Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Caymanprepared.ky
Influenza Pandemic
Ten Things You Need To Know About Pandemic Influenza
1. Pandemic influenza is different
5. Widespread illness will occur
from avian influenza
Because most people will have no immunity to the
Avian influenza refers to a large group of different
pandemic virus, infection and illness rates are expected to
influenza viruses that primarily affect birds. On rare
be higher than during seasonal epidemics of normal
occasions, these bird viruses can infect other species,
including pigs and humans. An influenza pandemic
happens when
a new subtype emerges that has not
It is estimated that about 25% of the population would be
previously circulated in humans. Avian H5N1 is currently
affected. This amounts to almost 13,000 persons in the
circulating in Asia and Europe. It is a strain with pandemic
Cayman Islands.
potential, because of the fact that it might adapt into a strain
that is may be passed from human to human. If this
6. Medical supplies will be inadequate
adaptation occurs, it will no longer be a bird virus--it will be
Supplies of vaccines and antiviral drugs – the two most
a human influenza virus.
important medical interventions for reducing illness and
deaths during a pandemic-will be inadequate in all
Influenza pandemics are recurring
countries at the start of a pandemic and for many months
thereafter. The Cayman Islands Government is working
An influenza pandemic is a rare but recurrent event. Three
with the United Kingdom and PAHO to ensure adequate
pandemics occurred in the previous century: "Spanish
supplies. Priority will be given to high risk populations.
influenza" in 1918, "Asian influenza" in 1957, and "Hong
Kong influenza" in 1968. The 1918 pandemic killed an
7. Large numbers of deaths will occur
estimated 40–50 million people worldwide. Subsequent
pandemics were much milder, with an estimated 2 million
Death rates are largely determined by four factors: the
deaths in 1957 and 1 million deaths in 1968.
number of people who become infected, the virulence of the
virus, the underlying characteristics and vulnerability of
The world may be on the brink of
affected populations, and the effectiveness of preventive
measures. WHO has used a relatively conservative estimate –
The H5N1 strain first infected humans in Hong Kong in
from 2 million to 7.4 million deaths globally – based on the
1997, producing 18 cases, including six deaths. Since
comparatively mild 1957 pandemic.
mid-2003, this virus has caused 327 human cases (as of
August 31, 2007) that have have been confirmed in twelve
Economic and social disruption will
countries (Azerbaijan, Cambodia, China, Djibouti, Egypt,
Indonesia, Iraq, Lao People's Democratic Republic,
High rates of illness and worker absenteeism are expected,
Nigeria, Thailand, Turkey, and Viet Nam), and more than
and these will contribute to social and economic disruption.
half of these people have died. Should H5N1 evolve to a
Social disruption may be greatest if rates of absenteeism
form as contagious as normal influenza, a pandemic could
impair essential services, such as power, transportation, and
begin. The risk of H5N1 infection among birds in the
Cayman Islands is very remote. The Department of
Agriculture does not allow importation of poulty or poulty
Every country must be prepared
products from countries affected with Avian Influenza. The
WHO has issued a series of recommended strategic actions
Department of Agriculture is also monitoring the
for responding to an influenza pandemic threat. The
importation of any exotic birds, and is strictly enforcing the
Cayman Islands Influenza Pandemic Contingency Plan
necessary quarantine requirements.
describes the proposed actions to be taken at various phases
of the pandemic.
4. All countries will be affected
10. WHO will alert the world when
Once a fully contagious virus emerges, its global spread is
considered inevitable. Given the speed and volume of
the pandemic threat increases
international travel today, the virus could spread more
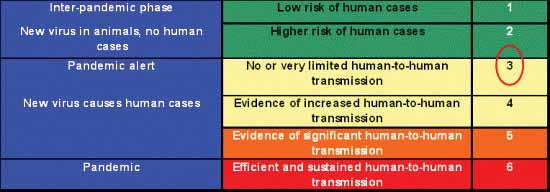
Six distinct phases have been defined to facilitate pandemic
rapidly, possibly reaching all continents in less than three
preparedness planning, with roles defined for governments,
months. The Cayman Islands will not be spared due to the
industry, and WHO. The present situation is categorized as
active tourism industry and frequent travel by residents.
phase 3: a virus new to humans is causing infections, but
does not spread easily from one person to another.
HE HATH FOUNDED IT UPON THE SEAS
HE HATH FOUNDED IT UPON THE SEAS
Influenza Pandemic
Contingency Plan
First draft of this Plan was approved by Cabinet in December, 2006.
Revision approved by Cabinet in September, 2007.
For further information please contact:
Dr. Kiran Kumar Alla
Medical Officer of Health
Public Health Department
Cayman Islands Hospital
PO Box 915
Grand Cayman KY1-1103
Tel: 244 2621
Fax: 945 2153
Printing sponsored by
Sagicor General Insurance (Cayman) Ltd
Harbour Place, 3rd Floor
Grand Cayman KY1-1105
Tel: 345-949-7028 Fax: 345-949-7457
Email:
[email protected]
2. Aim and Objectives
2.1 Objectives2.2 Principles Underlying The Response
3. The Phases Of An Influenza Pandemic
3.1 International Phases3.2 Transition Between Phases3.3 Implications For The Cayman Islands3.4 Mechanism For Declaring A Pandemic
4. Impact Of An Influenza Pandemic
4.1 Planning Assumptions4.2 The Extent To Which Interventions Might Lesson The Impact
5. The Plan: Key Elements
5.1 Organization and Coordination5.2 Communications
- Strategic and Operational Communications and Advice- Professional Information and Guidance- Communications With The Public and The Media
5.3 Surveillance5.4 The Public Health Response: Measures To Reduce The Health
Impact- Immunization Strategy- Antiviral Agents and Their Use
- Other Public Health Control Measures
5.5 The Health Service Response
- Investigation and Management of Cases and Contacts- Infection Control- Organization and Reinforcement of Health Services
5.6 The Civil Contingency Response: Reducing Societal Disruption5.7 Workforce Education and Training5.8 International Issues
6. Roles and Responsibilities
6.1 Organizational Structure6.2 Cayman Islands National Influenza Pandemic Committee
6.3 Cayman Islands National Influenza Pandemic Health Task
6.4 Ministry of Health6.5 Hazard Management Cayman Islands (HMCI)6.6 Government Information Services (GIS)6.7 Public Health Department6.8 Health Services Authority (HSA)6.9 Other Governmental Departments6.10 Private Health Care Providers6.11 Other Organizations
7. Phase By Phase Action
(a) The Inter-Pandemic Period – Phases 1 and 2:
- Phase 1: No New Influenza Virus Subtypes Detected in
- Phase 2: No New Influenza Virus Subtype Detected in
Humans. Circulating Animal Influenza Virus Subtype Poses Substantial Risk of Human Disease
(b) The Pandemic Alert Period – Phase 3:
- Phase 3: Human Infection(s) With A New Subtype, But No
Human-to-Human Spread
(c) The Pandemic Alert Period – Phases 4 and 5
- Phase 4: Small Cluster(s) With Limited Human-to-Human
- Phase 5: Large Clusters(s) But Human-to-Human Spread
(d) The Pandemic Period – Phase 6:
- Phase 6: Increased and Sustained Transmission in General
(e) The Post-Pandemic Period
Appendix I
(A) Disaster Risk Management Structure(B) The Cayman Islands National Influenza Pandemic Committee(C) The Cayman Islands National Influenza Pandemic Health Task Force
Appendix II
Business Contingency Planning Guidance
Appendix III
Sources of Guidance
The possibility of an influenza pandemic is a significant challenge facing the
world, one which must not only be contemplated but prepared for. A pandemic
is the worldwide spread of a disease, with outbreaks or epidemics occurring in
many countries and most, if not all, regions of the world.
Influenza is an acute viral infection, characterized by the sudden onset of
fever, chills, headache, aching muscles, prostration and a cough, with or
without a sore throat or other respiratory symptoms. The acute symptoms last
about a week but a full recovery may take longer. Influenza can spread rapidly
from person to person, via droplets and fine aerosols of infected respiratory
secretions. Influenza has an incubation period of one to three days.
Seasonal outbreaks are caused by subtypes of influenza viruses that already
circulate among people worldwide. In the Cayman Islands, it usually occurs
during the cooler months of December to March.
There are three (3) types of influenza, identified as type A, B, and C. Types A
and B are known to affect humans.
• The three (3) Type A viruses, which commonly cause epidemics in
humans, are known as H1N1, H1N2 and H3N2. Type A viruses are
divided into subtypes on the basis of the proteins attached to the surface
of the virus.
• Influenza A (H5N1) is the subtype, which is causing the current outbreak
of Avian Flu in Asia.
• Type B viruses are also known to cause epidemics among humans.
• Type C viruses are milder and do not cause epidemics.
Over the last hundred years there have been three (3) major influenza
pandemics. These were:
• the 1918-19, "Spanish Flu" Type A (H1N1) where an estimated 20 to
50 million deaths occurred worldwide;
• the 1957-1958 "Asian Flu" Type A (H2N2) causing about 70,000 deaths
in the United States alone; and
• the 1968-69 "Hong Kong Flu" Type A (H3N2), which caused about
34,000 deaths in the United States and is still in circulation today.
An influenza pandemic results when a new influenza virus emerges which is
markedly different from recently circulating strains and is able to:
• infect people (rather than, or in addition to, other mammals or birds);
• spread readily from person to person;
• cause illness in a high proportion of the people infected; and
• spread widely, because most people will have little or no immunity to
the new virus and will therefore be susceptible to infection.
Avian viruses played a role in the past three influenza pandemics. The current
pandemic threat emanates from an unprecedented outbreak of avian influenza
in Asia and Europe, caused by the H5N1 strain of the Influenza A virus. To
date, the virus has infected birds in 64 countries. While traditional control
measures have been attempted, the virus is now endemic in Southeast Asia,
present in long-range migratory birds, and unlikely to be eradicated soon.
A notable and worrisome feature of the H5N1 virus is its ability to infect a
wide range of hosts, including birds and humans. As of August 31st 2007 the
virus is known to have infected 327 people in 12 countries, resulting in 199
deaths over the past four years. Although the virus has not yet shown an ability
to transmit effectively between humans, as is seen with the annual influenza
viruses, there is concern that it will eventually acquire this capability through
genetic mutation with a human influenza virus.
It is impossible to know at this stage whether the currently circulating H5N1
virus will cause a human pandemic. Although it has been transmitted from birds
to humans, the rapid spread from human to human has not hitherto happened;
the potential, however, is there. If this does not occur with the current H5N1
strain, history suggests that a different influenza virus will emerge and result
in the next pandemic.
It is the opinion of scientists worldwide that there will at some point be another
severe influenza pandemic; the question is when. Introduction of Avian
Influenza in the Cayman Islands bird population through migratory birds or
importation of infected birds and its transmission to humans and the initiation
of a pandemic is, it might be argued, a remote possibility. However, should the
flu pandemic start, most likely in Asia, the Cayman Islands, being a popular
tourist destination in these days of rapid international travel, it is inevitable
that we will be affected.
The timing, extent and severity of a future pandemic remain uncertain, but
experience from previous pandemics suggests that it will spread rapidly to all
parts of the globe causing sudden, sharp increases in illness and deaths over
a matter of weeks. It could rapidly overwhelm health and other services, and
have far reaching effects on daily life, businesses and, consequently, national
and global economies.
In the event of a pandemic, the rapid transmissibility of influenza viruses,
the universal susceptibility of the world's population to viruses that have not
previously circulated, and the mobility of human populations mean that every
corner of the globe and every element of society are likely to be touched.
This has ramifications for not only the health and wellbeing of populations,
but for the national and economic security of nations, and the functioning of
civil societies. The scope and scale of the measures necessary to prepare for
a pandemic are wide ranging.
