Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Review article: vitamin d and inflammatory bowel diseases
Alimentary Pharmacology and Therapeutics
Review article: vitamin D and inflammatory bowel diseases
V. P. Mouli* & A. N. Ananthakrishnan†,‡
*Department of Gastroenterology, All
India Institute of Medical Sciences,
New Delhi, India.
†
Harvard Medical School, Boston,
Vitamin D is traditionally associated with bone metabolism. The immuno-
‡Division of Gastroenterology,
logical effects of vitamin D have increasingly come into focus.
Massachusetts General Hospital,Boston, MA, USA.
AimTo review the evidence supporting a role of vitamin D in inflammatory
Correspondence to:
bowel diseases.
Dr A. N. Ananthakrishnan, Crohn's &Colitis Centre, Massachusetts General
Hospital, 165 Cambridge Street, 9th
A comprehensive search was performed on PubMed using the terms
Floor, Boston, MA 02114, USA.
crohn's disease' ‘ulcerative colitis' and ‘vitamin D'.
ResultsVitamin D deficiency is common in patients with inflammatory bowel dis-
eases (IBD) (16–95%) including those with recently diagnosed disease. Evi-
Submitted 27 September 2013
dence supports immunological role of vitamin D in IBD. In animal models,
First decision 15 October 2013
Resubmitted 26 October 2013
deficiency of vitamin D increases susceptibility to dextran sodium sulphate
Accepted 28 October 2013
colitis, while 1,25(OH)2D3 ameliorates such colitis. One prospective cohort
EV Pub Online 17 November 2013
study found low predicted vitamin D levels to be associated with anincreased risk of Crohn's disease (CD). Limited data also suggest an associ-
This commissioned review article wassubject to full peer review and the
ation between low vitamin D levels and increased disease activity, particu-
authors received an honorarium from
larly in CD. In a large cohort, vitamin D deficiency (<20 ng/mL) was
Wiley on behalf of AP&T.
associated with increased risk of surgery (OR 1.8, 95% CI 1.2–2.5) in CDand hospitalisations in both CD (OR 2.1, 95% CI 1.6–2.7) and UC (OR 2.3,95% CI 1.7–3.1). A single randomised controlled trial demonstrated thatvitamin D supplementation may be associated with reduced frequency ofrelapses in patients with CD compared with placebo (13% vs. 29%,P = 0.06).
ConclusionThere is growing epidemiological evidence to suggest a role for vitamin Ddeficiency in the development of IBD and also its influence on diseaseseverity. The possible therapeutic role of vitamin D in patients with IBDmerits continued investigation.
Aliment Pharmacol Ther 2014; 39: 125–136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
ciation with pathogenesis and natural history of these
Ulcerative colitis (UC) and Crohn's disease (CD) consti-
tute chronic idiopathic inflammatory bowel diseases(IBD). The key underlying pathogenic mechanisms for
both diseases is a dysregulated host immune response to
A comprehensive literature search on Pubmed was con-
commensal intestinal flora in genetically susceptible indi-
ducted using the following search terms: ‘Crohn's dis-
viduals.1, 2 Known genetic variants incompletely explain
ease' ‘ulcerative colitis' and ‘vitamin D' to identify
the variance in disease incidence, suggesting a strong role
relevant English language articles published between
for environmental factors, supported by epidemiological
1966 and 2013. In addition, bibliographies of the
retrieved articles were searched to identify additional rel-
Vitamin D has long been recognised as a major regu-
evant articles.
lator of calcium and phosphorus metabolism and key inmaintaining bone health.5–7 However, several recent
studies have yielded new insights into the role of vitaminD in various other physiological processes. In particular,
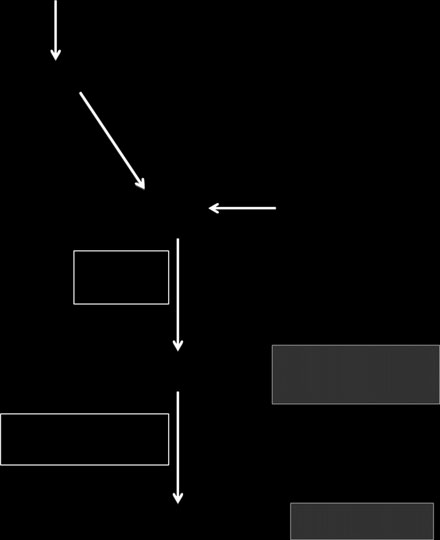
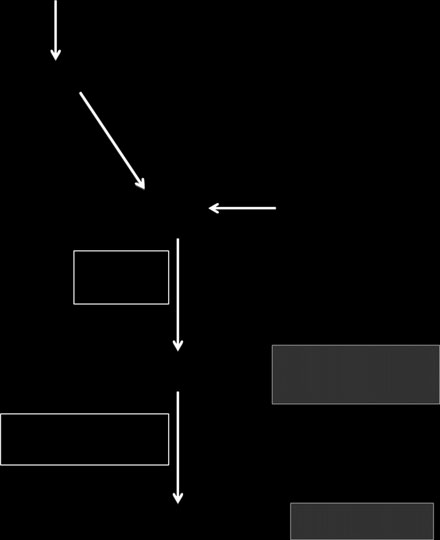
Vitamin D synthesis
vitamin D appears to play important roles in immune
The main source of vitamin D is endogenous production
regulation, particularly involving the innate immune
in the skin where ultraviolet B energy in the sunlight
system, cardiovascular and renal physiology, and devel-
