Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Wjes.org
Yahya et al. World Journal of Emergency Surgery 2014, 9:12http://www.wjes.org/content/9/1/12
WORLD JOURNAL OF EMERGENCY SURGERY
The role of emergency surgery in hydatid liverdisease
Ali I Yahya*, Hussen E Shwereif, Mustafa A Ekheil, Ahmed S Thoboot, Kalid A Algader, Fatma O Gyaedand Abdsalem S Aldarat
Hepatic hydatid disease is very common in Libya. In Zliten hospital, we operated 400 patients with hepatic hydatidcysts over period of 20 years. All patients were symptomatic. Their ages varied from 3 to 85 years including 215female and 185 male patients. Their symptoms varied from abdominal pain to abdominal mass 67 patients wereadmitted through Accident and Emergency Department with acute presentations including fever, skin rash,jaundice and shock with acute abdominal pain. Those 67 patients had necessary investigations, resuscitation andunderwent emergency surgery. The hepatic cysts in all patients were excised, and the obstructive jaundice wascleared in those patients with obstructive jaundice. Unfortunately, one of the patients died two days after thesurgery because of multiple organ failure (MOF) Morbidity was wound Infection, bile leak and recurrence rate wereall reported in our series.
Keywords: Liver, Hydatid disease, Emergency surgery
Methods and materials
Hydatid is a disease caused by tape worm called ecchi-
The files of the patients were reviewed retrospectively.
nococcous granulosis and ecchinococcous multilocularis.
Four hundred patients were operated at the general
Hydatid disease is endemic in some regions in the world
surgery department at Zliten hospital while sixty seven
and Libya is one of the endemic countries of hydatid dis-
patients were operated as emergency because of their
ease among the Middle East countries. This disease is
acute presentations, the research was approved by the
common in sheepherder regions. Thus people who live
research and ethical committee in the hospital.
thereare accidentally infected. Dogs are the definitive
67 patients were admitted through Accident and
host and sheep is the intermediate host. Human gets the
Emergency Department. One of them was shocked and
infection by eating contaminated vegetables by dogs'
admitted to the surgical ICU. All the patients came
waste or by direct contact with dogs. Infection rate is
from endemic areas of hydatid disease. Routine investi-
higher in places where dogs are fed with infected car-
gations were done including complete blood count,
casses and offal. Liver is the commonest organ involved
blood group, blood sugar, urea and electrolytes. Liver
in human as well as lung, kidneys,spleen, bones and soft
function tests and ultrasound scan were done for all
tissues. Symptoms depend on the size of the cyst, the
patients. CT scan was also performed for most of the
organ involved and the complications from the cyst.
patients. All the patients had intravenous fluid, antibi-
The diagnosis of hydatid liver disease depends on history
otics, analgesia and hydrocortisone.
and clinical examination. Using imaging investigations is
All patients had laparotomy at same day. The opera-
very valuable to confirm the diagnosis including ultrasound
tions were done under general anesthesia through right
scan and CT scan. While serological investigations are not
subcostal incision. Precautions were taken to prevent
needed in endemic area, surgical intervention is the main
spillage of the cyst content. Intraoperative ultrasound
way to treat hepatic hydatid cysts.
was done routinely for all patients to find out the exactnumber of cysts. The duration of surgeries varied from
* Correspondence:
one and half an hour to three hours. All the cysts were
General surgery department, Zliten Teaching Hospital and Edwaw District
Hospital, Zliten, Libya
2014 Yahya et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the CreativeCommons Attribution License which permits unrestricted use, distribution, andreproduction in any medium, provided the original work is properly credited.
Yahya et al. World Journal of Emergency Surgery 2014, 9:12
and rigid. The patient had resuscitation including IV fluid,
Group A - 45 patients were presented with abdominal
IV hydrocortisone and IV analgesia. He had routine inves-
pain and obstructive jaundice. Blood tests showed high
tigation and the ultrasound scan showed hydatid cyst liver
bilirubin and alkaline phosphates while other blood tests
in the left lobe with a lot of fluid in the abdomen. The pa-
were normal. The ultrasound showed hepatic hydatid cysts.
tient had laparotomy and there was a big hydatid cyst at
23 patients were with single big cyst with no daughter
the left lobe which was ruptured. With excision of the cyst
cysts. All cysts were near to the hilum with size ranges
and cleaning of the abdominal cavity, the patient im-
from 10 to 15 cm. In 9 patients, the cysts were in the left
proved and discharged in good conditions.