Advance planning is essential, to establish – and rehearse – contingency
arrangements, and identify and address gaps in our preparedness, so that we
are in the best possible position to manage an emergency on such a scale
and lesson its impact. Disruption is likely to be less if people know what to
expect and what to do and have had time to think through the consequences
for themselves, their families, communities and organizations.
This Plan builds on previous experience of managing events such as the
outbreak of severe acute respiratory syndrome (SARS) in 2003 and takes
into account 2005 World Health Organisation's (WHO) guidance (including a
recently revised phasing system) and the National Plans of the United Kingdom
and the United States of America. The Plan is based on three main elements:
• preparedness and communication;• surveillance and detection; and• response and containment.
It recognises the importance, when responding to a new event, of basing plans
on existing systems and infrastructures with which people are familiar, such
as the current national infrastructure for the prevention and control of seasonal
influenza, and plans and organisational arrangements for other outbreaks and
Not least among the uncertainties of a flu pandemic will be our ability to
reduce its impact through medical countermeasures such as vaccination and
the use of antiviral drugs. The normal annual influenza vaccine will not protect
against a pandemic strain and a specific vaccine will need to be developed and
manufactured. The Government is planning to build a stockpile of antiviral
drugs to treat the anticipated number of people with influenza during a
pandemic. The stockpiling of these drugs will be based on WHO advice about
the likely attack rate and that of the UK proposals but it will not be known
until the time how effective these drugs will be.
An influenza pandemic, or the threat of one, will create a high demand for
information and advice from health professionals, businesses and organisations,
the general public and the media, about the threat and the responses to it. Rapid
and effective communication, making difficult policy decisions transparent
and managing people's concerns are an integral part of the Plan.
This Plan concentrates on the national response and provides the framework
and information for all organisations involved in preparing for and responding
to an influenza pandemic. It identifies actions to be taken at each phase of the
pandemic as defined by WHO, with clear modifications to adapt the WHO
phases to the local situation.
The Plan is also intended to be flexible so that our response can be adapted
as a pandemic evolves and knowledge about the new virus, its impact and the
effectiveness of available counter-measures, emerges.
Improving our preparedness is a continuous activity and this Plan will continue
to be reviewed and updated, in particular to take account of new advice from
the WHO relevant to national plans.
2. Aim and Objectives
This document aims to provide a national framework for an integrated national
response to an influenza pandemic, with guidance for developing detailed
operational plans for response at all levels. The response is based on phases,
defined by the WHO in 2005, which trigger escalating public health action,
starting with plans which need to be put in place, and tested, during the inter-
pandemic and pandemic alert period. An inter-agency response is indicated
and the roles of relevant organisations and their lines of communication are
2.1 Objectives
The specific objectives of contingency planning for an influenza pandemic are
• set up a system for a flexible response to unpredictable events;
• recognise a new strain of influenza virus with pandemic potential and
clinical illness caused by it;
• minimise the spread of the new virus and if possible prevent a pandemic
• limit morbidity and mortality due to infection with the pandemic
• provide treatment and care for large numbers of people ill from influenza
and its complications;
• cope with the eventuality of large numbers of people dying;
• reduce the impact on health and social services consequent to an
influenza pandemic, including any consequences for other patients as a
result of re-prioritisation of services or cancellation of routine work;
• provide timely, authoritative and up to date information for professionals,
the public and the media throughout the period of a potential or actual
• ensure that essential services are maintained;
• reduce the impact on daily life and business;
• anticipate and plan for other consequences; and
• minimize economic loss.
Even if all these objectives are achieved, the consequences of an influenza
pandemic are likely to be serious.
2.2 Principles Underlying the Response
The following principles underlie this contingency planning:
• the priority in an influenza pandemic is to reduce the impact on public
health (i.e. reduce illness and save lives). Interventions will therefore
be applied where they will achieve maximum health benefit. However,
they may also be needed to help maintain essential services. Should
there be a conflict between these two aims, decisions made at Cabinet
level will need to be made about prioritizing these interventions.
• with or without medical interventions to protect or treat large numbers
of the population, measures aimed at slowing the spread of a pandemic
may buy valuable time, and help services to cope, even if this prolongs
the overall duration of the pandemic.
• the response to pandemic influenza in the Cayman Islands will require
collaboration between the Ministry of Health, the Health Services
Authority (HSA) and many government departments together with the
private sector, non-governmental organizations, and the community at
The Phases of an Influenza Pandemic
The World Health Organization (WHO) has defined phases in the evolution
of an influenza pandemic which allow a step-wise escalating approach to
preparedness planning and response leading up to a declaration of the onset
of a pandemic. Once a pandemic has been declared, action in the Cayman
Islands will depend on whether cases have been identified locally, and, if so,
how extensively the disease has spread.
3.1 International phases
The WHO phases, which were revised in April 2005, describe the progression
of an influenza pandemic from the first emergence of a new influenza virus
to wide international occurrence. This is a global classification based on the
overall international situation and is now used internationally for planning
No new influenza virus subtypes have been detected in
humans. An influenza virus subtype that has caused human
infection may be present in animals. If present in animals,
the risk of human infection or disease is considered to be
No new influenza virus subtypes have been detected in
humans. However, a circulating animal influenza virus
subtype poses a substantial risk of human disease.
Pandemic Alert Period
Human infection(s) with a new subtype, but no new human-
to-human spread or, at most, rare instances of spread to a
close contact.
Small cluster(s) with limited human-to-human transmission
but the spread is highly localised, suggesting that the virus
is not well adapted to humans.
Large cluster(s) but human-to-human spread is still localised,
suggesting that the virus is becoming increasingly better
adapted to humans, but may not yet be fully transmissible
(substantial pandemic risk).
Pandemic phase: increased and sustained transmission in
the general population.
Past experience suggests that a second wave, and possibly
more, of illness caused by the new virus is likely 3 – 9
months after the first wave has subsided. The second wave
may be as intense as the first or even more so.
Return to inter-pandemic period.
3.2 Transition between phases
Transition between phases may be rapid and the distinction blurred. The
crucial interval is between WHO Phases 5 and 6, which will determine to
a large extent whether vaccine can be available in time for the first wave of
illness in the Cayman Islands.
3.3 Implications for the Cayman Islands
The WHO Plan recognizes additional national subdivisions for Phase 2
onwards according to whether a country is affected itself, has extensive travel/
trade links with an affected country, or is not affected.
For our purposes, should we have cases during the pre-pandemic period (Phase
1-5), the international phases apply. Once a pandemic has been declared
(Phase 6), two stages of phase 6 are included for the Cayman Islands.
Cases only outside the Cayman Islands.
Pandemic cases identified in the Cayman Islands.
3.4 Mechanism for declaring a pandemic
The WHO will announce the various phases as soon as they are confirmed,
indicating the level of preparedness expected of WHO and its individual
Member States.
We in the Cayman Islands are expected to be prepared to activate our
national contingency plans following announcement of WHO Phase 5 (the
highest pandemic alert level). Before announcing this phase, WHO will have
consulted international experts to rule out other possible explanations, such as
WHO will normally consult internationally before confirming Phase 6, i.e. the
onset of a pandemic.
Action in the Cayman Islands
On being informed by WHO of the isolation of a new influenza virus with
pandemic potential (normally when person to person spread has been
confirmed, i.e. Phase 5), the Honourable Minister for Health will convene the
Cayman Islands National Influenza Health Task Force (CINIHTF) to ensure
the health services preparation and His Excellency the Governor will convene
the Cayman Islands National Influenza Pandemic Committee (CINIPC) to
review the preparedness of all sections.
On receipt of confirmation from WHO of the onset of a likely pandemic, i.e.
Phase 6, the Ministry of Health will immediately cascade this information to
the HSA, other Government Departments and Agencies, and other relevant
services and agencies. The CINIPC will be convened and the Hazard
Management Cayman Islands (HMCI) will coordinate the command and
control activities, with the Medical Officer of Health coordinating the health
services response.
Impact of an Influenza Pandemic
An influenza pandemic is thought most likely to emerge from Southeast
Asia, but could start anywhere in the world. For planning purposes, working
estimates of the most likely subsequent spread and impact have been derived
from theoretical modeling, informed by past experience, knowledge of the
world today and expert advice. Once established, a pandemic is likely to
spread to the Cayman Islands in 1 – 2 months, and in almost 2 – 3 weeks, it
could have spread through the three islands. Thereafter, activity could last 3 –
5 months, with a peak of cases at about week 6. Subsequent waves are likely
to occur weeks to months later. The illness is likely to affect more people and
cause more severe illness than the annual ‘seasonal' influenza which occurs in
the winter months: about a quarter of the population may have developed the
illness, with 11 – 50 deaths or more, by the end of the pandemic. Estimates for
the demand on health care are provided in this document. Timely information
about an actual pandemic, once it emerges, will be essential to provide more
accurate predictions.
In past pandemics, the scale and severity of illness, and hence the consequences,
have varied considerably but in general they have been of much greater
magnitude than even the most severe ‘epidemic' winters. There have also been
material differences in the age groups most affected (for example, working
age adults rather than the elderly), the time of year of outbreaks and the speed
of spread, all of which influence the overall impact.
Despite their variability and unpredictability, much can be learned from
previous pandemics. On the other hand, much has also changed in the world
since the last pandemic in 1968, including:
• the demography of the population (a greater proportion of elderly
• health care opportunities and expectations;
• the greater emergence of antimicrobial resistance among the bacteria
which may cause infections such as pneumonia following influenza;
• the extent of ‘surge' capacity in health care systems.
In the case of a new pandemic influenza virus there are few data and a wide
range in the plausible assumptions that can be made.
The main role of modeling in advance of a pandemic is to map out the range
of possible risks and to investigate which responses are likely to be robust
notwithstanding the uncertainty resulting from lack of data.
The modeling methodology undertaken in the UK is utilized in the calculations
in this document of the impact of an influenza pandemic in the Cayman
4.1 Planning Assumptions
Plans presented in this document concentrate on a ‘most likely' base scenario
following WHO advice and the UK proposals. These are working estimates
for planning purposes, and not predictions of the next pandemic. Generally it
• the emergence of new Influenza A viruses is inevitable;
• a new pandemic will be due to a new subtype of influenza A;
• a potential pandemic or pandemic strain could first emerge anywhere,
but is most likely to emerge in Asia;
• in the event of a new influenza virus causing significant outbreaks of
human illness elsewhere in the world, it is unlikely that the Cayman
Islands could prevent importation (except by closing all borders which
is not practical); even a 99.9% restriction of travel into the country
would only be expected to delay importation of the virus by up to two
• following arrival in the Cayman Islands it will take a further 2 – 3
weeks for cases to occur across Grand Cayman and the Sister Islands.
More specific assumptions are set out in (a) to (g) below.
(
a) Duration and Extent of Infection
• The incubation period is 1 – 3 days. On an average, an infected person
will transmit infection to approximately two other people.
• Most people will be susceptible, although not all will necessarily
develop clinical illness. Previous experience suggests that roughly
equal numbers will have asymptomatic infection as have symptomatic
• For planning purposes, the base scenario, based on previous pandemics
in the 20th century, is a cumulative clinical attack rate of 25% of the
population over one or more waves of around 15 weeks each, weeks or
months apart.
• This compares with a usual seasonal influenza attack rate of 5 – 10 %.
The second wave may be the more severe. A total cumulative attack
rate over a number of waves is unlikely to exceed 50%.
• All ages will be affected, but children and otherwise fit adults could be
at relatively greater risk, since elderly people may have some residual
immunity resulting from exposure to a similar virus earlier in their
lifetime. For illustrative purposes, a uniform attack rate has been used
across all age groups as in the UK plan.