converts 7-dehydrocholestrol to cholecalciferol (vitamin
opment of cancer.6 Importantly, an increasing body of
D3) (Figure 1).5, 14 Dietary contribution to vitamin D
literature supports an important role of vitamin D in the
status includes foods such as egg yolk, beef liver, cod
pathogenesis as well as potential therapy of IBD.8–13 The
liver oil, fatty fish, fortified milk and milk products.5
current review examines the evidence linking vitamin D
Vitamin D from the endogenous production on exposure
to IBD, both through its effect on bone health and asso-
to sunlight as well as that absorbed from diet is
7-dehydro cholesterol
UV exposure (Sunlight)
Dietary vitamin D
Major circulating form
25-hydroxy vitamin D3
(bound to vitamin D bindingprotein)
+ Parathormone (PTH)
(proximal tubules of kidney)
– Fibroblast growth factor 23
Figure 1 Metabolism of
Biologically active form
1,25-dihydroxyvitamin D3
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Review: vitamin D and inflammatory bowel diseases
metabolised within the liver to 25-hydroxyvitamin D (25
related to the underlying bowel disease, while others are
(OH)D) by the enzyme vitamin D 25-hydroxylase. 25
in common with the non-IBD population. These include
(OH)D is the major circulating form of vitamin D and is
inadequate exposure to sunlight either related to lifestyle
also used to determine the status of vitamin D in clinical
or persistent symptoms of active disease restricting phys-
practice. 25(OH)D is biologically inactive and is activated
ical activity, inadequate dietary intake due to symptoms
within the proximal tubules of nephrons in the kidneys
of bowel disease, impaired absorption, impaired conver-
by the enzyme 25-hydroxyvitamin D-1alpha-hydroxylase
sion of vitamin D to its active products, increased catab-
(also known as CYP27B1) to 1,25-dihydroxyvitamin D
olism and increased excretion.5, 7 That inadequate
(1,25(OH)2D). The renal synthesis of the active biologi-
exposure to sunlight is an important cause of vitamin D
cal product of vitamin D (1,25(OH)2D) is regulated by
deficiency in patients with IBD is supported by evidence.
various factors including serum calcium and phosphorus
Several studies, particularly from northern climates, have
levels, parathormone and fibroblast growth factor 23.15
consistently demonstrated an association between vita-min D deficiency and winter season, a period of likely
Prevalence of vitamin D deficiency in IBD
low sunlight and UVB exposure.13, 21, 22 Insufficient die-
While it is relatively easy to ascertain macronutrient
tary consumption also contributes to low vitamin D in
deficiency clinically, micronutrient deficiency may not
some patients with IBD. In a detailed nutritional survey
always be clinically evident and usually requires labora-
of 126 IBD patients, inadequate vitamin D consumption
tory testing. The best measure of an individual's vitamin
was found in 36% of patients and suboptimal serum
D status is serum 25(OH)D.5, 7, 16 Serum 25(OH)D lev-
vitamin D levels were found in 18% of patients.23 Oral
els of less than 20 ng/mL (50 nmol/L) indicate vitamin
intake correlated significantly with serum levels in CD
D deficiency. Serum 25(OH)D levels between 21 and
and with all IBD in remission.23 While other small stud-
29 ng/mL (52.5 and 72.5 nmol/L) represent vitamin D
ies suggested no correlation between dietary vitamin D
insufficiency, while levels between 30 and 100 ng/mL (75
intake and serum 25(OH)D in CD patients, they may
and 250 nmol/L) represent normal values.5, 7, 16 Several
have been limited by lack of statistical power.24
studies have reported a high prevalence of vitamin D
Fats and fat-soluble vitamins are absorbed after emul-
deficiency in patients with IBD, although it has not been
sification by bile acids. The bile acid pool is maintained
universally established that this rate is higher than in
by an enterohepatic circulation occurring from the ter-
other chronic illnesses, inflammatory diseases, or even
minal ileum. Interruption of the enterohepatic circulation
health individuals in that region (Table 1). Levin et al.