lobe and in the other 14 patients, they were in the right
Group E - Ten patients were admitted with abdominal
lobe. Bile ducts were normal in size.
pain and fever. They had ultrasound scan which showed
In 22 patients, the ultrasound showed cysts with mul-
hydatid cysts of the liver. In seven patients, the cysts
tiple daughter cysts. In twenty one of them, the cysts
were at the right lobe and in three patients at the left
were in the right lobe and in one patient, the cyst was in
lobe. Laparotomy was performed for all of them. The
the left lobe. The size of cysts ranges from 8 to 15 cm.
cysts were full of pus, and the cyst cavity was completely
MRCP was done for two patients and it showed clear
cleared. Drain was inserted and the patients were cov-
communication between the cyst and the biliary tree.
ered with antibiotics. Patients improved and discharged
Preoperative ERCP was done for one patient who was in
in good conditions.
septicemia and renal impairment. 23 patients, with their
Group F - A female Patient was 35 years old was ad-
cysts near the hilum, were excised and the fluid in the
mitted with dyspnea and chest pain. On clinical examin-
cyst was clear. There were no bile and no daughter cysts
ation, the patient looked pale and dyspnic with rapid
but only single endocyst. There was no bile duct com-
pulse and decrease air entry on the right side of the
munication and the cyst cavity was completely closed.
22 patients were with cysts at the right and the left
X-ray of the chest showed that the right side was
lobe of the liver. Those cysts contain multiple daughter
pleural effusion. The ultrasound of the abdomen showed
cysts. Some of them contain bile stained fluid. After re-
huge hydatid cyst in the right lobe of the liver with a lot
moval of all daughter cysts, there were communications
of daughter cysts in the right chest cavity. The CT scan
with bile ducts. With the use of the Fogarty catheter,
of abdomen and chest confirmed the finding of hydatid
daughter cysts and membranes came out. We flushed
cyst liver ruptured into chest. The patient had routine
the bile ducts with huge amount of saline and the com-
investigations and urgent surgery. The finding was a
munication was closed with 2/0 PDS.
huge cyst in the right lobe of the liver full of daughter
Group B -Two patients (one is male 18 years and the
cysts and bile, ruptured into the chest cavity. Wound ex-
other is female 24 years old) were presented with swell-
tended into the right thoracotomy and the hepatic cyst
ing at anterior abdominal wall. Both the swellings were
was excised and the fistula closed washing the pleural
tender red, ultrasound findings in both patients showed
cavity. Drains were inserted and common bile duct was
that hydatid cyst liver communicating with the abdom-
cleared from daughter cysts. The patient discharged in
inal swellings which were cystic. Both patients had
good conditions.
laparotomy and excision of the hydatid cysts and the
Group G - Two patients had laparotomy for hepatic
abscess track. Both patients cured and discharged in
hydatid cyst (one of them was male 18 years and the
good conditions.
other was female 25 years old). The male Patient was
Group C - Six patients were admitted with skin rashes
diagnosed with huge right hepatic lobe hydatid cyst.
all over the body. Two of them were males and the
MRCP showed big communication with cyst and the
others were females ageing between 16 to 25 years.
patient was not jaundiced. He had a laparotomy and ex-
General conditions were stable and their blood pressure
cision of the cyst. The communication with bile duct
was within normal. On abdominal examination, there
was closed and the patient discharged in good condi-
was guarding and tenderness all over the abdomen. The
tions. After 10 days from the surgery, the patient came
ultrasound examination showed huge hydatid cysts in
back to the hospital with abdominal pain. He looked
the liver and all were in the right lobe with free fluid in
dehydrated, sick and hypotensive. Routine investigations
the abdomen. 6 patients underwent urgent laparotomy
showed leucocytosis and raised bilirubin 3.3 mg with a
and excision of the hydatid cysts. There was leak from
slight increase of alkaline phosphates. The ultrasound
the cysts into the abdominal cavity, but patients im-
showed that the abdomen was full of fluid. The patient
proved and discharged in good conditions.
had IV fluid, IV antibiotics and laparotomy was done.