• It is estimated that 13,000 persons may be ill with influenza of which
6,500 might seek health care contact. Hospitalizations may vary
between 40–176 and there might be 11–50 deaths during the pandemic,
depending on the severity.
• The impact of a flu pandemic on health and human services is likely
to be intense, sustained and nationwide and the relevant entities may
quickly become overwhelmed as a result of:
Ø the increased workload of patients with influenza and its direct
Ø the particular needs for high dependency care and infection
control facilities and equipment;
Ø a secondary burden on health caused by anxiety and
Ø depletion of the workforce and of numbers of informal carers,
due to the direct or indirect effects of flu on themselves and their
Ø logistical problems due to possible disruption of supplies, utilities
and transport as part of the general disruption caused by the
Ø delays in dealing with other medical conditions; and
Ø the longer term macro effects of the pandemic on the national
(and world) economy.
• Innovative approaches to many aspects of health care will be needed,
including staffing, triaging of patients and coping with those patients
needing more intense care than is normally possible at home but who
may not be able to be admitted to hospital.
• There will be pressure on mortuary facilities (possibly exacerbated by
delays in death registrations and funerals).
(c) Absence From Work
• Absence from work will depend on the age-specific attack rate, although
even if working age people are relatively spared, additional absenteeism
may result from staff needing to take time off to care for family members
or difficulties with transport.
• Accelerated transmission may occur in the workplace, resulting in staff
being ill during a more concentrated timeframe than in the general
• It is suggested that business continuity plans should be based on a
cumulative total of 25% of workers taking some time off – possibly 5 –
8 working days – over a period of 3 to 4 months.
• In the absence of vaccination, those in occupations with particularly high
exposure such as health care workers will have higher absenteeism.
• The skill mix required in some occupations, including health care, may
limit the extent to which other staff can be redeployed.
(d) Schools and Other Closed Communities
• Influenza will spread rapidly in schools. 50% of schoolchildren may be
• However, closing schools has a significant impact on business continuity
and maintenance of essential services, particularly health care, due to
working parents needing to stay at home to provide childcare.
• A similar spread is likely in other closed communities such as residential
care facilities and prisons.
(e) Impact On Other Services
• In the absence of early or effective interventions, there will be an effect
on all other services, through staff sickness, any travel restrictions
imposed and also through the knock-on effects of other disrupted
businesses and services.
• This includes all non-health ‘first responder' services (police, fire etc)
the Civil Service and other essential services (e.g. utilities, fuel supply,
food production and distribution, transport).
• Services such as death registration and funeral homes will have an
increased work load.
• In addition to maintaining continuity of their work, badly affected
businesses will need to consider additional factors, for example, the
security of their premises.
(f) Impact On Travel
• Travel will be impacted through:
Ø any explicit advice or restrictions on travel and public gatherings
adopted as a policy option;
Ø people opting not to travel (e.g. because of cancellation of work/
school etc, fear of acquiring infection through travel or fear of
leaving home); and
Ø availability of fuel and transport workers.
(
g) Public, Political and Media Concern
• There will be high public and political concern and scrutiny at all stages
of an influenza pandemic.
• The media's need for information and their coverage of all aspects of
the pandemic will be intense.
• Managing people's concerns, expectations and frustrations will be a
key part of the response.
• People's concerns will extend to what is happening in other countries,
particularly those with which they have family connections.
• Interest and concern will also extend to national and international events
and mass gatherings as these can facilitate spread due to close contact
4.2 Extent To Which Interventions Might Lessen The Impact
More detail is given in later chapters in this Plan, but in summary:
• a
vaccine specifically formulated against the pandemic virus strain
(when such a vaccine becomes available) can be expected to achieve the
greatest reduction in illness, complications and deaths, and a lessening
of the impact on health and other services, although it should be noted
the extent of the effectiveness of a pandemic vaccine will not be known
until it is in use. In inter-pandemic years, when the virus strains predicted
to be circulating the following winter are included in the vaccine and
are well matched to those which actually do occur, vaccination reduces
infection by around 70-80%, hospitalisations of high risk individuals
by around 60% and deaths by around 40%;
• much work has been done on the most effective strategies for the
use of
antiviral drugs. If treatment with antiviral drugs provides benefits of
the same order as those demonstrated during seasonal influenza, early
treatment (within 48 hours of onset of illness) should shorten illness
by around one day, reduce the severity of the symptoms, and reduce
the need for hospitalisation. If, as planned, it is possible to treat all
those with clinical symptoms, there should be a reduction in the total
numbers affected, the number of hospitalisations needed (by around
50%) and those dying from the disease. However, the effectiveness of
antivirals in a pandemic, and particularly in reducing mortality in cases
of severe disease (including primary viral pneumonia), is not known at
this point in time. Predicting precisely how large these effects would be
is impossible with current information;
• the amount of antiviral drug required if it were to be taken as a
preventative measure over the entire pandemic period is prohibitive
and a treatment strategy is the only realistic option, other than in some
very specific circumstances (such as nursing homes); and
• international travel restrictions and screening passengers on entry to the
Cayman Islands would only have a very limited impact on delaying the
arrival of pandemic influenza in the Cayman Islands and is not feasible.
Travel advisories, however, can and should be given.
5. The Plan - Key Elements
The contingency plan is built around key elements such as:
• organization and co-ordination;
• professional and public communications;
• surveillance;
• public health response through vaccination, antiviral agents and their
use and other public health control measures;
• health service response by investigation and management of cases and
contacts, infection control & organisation and reinforcement of health
• the civil contingency response: to minimize societal disruption.
One of the major challenges of an influenza pandemic facing health authorities
worldwide will be to develop and manufacture a specific vaccine in the
shortest possible time and immunize whole populations. This will of necessity
take time, however, and plans are therefore based on there being no vaccine
available during the first wave. The main strategy during the first wave will be
to treat those who become ill with antiviral drugs. The Cayman Islands will
build up a stockpile of antiviral drugs for this. Other public health and ‘social
distancing' measures may be helpful in reducing the risk of infection to the
5.1 Organisation and Co-ordination
The SARS outbreaks of 2003 demonstrated the importance, of strong
international and national leadership and co-ordination, and a clear national
‘command and control' structure. The appropriate people at all levels must
have authority to make key decisions, act on them and be accountable for their
The Ministry of Health is the lead Government Agency for the planning,
initiation, direction and central coordination of the Cayman Islands Health
Response, guided by the advice of the CINIPC and the CINHTF and its
sub-committees responsible for surveillance, protection, treatment and risk
Effective communication provides the backbone for an effective and
coordinated response. The Ministry of Health will implement a comprehensive
communication strategy through Government Information Services (GIS)
with input from the risk communication sub-committee. It is recognised that
a wide range of groups at all levels will need accurate, timely and consistent
information and advice. It is also recognised that rumours and misinformation
will abound, and, inevitably, the media will sometimes report information
before it can be confirmed through official channels. This sort of situation
must be monitored closely and addressed in an effective, timely manner.
(a) Strategic and Operational Communication and Advice
• Systems are in place for communications between the main organizations
and have been, and are, tested continually in exercises. Either at Phase
5 or 6, the Ministry of Health will activate its operations room as the
hub for strategic and operational communication.
• Once a pandemic has been declared, the Government's News
Coordination Centre will be set up (coordinated by GIS) to coordinate
cross-Government briefing and public information.
(b) Professional Information and Guidance
• Regular information bulletins to health professionals will be issued as
required by the Ministry of Health via already established routes. Up to
date information will also be maintained on the HSA and Government
• Clinical guidance and public health advice will be maintained on the
HSA website, and issued directly to relevant groups as necessary.
(c) Communication With The Public and The Media
Co-ordination of media communication will be through the Government
Information Services.
Risk communication both before and during a pandemic is a key element of the
response. Emphasis in the inter-pandemic period will be on the uncertainties
surrounding a pandemic, advice on measures to reduce risk to the individual,
and the constraints faced by Governments in preparing their response. Later
communications will concentrate on what factual information people need to
have, and what action they should take. In the communication strategy clear,
active engagement of the public will be a priority throughout a pandemic by
way of, for example:
• readily accessible, easy to understand and regularly updated information
• briefing the media on the preparations and plans;
• working with the media to promulgate public health messages;
• focus groups to help identify public concerns;
• addresses to the Islands by the Honourable Minister for Health;
• press conferences;
• press releases;
• public service announcements;
• awareness meetings (schools, hospitals, businesses, associations); and
• the webpage www.caymanprepared.ky
• G.I.S. Spotlight Programme
Government will need regular, reliable and timely information on the extent
and impact of the pandemic across the whole country; public health policies
may need to change emphasis and guidance to clinicians may also need to
change. A key action in the inter-pandemic period is therefore to understand
the data requirements of the key players, so that, as far as is practicable, these
data requirements can be met should a pandemic occur.
(a) International Surveillance
Surveillance for influenza starts with good internationally coordinated
monitoring of prevalent influenza viruses worldwide and the illness caused
by them. The Medical Officer of Health keeps up to date information
through contacts with the Pan American Health Organization/ World Health
Organization (PAHO/WHO) and Caribbean Epidemiology Centre (CAREC)
(b) Cayman Islands Surveillance
Cayman Islands surveillance combines epidemiological, virological and other
data from a wide variety of sources, with the aim of:
• monitoring prevalent viruses, and the diseases caused by them;
• identifying a new virus at the earliest opportunity (including in birds or
• providing information on significant outbreaks;
• monitoring deaths; and
• monitoring the uptake and effectiveness of any interventions (including
possible adverse reactions).
It is recognised that the objectives of surveillance will change as the pandemic
evolves. The different phases will trigger enhancements – such as closer
monitoring of particular population groups, including laboratory workers – or
changes in emphasis. Flexibility will therefore be maintained in the indices
collected as the pandemic progresses.
Surveillance information, including monitoring of vaccine uptake and the
impact of interventions, will be disseminated to a wide range of stakeholders
to inform practice and planning.
In addition to addressing the information needs of key stakeholders, the
Cayman Islands plans will:
• maintain alertness among clinicians and laboratory staff to ensure that
they recognise any unusual developments. Influenza is a common
condition and has symptoms similar to those of many other viral
respiratory infections. Respiratory illness in a patient with a link to areas
where a new virus has been already identified, or to an area with poultry
farming, should be reported promptly. The Public Health Department
and the Cayman Islands Hospital Laboratory have developed a protocol
for investigating such patients;
• increase the coverage and frequency of reporting from physicians;
• establish a case based field information management system that links
epidemiological and laboratory data; and
• include monitoring of long term health sequelae of infection with a
pandemic strain of influenza virus.
The Cayman Islands Hospital Laboratory has the capability to test for Influenza
virus through Immuno Floescence. Positive samples for Influenza A virus will
be sent to CAREC and Centre for Disease Control (CDC) for further testing.
Given the large number of Influenza-Like Illnesses (ILI) (fever 38ºc, cough
and/or other respiratory symptoms) that clinicians encounter during a typical
flu season, laboratory evaluation for influenza A viruses during the Inter-
Pandemic and Pandemic Alert Periods is recommended only for:
• hospitalized patients with severe ILI, including pneumonia; and
• any severe cases attending A/E to identify if influenza is occurring and,
if so, what type.
Patients with ILI with a history of contact with a known case or coming from
a country with Avian Influenza with strong epidemiological suspicion will be
investigated for H5N1.
5.4 The Public Health Response - Measures To Reduce The Health
Public health control measures are broadly ‘medical' (vaccination, and the use
of antiviral drugs) or ‘social' (personal hygiene and ‘social distancing'), both
designed to reduce transmission or slow the spread of infection.
