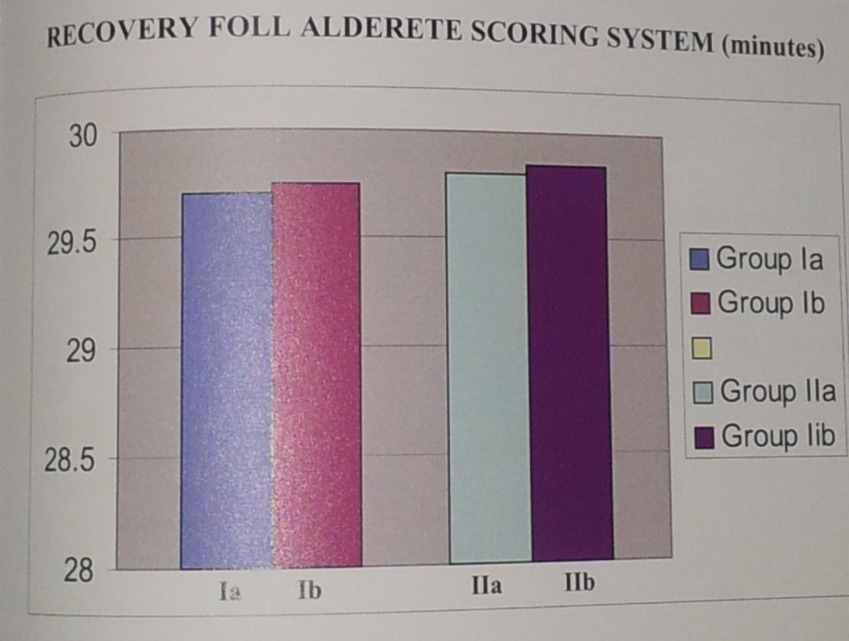
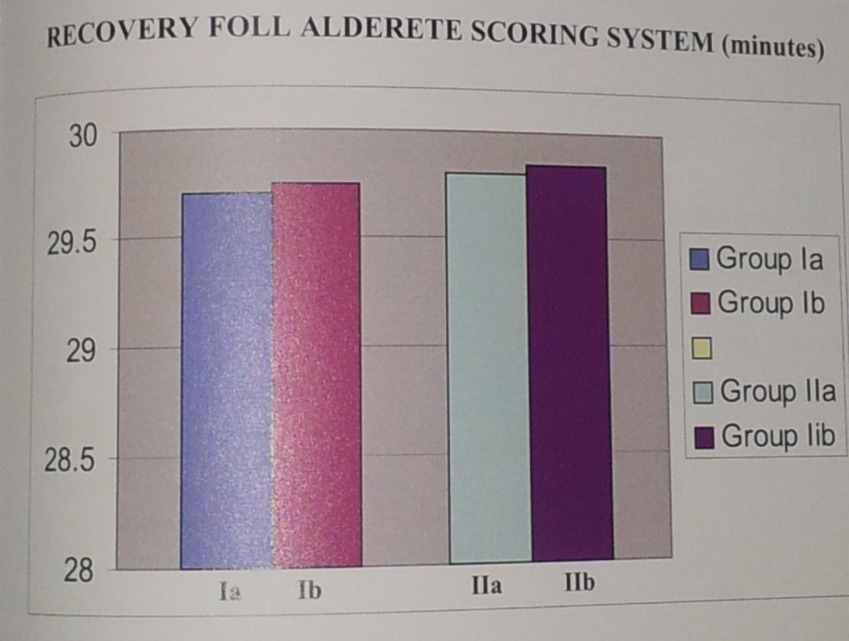
We recoded, time when patient was able to open eyes, follow commands and be oriented with respect to their name, place and date of birth. Times to sit, stand up, tolerate oral fluids and ambulate without assistance were recorded. Duration of time of stay in recovery room and actual time to discharge were recorded. Recovery was also assessed at 10 minutes interval using Modified Alderete Score. Early Recovery Phase I commence on discontinuation of the anesthetic agent, which allows the patient to awaken, recover protective airway reflexes and resume motor activity. Phase II recovery occurs before discharge, which makes able to tolerate orally, to void, to sit, to walk Modified Alderete Scoring System [MASS] is used to decide, when patients are ready for discharge from the post anesthesia care unit. Phase III recovery occurs after discharge and continues till patient resumes every day activities.
4 P a g e Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
A Total Score of 10 according to MASS indicates that the patient is in optimal condition.