(e.g., by terminal ileal resection) could theoretically con-
reported vitamin D deficiency in 19% and insufficiency
tribute to vitamin D deficiency. However, clinical data in
in 38% of children with IBD in a cohort predominantly
support of this are conflicting. Terminal ileal resection
consisting of patients with CD.17 In contrast, Alkhouri
was associated with vitamin D deficiency in some stud-
et al. reported that the prevalence of vitamin D defi-
ies.25, 26 In a study of 12 CD patients who underwent
ciency in children with IBD (62%) was lower than the
terminal ileal resection, absorption of vitamin D was
rate in their controls (75%).18 In a large, retrospective
reduced with the decline in absorption correlating with
study of adult patients with IBD from Wisconsin (101
the length of the resected segment. However, other stud-
UC, 403 CD), nearly 50% of the patients had vitamin D
ies failed to identify an effect of ileal resection or active
deficiency and about 11% of patients had severe vitamin
disease.19 Malabsorption may theoretically contribute to
D deficiency,19 a frequency estimate that is consistent
low vitamin D in CD patients as vitamin D is absorbed
with other published IBD cohorts.13 While most studies
in the proximal part of small intestine. The prevalence of
have examined prevalence in patients with well estab-
vitamin D deficiency is higher in CD patients with upper
lished IBD, deficiency of vitamin D does not appear to
gastrointestinal tract involvement.27 However, when
be consequent to long-standing disease alone. In a
absorption of vitamin D was specifically tested, only 10%
cohort of newly diagnosed IBD patients from Manitoba
of patients with CD had decreased absorption of vitamin
providence in Canada, only 22% were found to have suf-
D compared to 50% of patients with pancreatic insuffi-
ficient levels of vitamin D.20
ciency.28 There also appears to be a wide variation inabsorption of vitamin D in patients with CD even in
Causes of vitamin D deficiency in patients with IBD
those with quiescent disease.29 Protein-losing enteropa-
There are several factors contributing to vitamin D defi-
thy occurs in some patients with IBD. As vitamin D and
ciency in patients with IBD, some causes specifically
its metabolites circulate predominantly as bound forms
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
Table 1 Prevalence of vitamin D deficiency in unselected cohorts of patients with inflammatory bowel diseases
65% of patients had low serum 25(OH)D25% had levels below 10 ng/mL
27% of CD patients had 25(OH)D levels <30 nmol/L
15% of UC patients had 25(OH)D levels <30 nmol/L
Mean 25(OH)D was lower in IBD patients (18.7 mcg/L) compared with controls
(28.5 mcg/L) (P < 0.05)
16% of CD patients had vitamin D < 38 nmol/L
22% had 25(OH)D levels <40 nmol/L8% had 25(OH)D levels <25 nmol/L
27% of CD patients were deficient (25(OH)D < 10 ng/mL) compared to
During late-summer, 5% of controls and 18% of CD patients were deficient
During late-winter, 25% of controls and 50% of CD patients were deficient
50% were vitamin D deficient during winter (<50 nmol/L) and 19%
were deficient during summer
Prevalence of vitamin D deficiency (25(OH)D < 15 ng/mL) was 35%
88% had serum 25(OH)D levels below 75 nmol/L
Mean 25(OH) levels were lower in CD patients (11 ng/mL) compared with
those with UC (20 ng/mL) (P < 0.001)
25(OH)D levels were lower in CD patients (16 ng/mL) compared with controls
50% of patients had 25(OH)D < 30 ng/dL, 11% had levels below 10 ng/dL
Vitamin D insufficiency (<20 ng/mL) was seen in 31% of patients with CD
and 28% of UC patients
19% of patients were deficient in vitamin D (<51 nmol/L)
37% had vitamin D deficiency
63% of patients with CD were deficient (<50 nmol/L)
39% of the entire cohort had low vitamin D (<50 nmol/L); this was more
frequent in 43% of CD and 37% of UC patients
30% of patients with CD had levels below 37.5 nmol/L compared
to 37% of controls
95% of patients had deficient vitamin D levels (25(OH)D < 30 ng/mL)
28% had insufficient (20–30 ng/mL) and 32% had deficient (<20 ng/mL) levels
62% of patients had low vitamin D levels compared to 75% of controls
IBD, inflammatory bowel diseases; CD, Crohn's disease; UC, ulcerative colitis, IC, indeterminate colitis.
* Paediatric cohorts.
to plasma vitamin D binding protein (DBP), the loss of
tion study of nearly 30 000 individuals of European des-
DBP along with the bound vitamin D could be an addi-
cent, variants at three loci near the genes involved in
tional plausible mechanism of vitamin D deficiency, par-
cholesterol synthesis, vitamin D hydroxylation and vita-
ticularly in those with severe disease. Finally, recent
min D transport were associated with vitamin D insuffi-
studies have suggested that genetic variants contribute
ciency.30 The contribution of such genetic variants to
both to development of vitamin D insufficiency and
vitamin D status in patients with IBD has not yet been
response to supplementation. In a genome-wide associa-
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Review: vitamin D and inflammatory bowel diseases
Role of vitamin D in bone turnover and mineral
Vitamin D and innate immunity
Vitamin D receptor is ubiquitously expressed in several
Vitamin D helps to maintain calcium homoeostasis by
human tissues including immune cells, keratinocytes,
acting on the small intestine epithelium and osteoblasts.