Group D - One patient was admitted to Intensive Care
The abdomen was full of bile and it was cleaned com-
Unit with shock. On examination, patient looked sick, pale
pletely. There was a leak from the cyst cavity and a
and tachycardiac with low BP. Abdomen was guarding
big drain was inserted into the cyst cavity. Then the
Yahya et al. World Journal of Emergency Surgery 2014, 9:12
abdomen was closed and the patient improved and dis-
Discussion and conclusion
charged in good conditions.
Sixty seven patients with hepatic hydatid cysts were ad-
The female patient had laparotomy for the hydatid cyst
mitted through Accident and Emergency Department of
liver. After three days, she developed severe abdominal
Zliten hospital with acute symptoms. They were oper-
pain. On examination, the abdomen was guarding and
ated urgently and their presentations were as follow:
tender. The ultrasound showed plenty of fluid in the ab-domen. The patient was sick and urgent laparotomy was
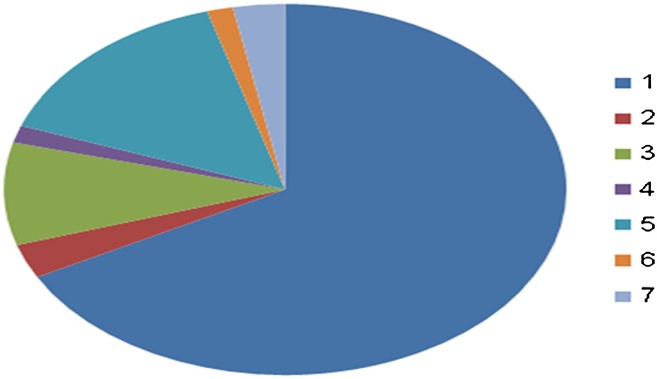
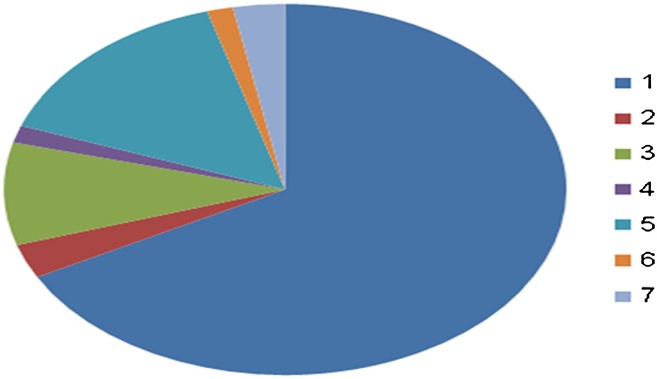
A. 45 patients with obstruction jaundice.
done to her. The abdomen was full of bile, it was washed
B. 2 patients with abdominal wall abscess.
with plenty of saline and a big drain was inserted in the
C. 6 patients with skin rash.
cyst cavity. And the patient improved and discharged in
D. 1 patient with anaphylactic shock.
good conditions.
E. 10 patients with liver abscess.
Sixty seven patients with hepatic hydatid cysts were
F. 1 patient with biliopleural fistula.
admitted to our surgery ward with acute presentations
G. 2 patients with biliary peritonitis following hepatic
included obstructive jaundice which was 11.25% of the
hydatid cystectomy.
total hydatid liver cysts operated in our institute. Sixpatients were presented with skin rash and acute ab-
Liver is the commonest organ gets infected by ecchinoco-
dominal pain was 1.25% of the total patients admitted
cous granulosis. The cyst can be asymptomatic discovered
and operated in Zlien hospital. Two patients were
on routine ultrasound examination of the abdomen, or
treated in the hospital with abdominal wall abscess
symptomatic like abdominal mass or abdominal pain
which is fistula with hydatid liver cyst which was 0.5%.
Hepatic cyst can be seen or discovered as organized cyst
While ten patients were presented with liver abscess
during investigations or other abdominal operations. In
which was 2% of the total patients treated. One patient
endemic areas, any patient, comes with the right upper ab-
was presented with anaphylactic shock and another
dominal mass, is considered infected with hydatid cyst liver
patient with bilipleaural fistula. Whereas another two
until it is proved otherwise. Surgery is the main treatment
patients were presented with peritonitis followed hep-
for hepatic hydatid cyst. Most of our patients were treated
atic hydatid cyst excision. Those sixty seven patients
electively. Sixty seven patients (67) with acute symptoms
underwent resuscitation and routine necessary investi-
were operated urgently to avoid complication such as rup-
gations. All of them had urgent surgery and hepatic
ture which was reported in the literatures of the patients
cysts were excised. One of the patients died after two
Different nonsurgical treatment was performed like
days from the surgery due to multiple organ failure.