(a) Immunization
In inter-pandemic years, immunisation is the cornerstone of influenza
prevention. Production of an appropriate vaccine is possible each year because
of scientists' ability to predict the strains of virus most likely to be circulating
that year. These routine vaccines will not protect against a pandemic strain of
influenza. Pandemics – and the viruses causing them – are by their very nature
impossible to predict with certainty. So, although as much work as possible
will be undertaken to pave the way for production of a suitable vaccine, a
specific vaccine is unlikely to be available in any quantity at least in the early
stages of a pandemic. There will therefore be three stages in the public health
1. no vaccine available;2. vaccine in limited supply; and3. vaccine widely available.
Even when a good match is achieved between an influenza vaccine and the
prevalent circulating virus or viruses, vaccination is not 100% effective in
preventing illness and the protection afforded can vary from year to year.
There is evidence to suggest that a vaccine against a new influenza strain to
which no-one has been exposed before, requires a larger dose, or more than
one dose or a different formulation of vaccine, to achieve optimal protection.
An appropriate vaccine can be expected to reduce the impact of pandemic
influenza, particularly by reducing complications, hospitalisations and deaths
among those groups most at risk of serious illness and death.
One of the greatest challenges in responding to a pandemic will be to develop,
in the shortest possible time, a safe, immunogenic vaccine which protects
against the pandemic strain of the virus. We will not be manufacturing our
vaccine in the Cayman Islands; instead, we will use the vaccine that is approved
for use in accordance with the Health Practice Law.
The lead time before a new vaccine becomes available in sufficient quantity
is likely to be at least 4-6 months. There may be no vaccine initially and then
availability will depend on production rates. At the same time, international
demand for vaccine will be high. Vaccine will have to be distributed equitably
and administered to pre-determined priority groups first, according to nationally
agreed recommendations.
The HSA will take the lead on purchasing and supplying a pandemic vaccine
to all administering agencies. In the Cayman Islands approximately 10 percent
of the population is immunized against the seasonal influenza annually. In a
pandemic, the aim will be to obtain vaccine for a far greater proportion of the
population. In an ideal situation, the whole population should be covered as
vaccine becomes available. However it should be borne in mind that a two-
dose schedule may be required and this fact may constrain more extensive
coverage than would be ideal.
The Cayman Islands Government is working closely with PAHO/WHO, and
the UK Government to put arrangements in place to ensure an adequate supply
of vaccine for the population.
(ii) Vaccine Strategy
Immunization with appropriately formulated influenza vaccine can be expected
to reduce the impact of a pandemic, particularly among the population groups
most at risk of serious illness or death from influenza.
However, as vaccine is likely to be in short supply and demand will be high
in the Cayman Islands and worldwide, vaccine must be administered as it
becomes available to predetermined priority groups. The reasons for the
priorities must be defensible. The public will need information about this and
the reasons why the vaccine is not more generally available.
The priority groups for immunization will be based on a number of factors,
including the need:
• to maintain the elements of community infrastructure in order to carry
out the pandemic plan;
• to limit mortality among high-risk groups;
• to minimize social disruption and economic losses; and
• to reduce morbidity in the general population.
The priority groups will be subject to review, depending on the epidemiology
and clinical features of the new pandemic virus and depending on the availability
of the vaccine. It is likely that advice will be given by WHO about priority
groups for immunization, as soon as epidemiological data from the emerging
pandemic is obtained. Hence the prioritization for vaccination will be to:
• protect health care workers occupationally most at risk. Health care
workers with patient contact, in addition to being essential to the health
service response, are likely to be at increased risk of acquiring infection
from their patients and passing it on to vulnerable patients;
• prevent illness, and thus absence, among workers required to keep
essential services going. (police, firefighters, elected officials, essential
government workers, employees of utilities companies;
• prevent serious illness in the (anticipated or confirmed) most vulnerable
high risk groups;
• reduce the spread of influenza in situations where it might spread
particularly rapidly, for example in closed communities such as
residential care homes;
• reduce overall spread by immunizing those more likely to transmit the
virus, e.g. children; and
• prevent illness in the general population.
(iii) Operational Aspects of Immunization
Vaccine will be centrally purchased through the HSA Pharmacy and will be
allocated according to the estimated needs for the predetermined priority
groups. Operational details on quantities for each priority group are being
developed by the Sub-committee on Prevention.
• Public Health Nurses will play a major role in mass community
(iv) Managing Public/ Patient Expectations Regarding Vaccination
An important part of the communication strategy will be to inform the public
about the reasons for vaccine not being generally available and to manage
their expectations.
Members of the public will also need information to assist them make their
own decisions about vaccination, for example about any potential a pandemic
vaccine to cause adverse reactions.
(b) Antiviral Drugs and Their Use
Antiviral drugs active against influenza are the only other major medical
countermeasure available. They will be used in the absence of, and, once
vaccine becomes available, as an adjunct to, vaccination. However, there are
limitations to their use and their effectiveness in a pandemic situation has yet
to be tested. Antiviral resistance may also be – or may become – a problem.
Manufacture of antiviral drugs takes several months, and their availability
cannot be assured at the time of a pandemic, when international demand will
in any case be high. A stockpile of antiviral drugs (oseltamivir) is, therefore,
being built up in the Cayman Islands against the contingency of an influenza
pandemic. The stockpile, when complete, will be sufficient to treat 25% of
the population, the scenario considered most likely. However, as with other
scarce resources, the drugs will need to be given in the most effective way on
operational, clinical and cost-effectiveness grounds taking into account the
stocks available.
If treatment with antiviral drugs provides benefits of the same order as those
demonstrated during seasonal influenza, early treatment (within 48 hours of
onset of illness) should shorten illness by around one day, reduce the severity
of the symptoms, and reduce the need for hospitalisation. If, as planned, it is
possible to treat all those with clinical symptoms, there should be a reduction
in the number of hospitalisations needed (by around 50%), and deaths, and
possibly in the size of the peak and the total numbers affected. However,
their effectiveness in a pandemic, and particularly in reducing mortality in
cases of severe disease (including primary viral pneumonia), is not known.
Predicting precisely how large these effects would be is impossible with
current information.
Strategies For The Optimal Use of Antiviral Drugs
The provisional strategies proposed are:
Phase 1. No specific action required.
Phase 2. Attempted prevention of a pandemic virus from emerging. In the
event of outbreaks of highly pathogenic avian influenza in poultry, antiviral
agents will be offered to occupational groups exposed to dead or diseased
birds. This is for their personal protection, but also to protect against the
establishment and evolution of avian influenza viruses in people.
Phases 3/4. Prevention of the evolution of a new virus causing human infection.
In addition to the strategy in Phase 2, antivirals will be used to treat cases.
Phase 5 (and possibly very early in Phase 6). Possible ‘abortion' of a potential
pandemic or delay in its establishment and spread.
At this stage, this would involve treatment of a symptomatic case (or cases)
and short term prophylaxis (taken for the duration of the incubation period,
usually 7 days) to prevent infection developing in those of their close contacts
(including health care workers) who are potentially exposed to the virus. This
will be done on a case by case basis and is likely to be a short-term strategy,
and not the main use of antiviral drugs.
During inter-pandemic and pandemic alert periods. Given the large number
of influenza-like illnesses that clinicians encounter during a typical flu season,
laboratory evaluation for new influenza A viruses during the Inter-pandemic
and Pandemic Alert Periods is recommended only for:
• hospitalized patients with severe ILI, including pneumonia, who meet
the epidemiologic criteria (see below); or
• non-hospitalized patients with ILI and with strong epidemiologic
suspicion of new influenza virus exposure (e.g., direct contact with
infected poultry in an affected area, or close contact with a known or
suspected human case of new influenza.
Epidemiologic criteria for evaluation of patients with possible new influenza
focus on the risk of exposure to a new influenza with pandemic potential.
Although the incubation period for seasonal influenza ranges from 1 to 4 days,
the incubation periods for novel types of influenza are currently unknown and
might be longer. Therefore, the maximum interval between potential exposure
and symptom onset is set conservatively at 10 days.
Exposure Risks
Exposure risks fall into two categories; travel and occupational. Persons have
a travel risk if they have: 1) recently visited or lived in an area affected by
highly pathogenic avian influenza A outbreaks in domestic poultry or where
a human case of novel influenza has been confirmed, and either 2) had direct
contact with poultry, or 3) had close contact with a person with confirmed
or suspected novel influenza. Updated listings of areas affected by avian
influenza A (H5N1) and other current/recent novel strains are provided on the
websites of the OIE (http://www.oie.int/eng/en index.htm), WHO (www.who.
int/en/) and CDC (www.cdc.gov/flu).
Direct contact with poultry is defined as: 1) touching birds (apparently well,
sick, or dead) or 2) touching poultry feces or surfaces contaminated with feces,
or 3) consuming uncooked poultry products (including blood) in an affected
Close contact with a person from an infected area with confirmed or suspected
novel influenza is defined as being within 3 feet (1 meter) of that person during
their illness.
Phase 6. Treatment of Cases
This will be the main strategy once a pandemic is established. Until the full
stockpile of antiviral drugs is established, or if the clinical attack rate is greater
than the 25% planned for, treatment will be offered in provisional order of
• health care workers, if and when they develop fever or other influenza-
like symptoms (regardless of whether vaccinated);
• unimmunised people in high risk groups (or groups which emerging
information suggests are at special risk), to lessen illness and reduce
complications and death;
• other unimmunised people; and
• immunised people, using the same criteria as above, if emerging
information suggests the vaccine being used is not effective at reducing
serious illness, complications or deaths.
In certain defined situations, limited use of antiviral drugs may be recommended,
if supplies allow, limiting the spread in those situations such as, for example,
in a closed institution suffering an outbreak.
Longer term prophylaxis on a population-wide level (i.e. taking the drug to
prevent infection throughout the period of possible exposure) is not considered
likely to represent an efficient use of the drugs (bearing in mind the virus
may be circulating in the population for several weeks or months). As with
seasonal flu, it is likely that for maximum effect the drugs will need to be
started as soon as possible and within 48 hours of (for treatment) onset of
symptoms or (for post-exposure prophylaxis) exposure to infection.
Supply and Distribution of Antiviral Drugs
Antiviral drugs are being centrally purchased by the HSA and will be allocated
as the need arises.
(c) Other Public Health Measures
With or without medical countermeasures, other public health and ‘social
distancing' interventions may be helpful in reducing an individual's risk of
infection. The following public health measures are being kept under review
and infection control guidance for non-health care settings is being developed
and will be maintained on the Government website.
International Travel
During the outbreaks of SARS in 2003, internationally agreed measures were
instituted which were designed to restrict the movement of people possibly
infected with SARS. These measures were assessed by WHO to have greatly
contributed to bringing the disease under control.
Influenza (which is more infectious than SARS) is most infectious early in
the course of the disease (and possibly even before symptoms begin) and has
a much shorter incubation period (1 – 3 days). These important differences
make it unlikely that similar interventions will do more than delay or slow the
transmission of pandemic influenza at best, but this nonetheless may still be
deemed useful. Possible measures include:
• travel advice on travel to and from affected countries; • health information for exiting and returning travelers; and • health screening at ports.
(ii) National Travel
• Reducing unnecessary, especially long distance, travel may help slow
the spread of infection at the beginning of the pandemic.
• Local restrictions on the movement of people, e.g. in a community or
district, are unlikely to have much impact.
(iii) Mass Gatherings
• Decisions on whether to restrict mass gatherings will depend on whether
they are local, national or international events, the size, duration, and
whether in confined spaces or the open air.