DATA RELATED TO RECOVERY
Table: 3 Data related to recovery
Eye opening 5.65*1.17
Time to sit up 14.52*2.13
Time to stand 27.35*4.96
When a patient had no excessive pain or no vomiting and was able to walk unaided, he she can be discharged with a escorts.All patients required to be accompanied home with a responsible adult and who could stay with him for a minimum of 24 hours post discharge. Each patient was provided with a contact number where he remains with a health care provider in case of any difficulty. Side effects e.g.vomiting and pain were recorded. The Severity of emesis was assessed, based on a 4-point scale suggested by Belville et al to determine the emesis score in the following manner [5].O- No nausea or vomiting, 1- Nausea alone, 2- Vomiting once, 3- Vomiting > 3 times.In our study1 patient in-group Ib and 3 patients' in-group II b had nausea of which one has vomiting also. It was corrected with injection Ondansetron 4 mg intravenously.Pain was assessed with using a 10 cm Visual Analog pain Scale (VAS) where in scoring of pain from 0 to 10 was done with markings, corresponding to 0-no pain, 10 worst imaginable pain and with 1 to 3 implying mild pain 4 to 6 implying moderate pain and 7 to 10 implying severe pain.Postoperative pain was treated with injection Tramadol 50 mg intravenously.
5 P a g e Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
Figure: 3 Recovery foll alderete scoring system
DISCUSSION
Paulin et al reported that GA with newer anesthetic drugs allowed an earlier discharge as compared with spinal or epidural anesthesia in newer practice [184 vs. 202 min for males] and [185 vs. 213 min} [6].
The introduction of rapid ultra short acting anesthetic agents like Propofol, Isoflurane and Sevoflurane and Fentanyl achieve a recovery profile that facilitates fact tracking after GA, Isoflurane is another anesthetic agent, which is popular for day care anesthesia, as it is also known to have a short recovery time [7]. It has been used for conscious sedation in outpatient dental surgery, when patients were street fit within 10 min after anesthesia [8]. But study by Kortill K. Ostman P in 1990 has shown that recovery was quicker following propofol as compared to Isoflurane anesthesia. [9].
Total intravenous anesthesia reduced the absolute incidence of postoperative nausea and vomiting up to 72 hr by 15% in patients and by 18% in outpatients. This effect was most pronounced in the early postoperative period. The cost of anesthesia was more than three times greater for Propofol TIVA but TIVA could be cost effective because the costs of treating PONV and increased recovery room stay after inhalational anesthesia offset the additional drug acquisition costs of Propofol TIVA [8]. So we used Propofol for induction in both the groups and for maintenance in one group, as it has favorable pharmacokinetic, Pharmachodynamic and antiemetic properties as we have discussed earlier for day care surgery. [10-13]
As Propofol does not have any analgesic property, so we have used Propofol and Fentanyl combination in low doses for balanced anesthesia [14,18]
For intra-operative pain relief, we use intravenous aqueous preparation of Voveran and Fentanyl in all patients. The VAS scores for pain, sleepiness anxiety and co-ordination were not affected by our anesthetic techniques.No difference in the analgesic requirement was found in the postoperative period.
Canosen described, effectiveness of Ondansetron in the prevention of postoperative vomiting is not affected by the patient's past history of PONV. [15]
6 P a g e Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
Sadhasivam et al reported that prophylactic use of Ondansetron 75 mcg / kg reduces the incidence of PONV from 80% to 30% and improves true outcomes after strabismus repair in children [16].
In our study, no patient felt nausea & vomiting. In subgroups which received two antiemetic drugs. But in group Ib, only I patient and 3 patients in group II b had nausea which was treated with intravenous Ondansetron 4mg, where we used Isoflurane for maintenance, no antiemetic drug was used in this subgroup. It has shown that after general anesthesia PONV is common, which is manifested when we did not use any antiemetic drug.
We used modified ALDERETE scoring system to asses the recovery from the PACU to the home, as in our hospital we have only one O.T recovery room so we kept patient there till we get score of 9 according to this system. This criteria do little to test higher level of function such as the ability to use one's hands, do drive car or to remain alert for long enough to drive So we had to keep patient in our recovery room till they become fully awake, obeying commands, haemodynamically stable without pain, nausea and vomiting [phase I and phase II recovery]. This was noted as actual discharge time or time to be ‘street fit'One person should accompany the patient for24 hours,even in the home. Phase III recovery occurs after discharge and continues until the patient has resumed usual everyday activities [17]. The 24 hrs follow up telephone interviews revealed no difference in the incidence of nausea, vomiting, coughing and dizziness in all the groups.