pancreatic beta-cells, cardiac myocytes, central nervous
1,25(OH)2D acts mainly through the nuclear vitamin D
system, renal tubules and the intestine. Many of these
receptor (VDR), which forms a heterodimer with a reti-
tissues also contain the enzymes for conversion of vita-
noid X receptor, binds to the vitamin D response ele-
min D to its active metabolites, supporting a widespread
ment and recruits co-activators and enzymes with
extraskeletal role of vitamin D.45 Vitamin D appears to
histone acetylation activity, thereby regulating gene
have an important role in innate immunity as well as
expression.10, 31–33 25(OH)D interacts with the VDR in
adaptive immunity.10, 33 It acts as a key link between
the small intestinal epithelium and augments the
toll-like receptor (TLR) activation and antibacterial
absorption of calcium and phosphorus from the small
responses in innate immunity. Activation of TLRs on
intestine.34 1,25(OH)2D also interacts with the VDR on
macrophages by a Mycobacterium tuberculosis derived
osteoblasts and increases the surface expression of
lipopeptide leads to upregulation of conversion of 25
Receptor Activator for Nuclear Factor jB ligand
(OH)D to the active 1,25(OH)2D, upregulation of VDR
(RANKL), which, after binding with RANK on pre-os-
expression and induction of downstream targets of VDR
teoclasts, converts them into osteoclasts.35, 36 Osteoclasts
including cathelicidin, an antimicrobial peptide.46 1,25
function in dissolution of bone matrix and mobilise cal-
(OH)2D also acts synergistically with activated NF-jB to
cium stores into circulation, thus helping in the mainte-
induce expression of b-defensin 4 gene.47 Supplementa-
nance of calcium homoeostasis. Dissolution of bone
tion with vitamin D in individuals with insufficient
matrix by osteoclasts is an essential part of bone
serum levels of 25(OH)D leads to induction of cathelici-
din, thus enhancing the innate immune defences against
Vitamin D deficiency leads to reduction in serum lev-
microbial agents.48
els of ionised calcium leading to secondary hyperpara-
Autophagy plays an important role in the pathogene-
sis of CD, and several lines of evidence support the
disproportionate increase in bone resorption, osteopenia
hypothesis that the effect of vitamin D on IBD patho-
and osteoporosis.37 In children, vitamin D deficiency
genesis may be through this pathway. 1,25 (OH)2D helps
results in poor mineralisation of the epiphyseal growth
in autophagy in macrophages by enhancing the co-locali-
plates leading to bone deformities and stunted longitudi-
sation of pathogen harbouring phagosomes with auto-
nal growth, which are the typical features of rickets. In
adults with vitamin D deficiency, there is defective min-
Similar induction of autophagy by vitamin D has also
eralisation of the newly formed bone collagen matrix
been demonstrated in several models of cancer cell lines.
resulting in osteomalacia which manifests as bone pain,
Vitamin D3 has been hypothesised to regulate autophagy
fractures and proximal muscle weakness.5, 7, 16
at several steps.50 Increased calcium absorption mediated
There is a high prevalence of metabolic bone disease
by the effect of vitamin D3 on the VDR can activate
in patients with IBD. The prevalence of osteopenia
autophagy through various calcium-dependent kinases
ranges from 23% to 67% and osteoporosis from 7% to
and phosphates, while vitamin D3 can itself downregu-
35% among patients with CD or UC.38–40 Active
late the expression of mTOR, a negative regulator of
inflammatory disease is a strong risk factor for low
autophagy.50, 51 Vitamin D3 can also induce autophagy
bone mineral density (BMD) in patients with IBD, with
through increasing beclin-1 expression, a regulatory of
BMD improving with increasing duration of remis-
autophagy, and activating the PI3K signalling path-
sion.41 This is supported by the known effect of TNF-a
way.50–52 Vitamin D has been long used to treat myco-
and other pro-inflammatory cytokines like IL-1, IL-6,
infections46, 53, 54
IL-17 in activating osteoclasts.42, 43 In addition, gluco-
supplementation may reduce likelihood of tuberculin
corticoids use is an important risk factor for bone loss
conversion.55, 56 In a randomised controlled trial, vita-
in patients with IBD.39 However, the data linking vita-
min D supplementation was associated with a reduced
min D deficiency and impaired BMD in patients with
rate of development of a positive tuberculin reaction,
IBD have been conflicting, with some studies support-
suggesting a protective effect against tuberculosis infec-
tion in an endemic population.56 Low serum vitamin D
effect.20, 39, 44
is also associated with reduced immunoreactivity to an
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
anergy panel, and supplementation with vitamin D in
link between polymorphisms in the VDR gene region on
anergic individuals with deficient levels restored delayed
chromosome 12 to development of IBD,10, 68–70 although
not all cohorts have yielded positive results. Variations
Vitamin D also plays a role in preventing over-activa-
in the DBP were also found to be associated with IBD.71
tion of pro-inflammatory responses. 1,25(OH)2D within
Few studies have been able to examine the association
the monocytes dose-dependently inhibits lipopolysaccha-
between vitamin D status and incident IBD directly. One
ride (LPS)-induced p38 phosphorylation and production