• Closing schools will have an impact on maintaining the workforce in
(iv) Personal and Respiratory Hygiene
• People can reduce, but not eliminate, the risk of catching or spreading
influenza during a pandemic by:
Ø covering their nose and mouth when coughing or sneezing, using
a tissue when possible;
Ø disposing of dirty tissues promptly and carefully by bagging and
Ø avoiding non-essential travel and large crowds whenever
Ø maintaining good basic hygiene, for example washing their hands
frequently with soap and water to reduce the spread of the virus
from their hands to their face or to other people;
Ø cleaning hard surfaces (e.g. kitchen worktops, door handles)
frequently, using a normal cleaning product; and
Ø making sure their children follow this advice;
• If someone catches flu, they should:
Ø stay at home and rest;
Ø take medicines such as aspirin, ibuprofen or paracetamol to relieve
the symptoms (following the instructions with the medicines).
Children under 16 must not be given aspirin or ready made flu
remedies containing aspirin; and
Ø drink plenty of fluids.
(v) Staff Rostering
• Staff rostering to minimise interchange of staff between teams may help,
for example in health care settings, to reduce the impact on staffing. If
one member of a team becomes ill, all contacts in the team would be
asked to remain in voluntary quarantine.
Voluntary co-operation with all recommended measures would be sought;
mandatory quarantine and curfews are generally not considered necessary.
5.5 Health Services Response
The HSA will provide coordinated arrangements for the efficient, safe clinical
management of cases (and suspected cases) and their contacts in primary,
secondary and long term residential care. Maintaining services in the face of
unprecedented demands and disruption will present logistical problems.
Health service organisations and personnel also have a role in supporting the
public health response, and will be required to supply data for surveillance
and for local and national monitoring of the pandemic's impact.
(a) Investigation and Management of Cases and Contacts
The public will require clear guidance as to who should self-care (and how),
and who should seek medical assistance, when, how and where.
Provisional clinical management guidelines for adults and children, in the
community and hospital, are being developed, led by the Public Health
Department in consultation with relevant clinical groups. They will be posted,
and kept up to date, on the Government and HSA websites, taking account of
relevant clinical experience as necessary.
Health services plans will include plans for the efficient dispensing of antiviral
drugs within the agreed protocols, so that those recommended for antivirals
are able to start them within 48 hours of onset of symptoms.
(b) Infection Control
Infection control guidance for health, social care and community settings, will
be made available, based on WHO recommendations.
(c) Organisation and Reinforcement of Health Services
Depending on the number of cases, the HSA and private health care facilities
will need to establish ways of caring for large numbers of patients on a scale
outside their normal experience. This will include high dependency for people
of all ages care. Some of the key decisions that will need to be made in the
Cayman Islands are:
• provision of staff protection equipment;
• where patients are to be seen and assessed;
• how to ‘triage' patients, i.e. to quickly assess their needs and ensure
they are directed to the appropriate care, in primary care and hospitals;
• where patients are to be treated and admission criteria;
• the provision of diagnostic services and the safe handling of specimens
(following national protocols);
• how to maintain care for those staying in their own homes;
• the logistics of maintaining supply of equipment and pharmaceuticals,
including the blood supply;
• cancellation or reorganization of routine activity where possible;
• how other work is to be reorganized;
• how to roster staff to minimise the spread of infection in health care
premises, maintaining the right skill mixes, but ensuring that all staff
• how additional mortuary space is to be provided and safe practice for
• how to manage the interface between primary care and Accident
and Emergency Departments when primary care services are under
HSA will develop a detailed operational manual on the delivery of health care
during the pandemic.
5.6 The Civil Contingency Response - Reducing Societal Disruption
This plan is mainly concerned with the health response to an influenza pandemic,
but health services will be looking to other Government Departments and other
agencies to assist with the successful implementation of the health response.
Additionally, all organisations, including businesses, need to consider the
implications for their organisations, taking into account the information in
this plan, and make their own business continuity plans.
Existing contingency plans in dealing with disasters will come into effect
should the scale of a pandemic warrant it. These cover, for example:
• maintenance of essential services such as emergency services,
transport, food distribution, pharmaceutical supplies, utilities and
• management of mass casualties;
• maintenance of public order; and
• the role of the police and other security forces.
5.7 Workforce Education and Training
All organisations need to consider the implications of staff absence (because
of sickness, or the need for staff to take time off to care for others), at a time
when the workload for some may be increased. This will include:
• establishing minimum staffing levels;
• identifying a ‘front line' group of essential staff;
• considering the need to transfer or redeploy staff to do jobs they may
not be trained to do or familiar with, or to recruit additional staff or
• ensuring a system for vetting additional staff, including volunteers;
• accommodation, for example, portacabins with bunks for people to rest
between shifts when transport home may be difficult or disrupted.
Staff rosters must allow for adequate break and leave periods to ensure staff
are able to sustain a response over several weeks.
The educational and training needs of both regular staff and staff drafted in or
redeployed should be considered as part of preparedness planning but in all
likelihood it will need to continue during the response. Some of these needs
• appropriate staff training;
• training of volunteers;
• teaching staff how to handle and work with volunteers. Although there
will be regular volunteers, e.g. Pink Ladies, Cayman Islands Red Cross,
staff may not know who they will be working with until a shift starts
and cannot assume their skills and experience;
• keeping a database of former or recently retired clinical staff or local
doctors who may be called upon to help; and
• including in regular planning the possibility that a surge in staffing
might be required to cope with spikes in numbers of patients.
Staff may also need psychological or morale building support during what
will be a difficult time at work and at home.
Testing plans is an essential part of the training framework.
5.8 International Issues
A pandemic is, by definition, an international event. The Cayman Islands
must keep abreast of international developments and thinking about the best
practice approaches to coping with a pandemic. It also has certain international
obligations (in particular in respect of the PAHO/WHO, CAREC and the
UK) to report disease incidents and outbreaks and the actions the country is
6. Roles and Responsibilities of Key Organisations
This section outlines the roles and responsibilities of key organisations
with particular emphasis on the roles and responsibilities of the Ministry of
All organisations should have preparedness plans in place, covering both their
own part of the response and their business continuity arrangements, taking in
to account the advice in this document and other relevant contingency plans.
6.1 Organizational Structure
The organizational structure for development and implementation of the
Cayman Islands National Influenza Pandemic Plan (CINIPP) will be an
integral part of the Disaster Risk Management Structure – Cayman Islands
(Appendix I). The Cayman Islands National Influenza Pandemic Committee
(CINIPC) will be the specific hazard management group for the management
of any Influenza Pandemic. However, until the full development of this
structure, CINIPC will operate similar to the National Hurricane Committee
(NHC). The Cayman Islands National Influenza Pandemic Health Task Force
(CINIPHTF) will deal with all health aspects.
6.2 The Cayman Islands National Influenza Pandemic Committee
(CINIPC)
This committee (membership is shown in Appendix I) is similar to the National
Hurricane Committee, and will take on the role of Strategic Planning. It will
be chaired by the His Excellency the Governor.
The Medical Officer of Health and the Director of the Hazard Management
Cayman Islands (HMCI) will be co-coordinators. A core group will coordinate
inputs from various departments and agencies.
Members of the Committee will:
• bring relevant experience to the Committee;
• contribute to the provision of high quality advice to the Government;
• be expected to make considered contribution to the decision making
processes of the Committee;
• provide guidance when an issue which falls within their particular area
of expertise is under discussion; and
• ensure the existence of sound business continuity plans in the respective
departments/agencies under their jurisdiction.
6.3 The Cayman Islands National Influenza Pandemic Health Task Force
(CINIPHTF)
The Influenza Pandemic Health Task Force, (membership is shown in Appendix
I), under the chairmanship of the Honourable Minister for Health, will ensure
that operational plans are in place to address the areas of Surveillance,
Prevention, Treatment and Risk Communication; the last of these is particularly
intended to assist the general public with information.
The Medical Officer of Health will coordinate the discharging of responsibilities
of the Health Task Force.
The Committee will advise the Government on scientific matters relating to
the response of health services to an influenza pandemic.
This advice will contribute to the work of the CINIPC, which will incorporate
it in its reports to the Cabinet.
Members of the committee will:
• bring relevant experience to the Group;
• contribute to the provision of high quality advice to the Honourable
Minister for Health; and
• be expected to make contributions to the decision making processes of
the Committee.
6.4 Ministry of Health
The Ministry of Health has overall responsibility for planning, direction and
central co-ordination of the Cayman Islands health response. It will:
develop and ensure the ongoing monitoring and revision of the
Cayman Islands Influenza Pandemic Plan.
improve preparedness across all health services providers.
iii. oversee implementation of the plan.
provide policy direction for the public health response and develop
strategies to reduce the impact of the pandemic on the health of the
brief Cabinet.
vi. provide information and guidance to the HSA, government
departments and agencies and other voluntary and non-governmental
organisations to assist them to plan and respond appropriately.
vii. in partnership, and liaising closely with the other organisations
(indicated in brackets):
• secure supplies of an effective vaccine, antiviral agents,
antimicrobials and other pharmaceutical products and other
essential supplies e.g. face masks, surgical gloves etc. (HSA);
• develop strategies and priority groups for use of vaccine and use
of antiviral agents (Health Task Force); and
• co-ordinate provision of consistent, accurate advice to health
professionals, managers, the public and the media (Public Health
Department and HSA).
The Medical Officer of Health will coordinate the discharging of the
responsibilities of the Ministry and:
• provide a coordinating role for a National Public Health response.
• will liaise with the PAHO/WHO Health Protection Agency of the UK,
CAREC and other International Agencies.
6.5 Hazard Management Cayman Islands (HMCI)
The HMCI provides the national focus for cross-departmental and cross-
agency commitment, co-ordination and co-operation to enable the Cayman
Islands to deal effectively with disruptive challenges, emergencies and crises
If, as the consequence of a pandemic, control measures and/or other measures
have implications for departments and agencies other than the health services
alone, HMCI will co-ordinate strategic decision making on Cayman Islands
national priorities across departments to ensure an integrated response to the
HMCI would also be responsible for:
• activation and management of the National Emergency Operations
Centre, if necessary;
• liaising with other Caribbean countries, primarily through the CDERA
• coordination of external assistance where necessary; and
• coordination of the voluntary sector.
6.6 Government Information Services (GIS)
• Government Information Services will head the Risk Communication
Sub-committee. It will be responsible for developing and implementation
of the Risk Communication Strategy.
6.7 Public Health Department (PHD)
The PHD is the lead agency responsible for advising and supporting the national
public health response to major infectious disease incidents and outbreaks,
working along with the Cayman Islands Hospital Laboratory and HMCI.
The PHD will, in co-ordination, with colleagues in the HSA:
• provide specialist public health advice, together with operational and
investigative support, to Public Health Staff and others with formal
responsibilities for dealing with pandemic influenza;
• co-ordinate national influenza surveillance: obtain and analyze
information on national and international influenza activity (including
laboratory, clinical and mortality data) and distribute it on the HSA
website, and through regular bulletins to relevant personnel at frequent
• co-ordinate development of national guidelines for health professionals;
• monitor vaccine uptake, when vaccine becomes available.
6.8 Health Services Authority (HSA)
The HSA is responsible for:
• ensuring tried and tested command and control structures are in place across
• arrangements to appoint a named influenza co-coordinator, (Health Disaster
Preparedness Coordinator), and a pandemic planning commit ee with
appropriately wide representation to oversee the delivery of health care;
• routinely reporting data required by the PHD and the Ministry of
Health on a pandemic and its impact on delivery of care by the health
• arrangements for the optimum care of those affected, including the
ability to mobilize health care resources in other hospitals and health
centres at short notice, to support them and to sustain patients in the
community should hospital services be reduced or compromised for a
• ensuring the HSA has the appropriate facilities for infection control;
• arrangements to have mutual support arrangements with the private
• contingency staffing arrangements at hospitals, district health centres
and public health services;
• arrangements to provide antiviral treatment and to immunize essential
staff according to national guidelines;
• communication arrangements to health care professionals, the public
and the media, including timely cascades of information from national
and international sources.