1. Day care surgery is an upcoming branch of anesthesia. 2. PONV is a common problem causing delay in discharge. 3. Short and nonemetogenic procedures can be done without antiemetic drugs especially if we are using technique, which we have used in Group I.
REFERENCE
1. Janet M. Van Vlyment, while P, F- Outpatient Anesthesia In: Anesthesia 5th edition, Miller RD (ed) chapt: 65, pp 2213-2240 2. Morton HJV, Wylie WD (1951) Anesthesia deaths due to regurgitation or vomiting Anesthesia 6, 190-205 3. Smith GFR (1934) Postoperative vomiting Br J. Anesth. 11,132-39 4. S K, ambulatory anesthesia and surgery in America. A historical background and recent innovation J Peri anesthesia 1999, 14(5) 270-4 5. Bellvielle J W Brors IDJ, Holland W S. (1959) A method for the clinical evaluation of antiemetic agents, Anesthesiology 20, 735-60. 6. D Janet Pavlin factors affecting discharge time in adult out patient Anesth. Analg. 1998, 87: 816-26. 7. Korttila K, Valanne J. Recovery after outpatient Isoflurane and Enflurane anesthesia. Anesth Analg 1985:64:239
8. Randomized controlled Trial of Total Intravenous Anesthesia with Propofol versus Inhalation Anesthesia with Isoflurane- Nitrous oxide- Visser hassink Anesthesiology 2001 V 95 No3, Sep 2001 616-626
9. Kortlilak, Ostman P. Faure et al Randomized comparison of recovery after Propofol Nitrous oxide anesthesia in patients. Undergoing ambulatory surgery. Acta Anaesthsiol Scand 1990:34:400-903
7 P a g e Available online on www.ajpms.com Original Research Article
Asian Journal of Pharmacy and Medical Science Vol. 3 (1),April,2013 ISSN 2278-0017
10. Rolly G, Versichelen L. Comparison of Propofol and Thiopentone for induction of anesthesia in premedicated patient. Anesthesia 1985:40:945-48 11. Price ML, Comparison of Total intravenous anesthetic technique using Propofol of infusion with an inhalation technique using Enflurane for daycare surgery. 12. Mc Collum JSC, Milligan K. R, Dundee JW, The Antiemetic action of Propofol Anesthesia 1988:43:239-240 13. Van A, Doze BS, Shafer A, White P, Propofol- Nitrous oxide versus Thiopentone- Isoflurane Nitrous oxide for general anesthesia Anesthesiology 1988:69:63-71 14. A comparison b/t TIVA using Propofol Alfentanil mixture with an inhalational technique in laproscopic gynecologic sterilization E J Anesthesilolgy 1996: 13, 33-37 15. Canosa-ProphylacticOndansetron for postoperative emesis Acta Anaesthesiology Scandanavia1999,43
16. Sadasivam S et al- Safety and efficacy of prophylactic Ondansetron in patients undergoing redical mastectomy Anesth Analg 1999, 89. 1340-6
17. Paul F white and Dajun Song- New Criteria for fast tracking after outpatient Anesthesia- A Comparison with the modified Alderete Scoring System.Miller,s 6th edition 1894-1899
18. Comparison of 2 drug combinations in TIVA:Propofol-Ketamine and Propofol-Fentanyl .Saudi J Anaes 2010May-Aug 4(2):72-74
8 P a g e Available online on www.ajpms.com Original Research Article
Source: http://ajpms.org/admin/Issues/PIssue20.pdf
RESEARCH PACKET Rev. 1.4 June 2007 Table of Contents Corporate Philosophy.3 Our Mission.3 Research Philosophy.3 Commitment to Quality .3 Certificate of Analysis .3 Safe and Legal.4 About PreRace Pre-Exercise Supplement .5 Physiological Adaptations .5 Biochemical Processes.5
Security Mechanisms and Policy for Mandatory Access Control in Glenn Daniel Wurster A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfilment of the requirements for the degree of DOCTOR OF PHILOSOPHY Carleton University Ottawa, Ontario, Canada ©2010, Glenn Daniel Wurster Computer security measures, policies and mechanisms generally fail if they arenot understood and accepted by all parties involved. To be understood, manysecurity mechanisms currently proposed require security expertise by multipleparties, including application developers and end-users. Unfortunately, bothgroups often lack such knowledge, typically using computers for tasks in whichsecurity is viewed at best as a tertiary goal. The challenge, therefore, is todevelop security measures understood and accepted by non-experts.