such study was using the Nurses' Health Study, a cohort
of IL-6 and TNF-a in LPS-stimulated monocytes.58 Anti-
of female registered nurses in the United States, followed
gen-presenting cells, including dendritic cells, express
prospectively using biennial questionnaires, and compre-
VDR.59 The action of 1,25(OH)2D on dendritic cells
hensive assessment of diet and supplement intake and
leads to a tolerogenic phenotype, thus protecting against
physical activity during the cohort follow-up timeline.8
autoimmune type 1 diabetes in adult non-obese diabetic
The vitamin D status of the participants was defined
mice.60 Maturation of dendritic cells is prevented by the
using a validated regression model incorporating race,
interaction of 1,25(OH)2D with VDR on the dendritic
diet, physical activity and region of residence. Over a
22-year follow-up, higher predicted plasma 25(OH)D le-ves was associated with a significant reduction in the risk
Vitamin D and adaptive immunity
of incident CD, but not UC.8 Compared to women with
Vitamin D receptor is expressed in mitotically active T
the lowest quartile of plasma vitamin D, those in highest
and B lymphocytes.62 1,25(OH)2D acts on helper T cells
quartile had a reduced risk of CD (HR 0.54, 95% CI
(TH cells), inhibits production of IL-2 and immunoglob-
0.30–0.99).8 For each 1 ng/mL increase in the plasma
ulin synthesis by TH cell regulated B lymphocytes.63 Reg-
level of 25(OH)D, there was a 6% relative risk reduction
ulatory T cells (Treg), which are responsible for
for CD. There was also an inverse association between
maintenance of tolerance to self-antigens, are also modu-
vitamin D intake from dietary sources and supplement
lated by 1,25(OH)2D.10, 33 Although the effect of vitamin
and the risk for incident UC; each 100 IU/day increase
D on B cells is predominantly through modulation of
in total vitamin D intake was associated with a 10% rela-
T-cell function, recent evidence suggests that 1,25
tive reduction in the risk of UC.8
(OH)2D may also act directly on the B cells, affectingthe proliferation of activated B cells and inhibiting the
Relationship of vitamin D levels and IBD disease
generation of plasma cells and post-switch memory B
In tune with its immune-modulating effects, vitamin Dmay also influence severity of inflammation in IBD.
Role of vitamin D in the immunopathogenesis of IBD
Vitamin D deficiency causes more severe growth retarda-
Several lines of epidemiological and laboratory evidence
tion and weight loss and also led to higher mortality in
support a role for vitamin D in the pathogenesis of IBD.
IL-10 KO mice colitis.72 Disease severity correlated with
First, there is a north–south gradient in IBD incidence, a
vitamin D status in mice with DSS-induced colitis; both
gradient that parallels UV exposure and consequently
local as well as endocrine effects of 1,25 (OH)2D affect
vitamin D levels. In a study by Khalili et al., residence in
the disease severity.73 TNF-a plays a central role in
Southern latitudes of the United States, particularly at
inflammation. 1,25(OH)2D reduces the severity of colitis
age 30 was associated with a significantly lower risk of
in IL-10 KO mice by downregulating several genes asso-
CD [Hazard ratio (HR) 0.48, 95% CI 0.30–0.77] and UC
ciated with TNF-a.74 When mice with tri-nitro-benzene
(HR 0.62, 95% CI 0.42–0.90).65 This has been supported
sulphonic (TNBS) acid-induced colitis were treated with
by other studies that have modelled residential UV expo-
a combination of corticosteroids and 1,25 (OH)2D, the
sure and shown an inverse correlation between UV
improvement in disease activity paralleled downregula-
exposure and IBD incidence.66 Mice lacking VDR are
tion of TH1 inflammatory cytokines profile as well as
more susceptible to dextran sodium sulphate (DSS)-in-
TH17 effector functions along with the promotion of TH2
duced mucosal injury compared with the wild type
and regulatory T-cell profiles.75
mice.67 The disruption in the epithelial junctions was
Data supporting a clinical association between vitamin
severe in mice lacking VDR and 1,25(OH)2D preserved
D deficiency and disease activity in IBD are conflicting
the integrity of the tight junctions in Caco-2 cells mono-
(Table 2). Neither El-Matary et al. nor Levin et al. found
layers.67 Genetic epidemiological studies have suggested a
a correlation between vitamin D levels and disease
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Review: vitamin D and inflammatory bowel diseases
Table 2 Observational studies of the association between vitamin D levels and outcomes in Crohn's disease andulcerative colitis
negatively correlatedwith disease activity(correlationco-efficient
Vitamin D levels were
not associated with
Vitamin D deficiency
was associated with l
ower HRQoL( 2.2, 95% CI
increased diseaseactivity (1.1, 95%CI 0.4–1.7) in CD,but not in UC
Vitamin D deficiency
(<20 ng/mL) was
increased risk ofsurgery (OR 1.8,95% CI 1.2–2.5) inCD and hospitalisationsin both CD (OR 2.1,95% CI 1.6–2.7) andUC (OR 2.3, 95%CI 1.7–3.1)
Patients with low
within 3 months of
anti-TNF initiation
increased risk of
early cessation of
CD, Crohn's disease; UC, ulcerative colitis; IBD, inflammatory bowel disease; HBI, Harvey Bradshaw index; PCDAI, Paediatric Cro-hn's disease activity index; PUCAI, paediatric ulcerative colitis activity index; SCCAI, simple clinical colitis activity index.