pair technique in different centers, but none of our patients
The main hospital stay is 6 days. The morbidity noticed
was candidate for pair technique Medical treat-
among 400 operated patients. 6% of them suffered
ment like albendazole (antihelmentic) is used in treatment
from bile leak, 4% with wound infection and 2% with
of hepatic hydatid cysts. Some centers used the medical
recurrence (Figure
treatment and good results were observed. But in our cen-ter, we did not report significant benefits of medical treat-ment. We used albendazole preoperative and postoperativeto prevent recurrence and antihelmintic. Medical treatmentis not beneficial for patients with acute presentation wheretime makes difference in management. We also used med-ical treatment postoperatively for our patients to preventrecurrence. Sixty seven patients who came to the Accidentand Emergency Department had routine investigations andultrasound scan, and they were treated by urgent laparot-omy through the right Kocher incision. Patients of groupA, with obstructive jaundice, the obstruction was done bycompression on bile duct from outside and obstructionfrom inside by daughter cysts and parasitic membraneNone of the patients had preoperative ERCP
Figure 1 Distribution of patients presentations. A-45 patients
Only four of them had ERCP postoperatively for continu-
with obstruction jaundice. B-2 patients with abdominal wall abscess.
C-6 patients admitted with skin rash. D-One patient with anaphylactic
ous bile leak through the drain. ERCP will not cure them
shock. E-10 patients with liver abscess. F-1 patient with biliopleural fistula.
but it will only clear the bile ducts from intraductal obstruc-
G-2 patients with biliary peritonitis following hepatic hydatid cystectomy.
tion by daughter cysts or parasitic membrane and will relief
Group A=1, Group B=2, Group C=3, Group D=4, Group E=5, Group F=6,
the jaundice before surgery. The patient will still need
surgery to cure him or her from the disease. We explored
Yahya et al. World Journal of Emergency Surgery 2014, 9:12
the common bile duct through the communication with
Accident and Emergency Department. Those patients were
the cyst for those in whom the obstructive jaundice is intra-
sick and they had the investigations and treatment done ur-
ductal. But those in whom the obstruction is extra ductal
gently. They were presented with different acute presenta-
the obstruction is cleared with excision of the cyst. We
tions such as obstructive jaundice, skin rashes, anaphylactic
reviewed the literatures of the patients. Most of the patients
shock, abdominal wall abscess, liver abscess, peritonitis and
underwent ERCP before surgery. Patients of group B suf-
biliopleural fistula. All of them had urgent surgeries and
fered from abdominal wall swelling due to fistulization of
could not be treated by medical or PAIR treatment. As
superficial laying hepatic hydatid cyst. Rare presentation
usual, the complications from emergency surgery were ex-
was also reported in literatures of patients with
pected to be more. But in this research, the rate of compli-
biliocutaneous fistula. Patients of group C were presented
cations were not much different from the patients operated
with skin rash and abdominal pain due to leakage of para-
electively. This is due to emergency surgery done at the
sitic fluid into the abdominal cavity which induced anaphyl-
right time for the right patient.
actic reaction due to antigen antibody reaction. Thosepatients had minimal leak where they did not go into
Competing interests
anaphylactic shock. All of them had intravenous fluid and
The authors declare that they have no competing interests.
hydrocortisone and underwent urgent laparotomy and
Authors' contribution
excision of hydatid cyst. While patients of group D were
All authors read and approved the final manuscript.
presented with anaphylactic shock due to hydatid cyst. Butthis was very rare. Among four hundred patients operated
Received: 12 March 2013 Accepted: 6 October 2013Published: 30 January 2014
in our institution, only three patients had anaphylacticshock, two of them had the shock during surgery and the
other patient was case reported as emergency presentation.
Grosso G, Gruttadauria S, Biondi D, et al: Worldwide Epidemiology of LiverHydatidosis Including the Mediterranean Area. World J Gastroenterol 2012,
The three patients were saved with use of intravenous
adrenaline and intravenous fluid. Patients of group E were
Kjossev K, Losanoff J: TNRC Classification for Liver Hydatid Cysts. Int Surg
presented with liver abscess and secondary infection
1998, 83:311–313.