The Medical Director of the HSA will ensure the provision of clinical care and
the Health Services Disaster Preparedness Coordinator will ensure all support
services are in place.
6.9 Other Government Departments
The following Government Offices and Departments will be directly or
indirectly involved in the response to an influenza pandemic, or will have
client groups who need advice and/or need to be kept informed (e.g. utilities,
schools, colleges, business and transport):
• All Ministries• Education Department • Department of Tourism• Civil Aviation Authority• Immigration Department
• Customs Department • Royal Cayman Islands Police Service• Airports Authority • Ports Authority• Department of Agriculture • Cabinet Office
Other Government Departments will be consulted either directly or via the
collective decision making mechanism provided by HMCI before any actions
are agreed or taken that will impact on their sector or area of business.
10.10 Private Health Care Providers
• participate in the Influenza Surveillance Program;
• provide care and management of influenza cases in accordance with the
clinical protocols developed by the Health Task Force.
10.10 All Other Organizations
These include private sector businesses and non-governmental organizations.
• ensure business contingency plans as per Appendix II.
7. Phase by Phase Actions
The Cayman Islands' response follows the WHO phases outlined in Chapter 3.
This present chapter sets out the action to be taken by different organizations
at each phase. At each stage, WHO will inform the Ministry of Health of the
increased alert level. The Medical Officer of Health will communicate this
information, together with an assessment of the risk to the Cayman Islands, to
healthcare professionals, the public and relevant organizations. The actions
outline a proportionate response to the level of risk posed at each phase.
It is recognized that there may be a very short time period between the virus first
emerging internationally, its arrival in the Cayman Islands and its becoming
widespread in this country.
(A) Inter- Pandemic Period – Actions Required for Phases 1& 2
Phase 1. No new influenza virus subtypes detected in humans.
Phase 2. No new influenza virus subtypes detected in humans. Circulating
animal influenza virus subtype poses a substantial risk of human disease.
The overarching goal is to strengthen influenza pandemic preparedness and
minimize the risk of transmission to humans and to detect and report such
transmission rapidly if it occurs.
(i) Planning and Coordination
• Develop and maintain National Influenza contingency plan in harmony
with international planning.
• Update the membership of the CINIPC and CINIPHTF.
• Assess preparedness status and identify actions needed to fill gaps.
• Keep national influenza pandemic contingency plans up to date,
and improve preparedness, working with each other and other
• Provide information to other Government Departments, the HSA
and other relevant organizations to assist them to develop their own
contingency plans.
• Arrange workshops (as required) to discuss implications of a pandemic
for other organizations.
• Increase awareness of seasonal flu and flu immunization policies through
media campaigns.
• Use opportunities to prepare and inform the public about pandemic
• Prepare draft pandemic information frequently asked questions etc for
the public which can be issued as necessary.
• Strengthen national systems for influenza surveillance for early
detection of influenza infections in both humans and animals (Public
Health Department and Department of Agriculture are responsible).
• Report routine and unusual surveillance findings to relevant national
and international authorities.
• Assess burden of seasonal influenza to help estimate additional needs
during a pandemic.
• Develop contingency plan for ongoing monitoring of information, for
assessment of impact and resource needs during the pandemic phase
(e.g. morbidity, mortality, workplace absenteeism, risk groups affected,
health-care workers and other essential workers' availability, health-
care supplies, bed occupancy/availability, admission pressures, use of
alternative health facilities, mortuary capacity).
(iii) Vaccines and Antiviral Drugs
• Develop a strategy (e.g. stockpiling) to ensure access to antivirals for
national use; ensure availability of data to project likely needs during
higher phases.
• Consider priorities and criteria for deployment and use of antivirals
during pandemic alert and pandemic periods.
• Develop strategies to increase uptake of seasonal influenza vaccine.
(Public Health Department will be responsible).
• Define national objectives for the use of pandemic vaccines; develop
preliminary priorities for pandemic use, based on expected availability
(Health Task Force will be responsible).
• Develop strategies to allow access to vaccines and review logistic
and operational needs for implementation of pandemic vaccine
strategy (vaccine storage, distribution capacity, cold-chain availability,
vaccination centers, staffing requirements for vaccine administration).
(iv) Health Systems Response
• Ensure that up-to-date contingency plans and strategies are in place to
enable the health-care sector to respond successfully to a pandemic.
• Estimate pharmaceutical and other material supply needs; commence
arrangements to secure supply.
• Increase awareness and strengthen training of health-care workers on
pandemic influenza. (HSA & Private Health Care Providers)
• Test contingency plans regularly, including command and control
(v) Communications
• Establish phased national communications strategy to address
information needs brought about by pandemic influenza.
• Update national authorities, other partners and stakeholders, including
at-risk groups and the public, with current information on virus spread
and risks to humans.
• Establish and maintain a website with relevant information.
• Establish networks among key response stakeholders, including risk
communicators, non-health government departments, and professional
and technical groups.
• Familiarize news media with national plans, preparedness activities and
decision-making related to seasonal and pandemic influenza.
• Develop feedback mechanisms to identify public level of knowledge
about pandemic influenza and emerging public concerns. Address
rumors proactively and correct misinformation.
• Prepare and send out an annual letter on the national influenza
immunization programme to healthcare professionals.
• Maintain routine information on seasonal flu and flu immunization for
the public via leaflets, posters, and websites.
• Develop educational materials for healthcare and human services
providers, the media, and the public on pandemic influenza preparedness
and response.
• Develop strategies and materials to support a response to a pandemic and
to promote public trust and confidence and decrease fear and anxiety.
(B) Pandemic Alert Period - Actions Required for Phase 3
Phase 3. Human infection(s) with a new subtype, but no human-to-human
spread, or, at most, rare instances of spread to a close contact.
Planning and Coordination
• Review Cayman Islands Pandemic Plan.
• Continue to consult across Government to ensure all sectors are
developing contingency plans.
• Continue to assess preparedness plans and fill any gaps.
• Collaborate with international partners to respond to a pandemic alert.
• Inform Government officials (including Cabinet and legislators) of
pandemic alert status.
• Establish national case definition (or review/modify existing definition)
based on WHO guidance.
• Enhance human and animal surveillance.
• Ensure timely laboratory diagnosis is available through local laboratory
capacity and referral mechanisms.
• If a case is detected:
Ø collect information on possible source of infection and
Ø monitor contacts.
• Consider heightening surveillance as indicated by circumstances of the
case, for example, the person's country of origin, other related infections
or the person's connections with the Cayman Islands.
(iii) Vaccines and Antiviral Drugs
• Assess availability of antivirals and plan for distribution and access.
• Ensure treatment and infection control protocols are in place.
• Ensure protective equipment is available to all needed.
• Plan for procurement of vaccine when it becomes available.
• Establish strategies to prevent the spread of infection in the Cayman
(iv) Health Systems Response
• Provide public and private health care providers with updated case
definitions, protocols and algorithms to assist with case-finding,
management, infection control and surveillance.
• Assess capability/capacity for implementing infection control
procedures for ill patients; implement infection control consistent with
existing WHO guidance.
• Identify target groups for delivery of key messages; develop appropriate
materials, formats and language options.
• Enhance healthcare provider awareness of the potential for a pandemic
and the importance of diagnosis and viral identification for persons with
influenza-like illness, especially from potentially affected areas.
• Review and update information materials for news media, general
public and policy-makers.
• Review communications systems facilities to ensure that they are
functioning optimally, and that contact lists are up to date
(C) Pandemic Alert Period - Actions Required for Phases 4 & 5
Phase 4. Small cluster(s) with limited human-to-human transmission but
spread is highly localized, suggesting that the virus is not well adapted to
Phase 5. Large cluster(s) but human-to-human spread still localized, suggesting
that the virus is becoming increasingly better adapted to humans, but may not
yet be fully transmissible (substantial pandemic risk).
Planning and Coordination
• Convene the Cayman Islands National Influenza Pandemic Committee
to review all information related to the potential pandemic and advise
on the response.
• Assess preparedness status and identify immediate actions needed to
fill gaps. Ensure all operational plans are prepared.
• Establish coordination of response activities through the Emergency
Operations Center.
• Coordinate with WHO, UK and other governments.
• Notify government officials (including Cabinet and legislators) of
pandemic status.
• If it becomes clear that the new virus is not spreading widely in the
world, the NIPC will be stood down and the relevant organizations
informed accordingly. Some activities will continue on a precautionary
• Collaborate with international organizations to assess epidemiology of
the diseases and efficiency of person to person transmission.
• Implement plans to enhance national surveillance and identify suspect
cases and/or introduction of a new virus into the Cayman Islands,
including dissemination of WHO agreed case definition for surveillance
• Provide interpretation of surveillance activities with careful interpretation
to avoid spurious reporting of outbreaks.
• Ensure availability of diagnostic testing for the virus.
• Provide reference laboratory support to test clinical specimens for
influenza and identify a new strain.
(iii) Vaccines and Antiviral Drugs
• Finalise vaccine supply requirements.
• Liaise with vaccine manufacturers over production plans.
• Start negotiating central purchase of vaccine.
• Liaise with PAHO and UK for assistance as the demands will likely be
• Develop a framework for delivery of mass vaccination to priority groups
depending on the availability of vaccine (quantities).
• Access the antiviral supplies and liaise with antiviral manufacturers
over accelerating antiviral supply.
• Finalise plan for use, access to and distribution of antiviral drugs.
(iv) Health Systems Response
• Assess capacity of medical and emergency response systems to meet
expected needs during a pandemic.
• Provide updated guidance, if indicated, to healthcare providers on
clinical management and infection control.
Ø review plans, based on gaps identified as a result of exercises
held previously; and
Ø be prepared to recognize, investigate and treat potential cases
according to the algorithm on management of patients with
suspected avian influenza.
• The Ministry of Health will assess risks based on information from
WHO and HSA and inform relevant organizations as appropriate.
• Update health professionals with an assessment of the significance and
information about the immunisation strategy as appropriate.
• Prepare and issue travel advisories as appropriate in conjunction with
Cabinet Office and Department of Tourism.
• Provide regular informative briefings for media.
• Implement public education on the potential for a pandemic and the
actions to be taken to reduce risk
(vi) Other Public Health Interventions
• Provide education to travelers, and issue travel advisories, precautions
or restrictions (if warranted by disease epidemiology); investigate
illness among travelers returning from affected areas and implement
isolation and quarantine, as needed.
• If cases occur in the Cayman Islands, implement intensive control
measures (isolation of case(s), quarantine of contacts in addition to
antiviral treatment of cases and prophylaxis for contacts):
Ø investigate possible reservoirs of infection;
Ø if hospitalized, treat patients in single rooms with full infection
control measures; and
Ø follow the algorithm for the management of suspected cases of
avian flu. If diagnosed within 48 hours, consider appropriateness
of antiviral treatment of the case plus prophylaxis for close
contacts who may have been infected.
(D) Pandemic Period – Action Required for Phase 6
Phase 6. Increased and sustained transmission in the general population
The WHO has announced that an influenza pandemic has started. In respect of
the Cayman Islands, this phase is divided into two stages:
(1) no cases in the Cayman Islands; and(2) cases in the Cayman Islands
No Cases in the Cayman Islands
Planning and Coordination
• Update government officials, (including Cabinet and legislators on
pandemic status).
• Finalise official guidelines.
• Collaborate with international organizations to assess epidemiology of
disease outbreaks and efficiency of person-to-person transmission.