activity in cross-sectional studies of IBD cohorts.17, 76 In
increased risk of surgery [Odds ratio (OR) 1.76; 95% CI
contrast, a retrospective study by Ulitsky et al. concluded
1.24–2.51] and hospitalisation (OR 2.07; 95% CI 1.59–
that vitamin D deficiency was associated with lower heal-
2.68) compared with those with sufficient levels.13 Fur-
th-related quality of life and increased disease activity in
thermore, CD patients who normalised their plasma 25
patients with CD, but not with UC.19 Overcoming some
(OH)D had a reduced likelihood of IBD-related surgery
of the limitations engendered by cross-sectional assess-
(OR 0.56; 95% CI 0.32–0.98) compared with those who
ment of vitamin D and disease severity, we examined
remained deficient.13
prospectively the association between vitamin D defi-ciency and need for IBD-related surgery or hospitalisa-
Does vitamin D have a role in the treatment of IBD
tions in a large cohort of 3217 patients with at least one
There have been several studies examining the role of vita-
measurement of plasma 25(OH)D.13 We found that
min D as a therapeutic agent for IBD in animal models.77
plasma 25(OH)D < 20 ng/mL was associated with an
Vitamin D-deficient IL-10 KO mice spontaneously
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
develop an accelerated and severe form of IBD. However,
of anti-TNF treatment, with a more pronounced effect
when such mice were fed high-calcium diet and 1,25
on patients with CD.79 Miheller et al. compared the
(OH)2D, they developed only mild disease.72 Both in
therapeutic effects of 1,25(OH)2D and 25(OH) D in
TNBS- and DSS-induced colitis models, administration of
patients with CD with respect to disease activity and
1,25(OH)2D led to an improvement in disease activity and
bone health.80 There was a significant improvement in
addition of 1,25(OH)2D to a steroid regimen had a syner-
disease activity as well as bone metabolism in the short-
gistic effect and this combination most effectively reduced
term at 6 weeks with 1,25(OH)2D but not 25(OH)D.80
the disease severity.78 A novel vitamin D analogue withanti-proliferative effects and limited calcemic activity was
also found to alleviate disease activity in mice withDSS-induced colitis.78
There have been few human studies (Table 3). Jorgen-
Despite emerging promising data, there exist several lim-
sen et al. conducted a multicentre, randomised, dou-
itations in the literature regarding the role of vitamin D
ble-blind, placebo-controlled trial in Denmark evaluating
in IBD pathogenesis. First, while consistently supported
the efficacy of 1,25(OH)2D as a maintenance therapy in
by experimental animal models, the association between
CD patients in remission.12 One hundred and eight
low pre-diagnosis vitamin D and increased risk of CD
patients were randomised to receive either 1200 IU of
has been examined in a single prospective cohort study
1,25(OH)2D with 1200 mg of calcium or 1200 mg of cal-
that used a regression model to predict an individual's
cium alone daily over 1 year. Nearly one-third of the
vitamin D status. Ongoing analysis of pre-diagnosis
study population had vitamin D deficiency defined as
banked specimens from ongoing prospective cohorts as
serum 25(OH)D levels <50 nmol/L. Only 13% of
well as additional high-risk IBD cohorts will provide a
patients in the vitamin D group relapsed during the
more definitive answer to this hypothesis as randomised
1-year study period compared to 29% in the placebo
controlled trials of vitamin D in prevention of IBD are
group (P = 0.06).12 A second study by Zator et al. exam-
unlikely to be feasible, given relatively low incidence of
ined the influence of vitamin D status on response to
disease in the general population, and need for large
anti-TNF therapy. In a single centre cohort of patients
numbers of participants and long follow-up. The associa-
with CD and UC, plasma 25(OH)D levels measured
tion between low vitamin D and increased disease
within 3 months of initiation of anti-TNF therapy dem-
activity, particularly in CD, is also supported primarily
onstrated a significant inverse association with durability
Table 3 Interventional studies examining the effect of vitamin D supplementation on disease activity in Crohn'sdisease and ulcerative colitis
Number of patients
Mean CDAI decreased
patients treated with
of cholecalciferol
104 CD patients in
Relapse rate was lower
clinical remission
in patients treated with
compared to placebo(29%) (P = 0.06)
Vitamin D supplementation
mild-to-moderate CD
reduced CDAI scores from
230 to 118 (P < 0.0001), and
improved health-related
serum 25(OH)Dof 40 ng/mL
CD, Crohn's disease; CDAI, Crohn's disease activity index.
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Review: vitamin D and inflammatory bowel diseases
cross-sectional and unable to differentiate effect of vita-
three regimens for 6 weeks: 2000 IU daily of vitamin D2;
min D on disease activity from that of disease course on
2000 IU daily of vitamin D3; or 50 000 IU weekly of
vitamin D levels, more recent analyses of large cohorts
vitamin D2.83 It was found that the 6-week regimens of
have been able to prospectively demonstrate an associa-
50 000 IU of vitamin D2 per week and 2000 IU of vita-
tion between low vitamin D levels and increased risk for
min D3 daily were superior to vitamin D2 2000 IU daily.