Kjossev K, Losanoff J: Response to Comment on ‘Classification of Hydatid
by bacteria. Liver abscess was expected because of high
Liver Cysts'. J Gastroenterol Hepatol 2007, 22(4):604.
temperature patients were sick and dehydrated. The
Kjossev K, Losanoff J: Classification of Hydatid Liver Cysts. J Gastroenterol
ultrasound showed that the cyst contents were thick. Liver
Hepatol 2005, 20(3):35.
Kjossev K: Classification, Staging and Surgical Treatment. Sofia Bulgaria: PhD
abscess was confirmed by surgery. All the patients had anti-
biotics and only three of them had blood transfusion be-
Dakkak A: Echinococcosis/Hydatidosis: A Severe Threat in Mediterranean
cause of low hemoglobin. The patient of group F had very
Countries. Vet Parasitol 2010, 174(1–2):2–11.
Akcan A, Akyildiz H, Artis T, et al: Peritoneal Perforation of Liver Hydatid
rare presentation. The hepatic hydatid cyst infiltrated the
Cysts Clinical Presentation, Predisposing Factors, and Surgical Outcome.
diaphragm and opened in the pleura. Patients of group G
World J Surg 2007, 31(6):1284–1291.
had urgent surgeries. The two patients had biliary periton-
Dumnici A, Papiu H, Olariu T: Acute Surgical Abdomen Produced by anAbdominalized Infected Gigantic Hydatid Cyst. Case Reports. English
itis after hepatic hydatid cyst surgery. They were diagnosed
Abstract. J Article Chirurgia (Bucur) 2004, 99(3):181–184.
clinically and underwent urgent surgery. The usual time of
Durif S, Marinkovic Z, Febvre C, et al: Hydatid Liver Disease Revealed by
surgery varies from one hour to 3 hours and the patients
Surgical Acute Abdominal Syndrome. Case Reports, English Abstract,Journal Article. Arch Pediatr 2005, 12(11):1617–1619.
had excision of the cyst and closure of the cyst cavity. But
Gogia N, Sharma R, Gamangatti S, et al: Hepatic Hydatid cysts with biliary,
none of them had liver resection although they had big
and peritoneal rupture and transdiaphragmatic migration. Case reports,
drain inserted around the cyst area which left for 3 to
Journal article. Trop Gastroenterol 2006, 27(2):93–96.
Ghesquière F, Mourot N, Olivero de Rubiana JP, et al: Surgery of Hepatic
5 days. Emergency surgery gives quick answer to patient
Hydatic Cyst. Per-operative Complications. Possibility of Anaphylactic
with acute complain. Only one patient died. She had
Etiology. Case Reports, English Abstract, Journal Article. Anesth Analg
obstructive jaundice and died because of multiple organ
(Paris) 1979, 36(11–12):561–563.
Daradkeh S, EL-Muhtaseb H, Farah G: Predictors of Morbidity and Mortality
failure. We reported morbidity includes bile leak, wound
in the Surgical Management of Hydatid Cyst of the Liver. Arch Surg 2007,
infection, recurrence. Hospital stay was longer for patients
who had emergency surgery in comparison to elective
Kang MJ, Lee SH, Kim SJ, et al: A Case of Multiple Intraperitoneal CystsFrom Ruptured Hepatic Hydatid Cysts. Case Reports, English Abstract,
Journal Article. Korean J Gastroenterol 2007, 50(3):203–206.
Ozturk G, Aydinli B, Yildirgan MI, et al: Posttraumatic Free Intraperitoneal
Rupture of Liver Cystic Echinococcosis: a Case Series and Review ofLiterature. Journal Article 2007, 194(3):313–316.
Hepatic hydatid disease can be asymptomatic or symptom-
Haddad M, Al Awar G, Jalbout R, Kanj V, Elkattah R, Faraj W, Khalifeh MJ:
atic with usual symptoms either abdominal pain or abdom-
New Trends in the Management of Hepatic Echinococcusgranulosus.
inal mass. We reviewed our patients admitted and treated
Libya 2011, 59(3):154–159.