• Implement travel advisories, precautions or restrictions, as
• Investigate illness among travelers returning from affected areas;
implement isolation and quarantine, as needed.
• Continue activities to enhance detection of cases of influenza at hospital
and outpatient settings.
• Ensure availability of diagnostic reagents for pandemic influenza strain
at the Cayman Islands Hospital laboratories.
• Ensure reference laboratory support to test clinical specimens for
influenza and identify new strain.
(iii) Vaccines and Antiviral Drugs
• Review and revise, if necessary, priority groups and strategies for
antiviral drug use and vaccination
(iv) Health Systems Response
• Review and revise, if necessary, plans for healthcare delivery and
community support.
• Assess availability of supplies, and materials for infection control and
clinical care of infected patients.
• Provide guidance to healthcare providers on infection control guidelines
for hospitals, long-term care facilities, and outpatient settings.
• Review the response plan.
• Update stakeholders and the media through regular briefings.
• Educate healthcare providers through seminars, bulletins and other
• Continue public education activities.
Cases in the Cayman Islands
Planning and Coordination
• Identify pandemic cases in the Cayman Islands.
• Convene regular meetings of the CINIPC, CINIPHTF, and other sub-
• Consider if, and when, to declare a Cayman Islands State of
• Continue to monitor the course of the pandemic outside the Cayman
• Monitor course of the pandemic virus in the Cayman Islands
Ø occurrence and causes of complications; andØ deaths.
• Distribute information via the bulletin weekly, although when new
information appears, inform labs and physicians immediately through
• Investigate local outbreaks/sporadic cases.
• Assess the effectiveness of public health measures.
(iii) Vaccines and Antiviral Drugs
• Review and revise priority groups for vaccination and antiviral drug
• According to availability of vaccine, implement immunization strategy
according to evolving circumstances and availability of vaccine.
• Review advice on priority groups to be vaccinated in light of emerging
clinical data.
Ø availability and use of vaccine;Ø vaccine uptake; andØ effectiveness of vaccine
(iv) Health Systems Response
• All heath care providers activate their Pandemic Influenza Plans.
• Prepare to restrict hospital admissions to meet the expected increased
demand for hospital beds.
• Consider ongoing training needs of redeployed staff or staff who are
likely to have to undertake new duties.
• Establish studies to monitor outcome of treatment.
• In accordance with facility plan;
Ø consider bed and staffing availability;Ø advise on use of antivirals; andØ administer vaccine (if available).
• Alert all health care professionals to situation and ask them to activate
their plans.
• Public Health Department continues to lead on updating clinical and
other guidance in light of emerging findings, including advice on:
Ø clinical management; andØ Infection control procedures.
• Daily situation reports from the Public Health Department.
• Government Information Services ensures coordinated media handling
Ø all information and advice for the public regularly updated;
Ø regular informative press briefings;
Ø prepare and issue international travel advisories as appropriate
in conjunction with the Cabinet Office and the Department of
Ø issue advice and guidance to the public about treatment, infection
control and related measures such as travel.
(E) End of First Pandemic Wave – Actions Required
• This phase is assumed to refer to the end of the first pandemic wave in
the Cayman Islands.
• Pandemic virus may still be circulating internationally.
Planning and Coordination
• Review and revise response.
• Review with HMCI the response in terms of the Cayman Islands
preparation for this and other emergencies.
• Estimate overall pandemic health impact including mortality and
• Ensure systems are in place to detect possible re-emergence.
• Consider serological surveys to assess population immunity.
• Restock laboratory reagents and equipment.
Vaccines and Antiviral Drugs
• Assess vaccine coverage, effectiveness of targeting of priority groups,
and efficiency of distribution and administration; determine number of
person who remain unprotected.
• Assess vaccine efficacy, safety, and impact during the pandemic.
Health Systems Response
• Put plans in place to resume business continuity.
• Prepare for future wave(s).
• Consider future manpower, education and training.
• Inform PAHO of any change in Cayman Islands control measures.
• Inform health professionals that the first pandemic wave is considered
over in Cayman, but activity may be ongoing in other countries.
• Inform the public and media about the situation in the Cayman
(vi) Cross Government and Civil Contingencies Response
• Consider actions needed to resume business continuity.
• Prepare for future pandemic wave(s).
• Consider future manpower, education and training needs.
Second or Future Pandemic Waves
• Pandemic virus may still be circulating internationally.
• Pandemic virus may have evolved.
• Impact may be less or even greater than first phase.
• Early detection of the second wave in the Cayman Islands.
• Reactivation of Phase 6.
(F) Post Pandemic Period – Return to Inter-Pandemic Period
• This or a similar virus is likely to remain in circulation.
• It may take months or even several years for some national services to
• Assessment and evaluation: review and revise plans.
The Cayman Islands National Influenza Pandemic Committee will prepare
a report, reviewing the effectiveness of and lessons learned from the plan.
The chairman will then decide if the Committee should be stood down.
All contingency plans should be reviewed in the same way in the light of
experience during the pandemic.
• Assessment and evaluation across all sectors.
• Returning to normal business continuity may take some time and
recovery plans may need to be drawn up.
NB: The operations manuals will have the specific details of Surveillance,
Prevention, Treatment and Risk Communications
Appendix I
A. Disaster Risk Management Structure
B. Cayman Islands National Influenza Pandemic Committee (CINIPC)
C. Cayman Islands National Influenza Pandemic Health Task Force
(CINIPHTF)
B. Cayman Islands National Influenza Pandemic Committee (CINIPC)
His Excellency the Governor (Chairman)
Honourable Minister for Health
Honourable Chief Secretary
Honourable Attorney General
Honourable Financial Secretary
Cabinet Secretary
District Commissioner –Cayman Brac
Chief Officers (all Ministries)
Chief Education Officer
Commissioner of Police
Director of Children and Family Services
Chief Executive Officer – HSA
Chief Medical Officer
Medical Officer of Health
Medical Director – HSA
Pathologist – HSA
Chief Nursing Officer – HSA
Staff Officer – Governor's Office
Chief Agriculture and Veterinary Officer
Chief Environmental Health Officer
Collector of Customs
Chief Immigration Officer
Director of Port Authority of the Cayman Islands
Director of Airport Authority
Director of Civil Aviation
Director of Red Cross
Director of Tourism
Government Information Services RepresentativeChamber of Commerce Representative
NB: The Medical Officer of Health and the Director of HMCI will coordinate the input
from various agencies.
HMCI will coordinate command and control of EOC operations when the National
EOC is activated.
C
. Cayman Islands National Influenza Pandemic Health Task Force (CINIPHTF)
This will ensure operational plans are established covering Surveillance, Prevention
and Treatment and also Risk Communication to the public.
Honourable Minister of Health (Chairman)
Chief Officer – Ministry of Health
Chief Executive Officer – HSA
Medical Officer of Health – PHD
Medical Director – HSA
Chief Nursing Officer – HSA
Chief Medical Officer
Pathologist – HSA
Chief Agriculture and Veterinary Officer
Chief Environmental Health Officer
Medical Officer-in- Charge – Cayman Brac
Disaster Coordinator – HSA
Chief Pharmacist – HSA
Public Relations Officer – HSA
Chrissie Tomlinson Memorial Hospital Representative
GIS Representative
Cayman Islands Medical and Dental Association Representative
Notes (i)
Four Sub-Committees of the CINIPHTF will address the issues pertinent
to Surveillance; Prevention; Treatment and Risk Communication
Medical Officer of Health will coordinate the discharge of the
responsibilities of the CINIPHTF.
Appendix II
Pandemic Flu Business Contingency Planning Guidance
In the event of an influenza pandemic, government departments and businesses
will have a key role to play in minimizing the risk to employees' health. They
will also need to maintain essential operations. Given the highly uncertain
nature of a pandemic, we cannot know in advance how serious it will be and
who will be most affected. It is therefore important that contingency plans are
developed which can address a range of scenarios.
This guidance and checklist have been produced to assist both businesses and
government departments in preparing plans. The guidance aims to provide
more information to the organisations about the threat from pandemic flu, the
impact it may have on business and services, and what government is doing
The checklist has been adapted from one produced in the UK and the U.S.A.
It identifies important activities which organisations can do to prepare for a
pandemic. It was designed primarily for larger businesses, but some elements
may be of use to smaller businesses.
2. The Cayman Islands Influenza Pandemic Contingency Plan
During an influenza pandemic, the Government will aim to encourage people
to carry on as normal, as far as possible if they are well, while taking additional
precautions to protect themselves from infection and to lessen the risk of
spread to others. The main objectives of the Government's response to an
influenza pandemic will be to:
• limit illness and death arising from infection;• provide treatment and care for those who become ill;• minimize disruption to health and other essential services;• maintain business continuity as far as possible; and• reduce as far as possible disruption to society.
3. Key Elements for Managing a Pandemic
(a) Medical Measures
The Government is building up a stockpile of sufficient antiviral drugs to
treat 25% of the population, in line with the planning assumption that 25%
of the population will become ill. These drugs will be the only major medical
countermeasure available in the absence of a specific vaccine. Used for
treatment only, they need to be taken as early as possible after symptoms
first start, preferably within 48 hours of onset. Their effectiveness will not,
however, be known until the pandemic virus is circulating.
If a pandemic were to emerge before the antiviral stockpile was complete,
available supplies would be prioritized to treat health workers and priority
medical groups first. As further drugs become available, they would be offered
to treat those who become ill.
Vaccines against the virus would not be available until at least 4-6 months into
the pandemic. This could be well after the first wave of illness in the Cayman
Islands has struck. The Government is intending to order sufficient vaccines
for the whole it is the belief of the scientific community that there will be
another severe influenza pandemic, but the question is when.
But, even after vaccines start to become available, the total order is unlikely
to be completed for several months, and priorities for receiving vaccines will
have to be set. Decisions on priorities will be finalized during a pandemic
when the impact of the virus is known.
In the meantime, all sectors will need to plan to cope without vaccines in at
least the first wave. When vaccines start to become available, essential and
emergency services (other than the health service) and other sectors should
not assume priority access.
(b) Reducing the Risk of Infection
Transmission of the pandemic virus from person-to-person will be through
close contact. The evidence suggests that the most important transmission
routes will be from coughing and sneezing and through direct and indirect
contact with infected people. Airborne or fine droplet transmission may also
These characteristics mean that the pandemic virus is expected to spread very
quickly through the population after if first arrives in the islands. Given that
it is likely to enter through the air bridge, it may only take a few days for the
virus to become widespread.
Early management of the pandemic will rely mainly on two elements. Firstly,
antiviral drugs for treating those ill with the pandemic. Secondly, public health
messages encouraging sensible precautionary measures to reduce the risk of an
individual becoming infected. Alongside the key message to people to continue
their everyday (essential) activities as normal will be messages encouraging
personal responsibility for self-protection and social responsibility to lessen
spread and thus protect others. The key public health messages will be:
If you do catch flu:
• stay at home and rest;
• take medicines such as aspirin, ibuprofen or paracetamol to relieve the
symptoms.
Children under 16 must not be given aspirin or flu remedies
containing aspirin; and
• drink plenty of fluids.
You can reduce, but not eliminate, the risk of catching or spreading
• covering your nose and mouth when coughing or sneezing, using a
tissue when possible;
• disposing of dirty tissues promptly and carefully by bagging and binning
• avoiding non-essential travel and large crowds wherever possible;
• maintaining good basic hygiene, for example washing hands frequently
with soap and water to reduce the spread of the virus from your hands
to your face, or to other people;
• cleaning hard surfaces (e.g. kitchen worktops, door handles) frequently,
using a normal cleaning product; and
• making sure your children follow this advice.