surgery and hospitalisations, particularly in CD.13 How-
Whereas the regimen of 50 000 IU per week of vitamin
ever, only one randomised controlled trial has examined
D2 improved the serum 25(OH)D levels to more than
the role of vitamin D in preventing relapse, but was also
32 ng/mL in 75% of patients, only 38% of patients who
limited by small numbers.12 Effect of vitamin D supple-
received 2000 IU of vitamin D3 daily and 25% of patients
mentation in ameliorating disease activity in CD has
who received 2000 IU of vitamin D2 daily achieved
been examined only in two open-label pilot studies, and
serum 25(OH)D levels of more 32 ng/mL after 6 weeks
no studies have evaluated this in UC. Consequently,
of therapy. All the three regimens were found to be safe
there is an urgent need for high-quality randomised
and well tolerated.
intervention trials of vitamin D supplementation in bothCD and UC with disease activity as a treatment end
Future directions
Several unanswered question remain regarding the role ofvitamin D in IBD (Table 4). Further investigation is
Clinical practice
needed to understand the effects of dietary intake of vita-
Patients with IBD are at risk of developing vitamin D
min D and vitamin D supplementation in relation to poly-
deficiency. The Endocrine Clinical Practice Guidelines
morphisms of DBP or VDR to identify if there are
Committee recommends screening of patients with IBD
subgroups who may derive greater benefit from prophy-
as well as patients who are on corticosteroids for vitamin
laxis or who would require greater doses for treatment.
D status.16 While there is lack of professional guidelines
With recent evidence pointing towards vitamin D defi-
regarding subsequent assessments of vitamin D status, we
ciency as associated with IBD risk, confirmation of such
adopt the following in our practice. If the baseline vita-
findings in other cohorts would establish the vitamin D as
min D status is normal, it may be logical to consider
one of the links in the gene-environment-gut micro-
rechecking the status annually or biennially if there is
biome-immune system interactions necessary for the
active disease, if there is documented metabolic bone
development of IBD. It also merits investigation whether
disease or if there is continued use of systemic corticos-teroids. The Institute of Medicine and the Endocrine
Table 4 Unanswered clinical questions regarding the
Practice Guidelines Committee recommend a dietary
role of vitamin D in inflammatory bowel diseases
intake of 400 IU of vitamin D per day for infants, 600 IUof vitamin D per day for children beyond 1 year of age
1. Does low serum vitamin D cause Crohn's disease or
ulcerative colitis, or is it a marker for other risk factors?
and adults and 800 IU of vitamin D per day for the
2. Can supplementation with vitamin D in high-risk individuals
elderly aged above 70 years.82 However, to consistently
prevent or delay the onset of Crohn's disease or
raise the level of 25(OH)D to more than 30 ng/mL, espe-
ulcerative colitis?
cially in patients who are at risk for vitamin D deficiency,
3. Does vitamin D deficiency cause a more severe phenotype
or increased inflammatory activity in Crohn's disease,
the Endocrine Practice Guidelines Committee recom-
or is it merely a consequence of severity of disease? Is
mended that a maintenance dose of at least 1000 IU per
vitamin D status predictive of recurrence of Crohn's
day would be required.16 To treat documented vitamin D
deficiency, it is recommended to use either vitamin D2 or
4. What is the optimal role of vitamin D supplementation as a
vitamin D3 in a dosage of 2000 IU per day for 6 weeks,
therapeutic modality in patients with IBD?
Induction of remission?
or 50 000 IU once a week for 6 weeks in case of children
Maintenance of remission and prevention of relapse?
and vitamin D2 or vitamin D3 6000 IU per day for
Prevention of post-operative recurrence?
8 weeks, or 50 000 IU once a week for 8 weeks for adults
5. What is the optimal serum 25(OH)D level for its effect
to achieve serum 25(OH)D levels of more than 30 ng/
on inflammation in patients with IBD?
mL. The optimal therapeutic regimen in IBD patients
6. What is the optimal dose and modality for treatment of
was examined in a single clinical trial by Pappa et al. in
vitamin D deficiency in IBD patients?
which 71 patients with IBD aged 5–21 years with vitamin
7. Can vitamin D supplementation reduce risk of
colorectal cancer in IBD?
D deficiency were randomised to one of the following
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
vitamin D deficiency leads causally to increased disease
severity or is merely a consequence of severe disease. Fur-
Guarantor of the article: Ananthakrishnan.
thermore, it needs to be identified if there are high-risk
Author contributions: Mouli and Ananthakrishnan per-
groups of patients who may need to be screened for vita-
formed literature review. Mouli wrote the first draft of
min D deficiency and preemptively treated to prevent the
the manuscript. Ananthakrishnan provided supervision
onset of IBD. Further high-quality studies are needed to
and both authors approved the final version of the
evaluate if correction of vitamin D deficiency or if vitamin
D supplementation can prevent disease relapses, whetherit can be used to induce remission in active disease, and
whether it has a role in prevention of long-term dis-
Declaration of personal interests: Dr Ananthakrishnan
ease-related complications like colorectal cancer as has
has served on the scientific advisory board of Cubist
been identified in non-IBD patients. Continued and fertile
interactions between biochemists, nutritional epidemiolo-
Declaration of funding interests: Dr Ananthakrishnan is
gists, laboratory scientists and clinical researchers will help
supported in part by a grant from the National Insti-
address many of these unanswered questions, improve our
tutes of Health (K23 DK097142). This work is also sup-
understanding of the role of the complex panoply of
ported by the National Institutes of Health (NIH) (P30
functions of vitamin D, and its application into clinical
DK043351) to the Center for Study of Inflammatory
Bowel Diseases.