Filippou D, Tselepis D, Filippou G, Papadopoulos V: Advances in
in Zliten institution. Most of them were admitted and
LiverEchinococcosis: Diagnosis and Treatment. Clin Gastroenterol Hepatol
treated electively 67 patients were admitted through the
Yahya et al. World Journal of Emergency Surgery 2014, 9:12
Dziri C, Haouet, Fingerhut A: Treatment of Hydatid Cyst of the Liver:WhereIs the Evidence? World J Surgery 2004, 28(8):731–736.
Liver Echinococcosis, Consensus Statement of The National Conference,Sofia. 2003.
Papadimitriou J, Mandrekas A: The Surgical Treatment of Hydatid Diseaseof the Liver. Br J Surg 2005 XII, 57(6):431–433.
Nunnari G, Pinzone M, Gruttadauria S, et al: Hepatic Echinococcosis: clinicaland the Rapeutic Aspects. World J Gastroenterol 2012, 18–13:1448–1458.
Mandal S, Mandal M: Human cystic echinococcosis: epidemiologic,zoonotic, clinical, Diagnostic and Therapeutic Aspects. Asian Pac J TropMe 2012, 5(4):253–260.
Ivanov G: Modern Approach in Diagnosis and Surgical Treatment of Liver.
Echinococcosis in children and Adults. Varna, Bulgaria: PhD Dissertation;2012:182.
Lu SF, Li JZ: Cases of Hydatid Disease of the Common Bile Duct. JournalArticle. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing ZaZhi 2000,18(3):185.
Manterola C, Barroso M, Vial M, Bustos L, Muñoz S, Losada H, Bello N,Hernández F, Carrasco R: Liver Abscess of Hydatid Origin: Clinical Features andResults of Aggressive Treatment. 2003.
Prousalidis J, Kosmidis C, Kapoutzis K, et al: Intrabiliary Rupture of HydatidCysts of the Liver. Journal Article. Am J Surg 2009, 197(2):193–198.
Târcoveanu E, Vasilescu A, Moldovanu R, Vlad N, Rusu V, Stanciu C: UnusualForms of Liver Abscesses. Rev Med Chir Soc Med Nat Las, 112(3):688–697.
Coyle WJ: ERCP in Hepatic Hydatid Disease. [Comment, Journal Article].
Gastroenterol Rep 2004, 6(4):272.
Florea M, Barbu ST, Crisan M, et al: Spontaneous External Fistula of aHydatid Liver Cyst in a Diabetic Patient. Case Reports, Journal Article.
Chirurgia (Bucur) 2008, 103(6):695–698.
Losada H, Bello N, Hernández F, Carrasco R: Liver Abscess of Hydatid Origin:Clinical Features and Results of Aggressive Treatment. 2003.
Manterola C, Barroso M, Vial M, Bustos L, Muñoz S, Losada H, Bello N,Hernández F, Carrasco R: Liver Abscess of Hydatid Origin: Clinical Featuresand Results of Aggressive Treatment. ANZ J Surg 2003, 73(4):220–224.
doi:10.1186/1749-7922-9-12Cite this article as: Yahya et al.: The role of emergency surgery inhydatid liver disease. World Journal of Emergency Surgery 2014 9:12.
Submit your next manuscript to BioMed Central
and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution
Submit your manuscript at www.biomedcentral.com/submit
Source: http://www.wjes.org/content/pdf/1749-7922-9-12.pdf
Department of Health and Human Services OFFICE OF INSPECTOR GENERAL PART D BENEFICIARIES WITH QUESTIONABLE UTILIZATION PATTERNS FOR HIV DRUGS Daniel R. Levinson Inspector General August 2014 EXECUTIVE SUMMARY: Part D Beneficiaries With Questionable Utilization Patterns for HIV Drugs, OEI-02-11-00170
Published Ahead of Print on March 8, 2010 as 10.1200/JCO.2009.24.4798 JOURNAL OF CLINICAL ONCOLOGY Prediction of Risk of Distant Recurrence Using the 21-GeneRecurrence Score in Node-Negative and Node-PositivePostmenopausal Patients With Breast Cancer Treated WithAnastrozole or Tamoxifen: A TransATAC StudyMitch Dowsett, Jack Cuzick, Christopher Wale, John Forbes, Elizabeth A. Mallon, Janine Salter, Emma Quinn,Anita Dunbier, Michael Baum, Aman Buzdar, Anthony Howell, Roberto Bugarini, Frederick L. Baehner,and Steven Shak