(c) Social Measures and Travel Restrictions
A third possible element of the response is the use of additional measures
which would reduce social mixing and thereby aim to reduce exposure to the
virus. The Cayman Islands Flu Contingency Plan sets out a range of possible
additional measures such as:
i. postponing large public gatherings and events;
ii. issuing advice to travel only if essential and encouraging remote
iii. the introduction of additional port health measures or entry screening
of passengers returning from countries first affected by the pandemic
virus. Even if implemented, such measures are likely to be stopped once
the virus has taken hold in the Cayman Islands; and
iv. the introduction of exit screening at ports to protect other countries, if
the Cayman Islands were one of the first countries affected. As further
countries become affected, WHO would probably advise that this
measure be discontinued.
Once the nature of the pandemic virus is known, emerging advice from WHO
and UK Department of Health will be used to inform decisions on introducing
4. Key Planning Assumptions
(a) Public Health Effects
Once it has reached the Cayman Islands, the infection is likely to spread quickly
throughout the islands. For planning purposes, the assumption is for:
i. a cumulative clinical attack rate of between 25% and 50% of the
population over one or more waves, each of around 15 weeks duration,
weeks or months apart. The second wave may be the more severe.
This compares with a usual seasonal influenza attack rate of 5 – 10%.
(b) Staff Absence from Work
The level of staff absence from work during a pandemic will depend on the
nature of the pandemic virus when it emerges. The planning assumptions set
out below are based on analysis of past pandemics, published evidence and
scientific modeling. Given the inevitable uncertainties, a range of figures is
given in some areas. Organisations should ensure that their continuity plans
take these ranges into account.
During a pandemic, staff will be absent from work if:
i. they are
ill with flu. Numbers in this category will depend on the
clinical attack rate. If the attack rate is 25%, one quarter of staff will be
sick (and hence absent from work for a period) over the course of the
pandemic. If a pandemic occurs over one wave, this level of cumulative
absence could be spread over a period of around 3 – 4 months. But there
may be more than one wave, with absence from work being spread
across those waves;
ii. they
need to care for children or other family members who are ill;
iii. they have
other medical problems;
iv. their employers have advised them to
work from home; and
v. they decide to absent themselves for
other reasons.
Business continuity planning against an influenza pandemic should use these
categories to estimate the number of staff likely to be absent from work at the
peak of the pandemic. In order to estimate the total number of staff likely to
be absent from work at the peak of a pandemic, employers should add:
i. the average number of staff
‘normally' absent from work;
ii. the proportion of staff whom they will advise to work from home; and
iii. their judgment based on the nature of their business and their employment
practices, as to the number of staff who might absent themselves from
work for other reasons.
It is expected that ill people will on average be absent for 5 – 8 working
As a rough working guide, organisations employing large numbers of people,
with flexibility of staff redeployment, should ensure that their plans are capable
of handling staff absence rates of up to 15% over the 2 - 3 week peak of a
pandemic (in addition to usual absenteeism levels). Small businesses (up to 15
people), or larger organisations with small critical teams, should plan for level
of absence rising to 30% at peak, perhaps higher for very small businesses
with only a handful of employees.
Finally, employers should note that absentee rates could be higher than the
estimates given if people take longer to recover from infection than the
assumption shown above, or if some age groups of the population are affected
more severely than others.
5. Issues to Consider in Business Continuity Planning
In carrying out business continuity planning, organisations will wish to
i. support efforts to reduce the impact of the pandemic by:
• taking all reasonable steps to ensure that employees who are ill or
think they are ill during a pandemic are positively encouraged not
to come into work. Personnel policies may need to be reviewed to
achieve this aim;
• ensuring that employers and employees are made aware of
Government advice on how to reduce the risk of infection during a
pandemic (information for staff will be available via the internet and
in printed form); and
• ensuring that adequate hygiene (e.g. hand-washing) facilities are
ii. put measures in place to maintain core business activities for several
weeks at high levels of staff absenteeism, including options for remote
working and increasing on-line options for customers and business
iii. identify those essential functions and posts, and perhaps individuals,
whose absence would place business continuity at particular risk;
iv. identify which services could be curtailed or closed down during all,
or the most intense period, of the pandemic;
v. identify inter-dependencies between organisations and ensure they are
resilient, for example by ensuring that suppliers delivering services
under contract have appropriate arrangements in place to allow
themselves to sustain their service provision;
vi. as necessary, factor into their planning the need to support the health
vii. factor into their planning the presumption that assistance from the
Armed Services will not be available; and
viii. factor into their planning that medical counter-measure will not solve
business continuity requirements because antiviral drugs for treatment
will only lessen the severity of the illness. They will neither cure it nor
significantly reduce absenteeism.
In addition, organisations will need (as necessary) to be aware of, and plan
for the consequences of measures that the Government may conclude are
necessary to control or delay the spread of the disease, described below, which
may result in additional staff absence from work.
6. Pandemic Flu-Business Contingency Planning Checklist
This checklist is not exhaustive. Nor will it all necessarily be relevant to your
business. It is a guide to help you start thinking about what you may need to
(a) Plan for the impact of a pandemic on your business.
i. Identify a leader and/or team with defined roles and responsibilities
for preparedness and response planning. The planning process
should include input from a wide range of stakeholders e.g. health
and safety representatives, Human Resources.
ii. Identify the critical activities undertaken by your business which
would have to continue during a pandemic, as well as the employees
and other inputs that support those activities (e.g. raw materials,
suppliers, sub-contractor services/products, logistics, process
iii. Consider how internal resources could be re-allocated to ensure
those activities are maintained. Consider what activities could or
would come to a stop during a pandemic.
iv. Discuss with your suppliers/sub contractors whether they have
robust business continuity plans in place – your organisation is
only as good as those on whom it depends.
v. Consider preparing an additional pool of workers to undertake
key tasks and provide training where appropriate (e.g. contractors,
cross train employees, retirees).
vi. Determine the potential impact of a pandemic on your business-
related travel (e.g. if international travel is curtailed in certain
countries due to quarantines and/or border closures).
vii. Note that current planning assumes that domestic travel will not
be restricted, although the Government may advise against non-
essential travel within the islands.
viii. Establish an emergency communications plan and revise
periodically. This plan should identify key contacts (with back-
ups), a chain of communications (including suppliers, customers
and employees), and processes for tracking and communicating
business and employee status.
ix. Implement an exercise to test your plan, and revise it periodically
taking into account updated advice and guidance from
(b) Plan for the impact of a pandemic on your employees and
i. Guided by advice from Government's Contingency Plan, forecast
and plan for employee absences during a pandemic. This could
be the result of a number of factors including personal illness,
family member illness, bereavement, possible disruption to
transport, etc.
ii. As a general approach to reducing the spread of the infection
across the islands, assess your business needs for continued
face to face contact with your customers/suppliers and consider
plans to modify the frequency and/or type of face-to-face contact
among employees and between employees and customers.
iii. Whilst there is no intention to restrict domestic travel, the
Government is likely to advise against non-essential travel, and
this should be taken into account in planning.
iv. Encourage annual influenza vaccination for employees.
v. Plan for a likely increase in demand for employees' health and
welfare services, if they are available, during a pandemic.
vi. Identify employees and key customers with special requirements,
and incorporate the requirements of such persons into your
preparedness plan.
vii. Consider your customers' needs during a pandemic and whether
to review your business model and arrangements to continue
to meet those needs. (e.g. enhance mail ordering and internet
(c) Establish policies to be implemented during a pandemic.
i. Guided by advice issued by Government, establish policies for
sick-leave absences unique to a pandemic, including policies
on when a previously ill person is no longer infectious and can
return to work after illness (i.e. when they are no longer showing
symptoms and feel better).
ii. Establish policies for flexible worksite operations (e.g. working
from home) and flexible work hours (e.g. staggered shifts).
iii. Establish policies for reducing spread of influenza at the worksite
(e.g. promoting respiratory hygiene/cough etiquette, and asking
those with influenza symptoms to stay at home).
iv. Follow the current policies for employees who are suspected to be
ill, or become ill at the worksite (e.g. infection control response,
sick leave policies).
v. Set up authorities and procedures for activating and terminating
the company's response plan, including altering business
operations, if necessary. This might include reducing operations
and transferring business knowledge to key employees. It should
include nominating deputies for key employees in advance, in
case these key employees are unable to come to work.
vi. In the early stages of a pandemic with outbreaks overseas, but
not yet in C.I.: Guided by advice from the Government, establish
policies on travel to affected geographic areas overseas and
develop policies on managing employees working in or near
an affected area when an outbreak begins (and later on in the
(d) Allocate resources to protect employees and customers during a
i. Provide sufficient and accessible means for reducing spread
of infection (e.g. provision of hand washing facilities or hand-
hygiene products).
ii. Consider additional measures to reduce the risk of infection, such
as more frequent cleaning on premises, and ensure the resources
to achieve these will be available.
iii. Consider whether enhanced communications and information
technology infrastructures are needed to support employees
working from home, telephone conferences instead of face to
face meetings and remote customer access.
(e) Communicate to and educate your employees.
i. Disseminate easily accessible information about pandemic flu to
your workforce which is appropriate to:
the stage of alert (e.g. signs and symptoms of influenza,
modes of transmission when this information is available);
personal and family protection and response strategies (e.g.
hand hygiene, coughing/sneezing etiquette, contingency
ii. Ensure that communications are culturally and linguistically
iii. Disseminate information to employees about your pandemic
preparedness and the response plan for your business, including
their role in this plan.
(f) Coordinate with external organizations.
i. Collaborate with insurers, health plans and local healthcare
facilities to share your pandemic plans and understand their
capabilities and plans.
ii. Communicate with the Public Health Department and/or
emergency responders about the assets and/or services your
business could contribute to the community.
iii. Share best practices with other businesses, chambers of commerce,
and associations to improve community response efforts.
Appendix III
Sources of Guidance
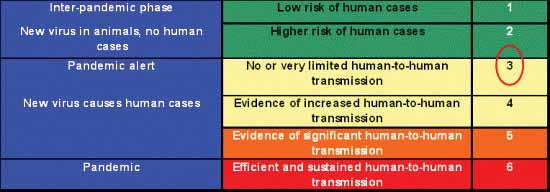
Global Cycle of Avian Influenza Viruses in Animals
Avian Influenza refers to different influenza viruses that affect birds. They circulate naturally among wild birds
and waterfowls. Occasionally, a strain may jump to domesticated birds, and mammals including humans.
WHO Influenza Pandemic Phases
An Avian Influenza may establish as human influenza and cause pandemics. The World Health Organization has
described six phases in the development of a pandemic to facilitate preparedness planning. Currently we are in
pandemic alert- phase 3.
Source: http://www.caymanprepared.ky/portal/pls/portal/docs/1/9348171.PDF
Athenea Digital - 14(3): 79-103 (noviembre 2014) -ARTÍCULOS- LA VIOLENCIA DE GÉNERO EN LA INTERVENCIÓN PSICOSOCIAL EN QUITO. TEJIENDO NARRATIVAS PARA CONSTRUIR NUEVOS SENTIDOS GENDER BASED VIOLENCE AND PSYCHOSOCIAL INTERVENTION AT QUITO. WEAVING NARRATIVES TO CONSTRUCT NEW MEANINGS Departament de Psicologia Social - Universitat Autònoma de Barcelona;
Romanian Neurosurgery (2012) XIX 1: 63 – 66 63 Primary tuberculomas of the thoracal spinal cord. Case report D. Balasa1, A. Tunas1, A. Terzi2, C. Serban4, M. Aschie3 Clinical Emergency County Hospital, Constanta 1Neurosurgery, 2Anestesiology, 3Pathology 4 Euromedic Private Unit, Constanta, Neuroradiology Abstract intramedullary tuberculoma. We present