10. Cantorna MT, Zhu Y, Froicu M, Wittke
guideline. J Clin Endocrinol Metab
A. Vitamin D status, 1,25-
2011; 96: 1911–30.
1. Abraham C, Cho JH. Inflammatory
dihydroxyvitamin D3, and the immune
17. Levin AD, Wadhera V, Leach ST, et al.
bowel disease. N Engl J Med 2009; 361:
system. Am J Clin Nutr 2004; 80:
Vitamin D deficiency in children with
inflammatory bowel disease. Dig Dis Sci
2. Khor B, Gardet A, Xavier RJ. Genetics
11. Garg M, Lubel JS, Sparrow MP, Holt
2011; 56: 830–6.
and pathogenesis of inflammatory bowel
SG, Gibson PR. Review article: vitamin
18. Alkhouri RH, Hashmi H, Baker RD,
disease. Nature 2011; 474: 307–17.
D and inflammatory bowel disease –
Gelfond D, Baker SS. Vitamin and
3. Jostins L, Ripke S, Weersma RK, et al.
established concepts and future
mineral status in patients with
Host-microbe interactions have shaped
directions. Aliment Pharmacol Ther
inflammatory bowel disease. J Pediatr
the genetic architecture of inflammatory
2012; 36: 324–44.
Gastroenterol Nutr 2013; 56: 89–92.
bowel disease. Nature 2012; 491:
12. Jorgensen SP, Agnholt J, Glerup H,
19. Ulitsky A, Ananthakrishnan AN, Naik
et al. Clinical trial: vitamin D3
A, et al. Vitamin D deficiency in
4. Ananthakrishnan AN. Environmental
treatment in Crohn's disease – a
patients with inflammatory bowel
triggers for inflammatory bowel disease.
randomized double-blind placebo-
disease: association with disease activity
Curr Gastroenterol Rep 2013; 15: 302.
controlled study. Aliment Pharmacol
and quality of life. JPEN J Parenter
5. Holick MF. Vitamin D deficiency. N
Ther 2010; 32: 377–83.
Enteral Nutr 2011; 35: 308–16.
Engl J Med 2007; 357: 266–81.
13. Ananthakrishnan AN, Cagan A, Gainer
20. Leslie WD, Miller N, Rogala L,
6. Holick MF. Sunlight and vitamin D for
VS, et al. Normalization of plasma 25-
Bernstein CN. Vitamin D status and
bone health and prevention of
hydroxy vitamin D is associated with
bone density in recently diagnosed
autoimmune diseases, cancers, and
reduced risk of surgery in Crohn's
inflammatory bowel disease: the
cardiovascular disease. Am J Clin Nutr
disease. Inflamm Bowel Dis 2013; 19:
Manitoba IBD Cohort Study. Am J
2004; 80: 1678S–88S.
Gastroenterol 2008; 103: 1451–9.
7. Rosen CJ. Clinical practice. Vitamin D
14. Norman AW. From vitamin D to
21. Gilman J, Shanahan F, Cashman KD.
insufficiency. N Engl J Med 2011; 364:
hormone D: fundamentals of the
Determinants of vitamin D status in
vitamin D endocrine system essential
adult Crohn's disease patients, with
8. Ananthakrishnan AN, Khalili H,
for good health. Am J Clin Nutr 2008;
particular emphasis on supplemental
Higuchi LM, et al. Higher predicted
88: 491S–9S.
vitamin D use. Eur J Clin Nutr 2006;
vitamin D status is associated with
15. Bienaime F, Prie D, Friedlander G,
60: 889–96.
reduced risk of Crohn's disease.
Souberbielle JC. Vitamin D metabolism
22. McCarthy D, Duggan P, O'Brien M,
Gastroenterology 2012; 142: 482–9.
and activity in the parathyroid gland.
et al. Seasonality of vitamin D status
9. Cantorna MT, Mahon BD. Mounting
Mol Cell Endocrinol 2011; 347:
and bone turnover in patients with
evidence for vitamin D as an
Crohn's disease. Aliment Pharmacol
environmental factor affecting
16. Holick MF, Binkley NC, Bischoff-
Ther 2005; 21: 1073–83.
autoimmune disease prevalence. Exp
Ferrari HA, et al. Evaluation, treatment,
23. Vagianos K, Bector S, McConnell J,
Biol Med (Maywood) 2004; 229:
and prevention of vitamin D deficiency:
Bernstein CN. Nutrition assessment of
an Endocrine Society clinical practice
patients with inflammatory bowel
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Review: vitamin D and inflammatory bowel diseases
disease. JPEN J Parenter Enteral Nutr
36. Yasuda H, Shima N, Nakagawa N,
responses. J Immunol 2009; 182: 4289–
2007; 31: 311–9.
et al. Osteoclast differentiation factor is
24. Harries AD, Brown R, Heatley RV,
a ligand for osteoprotegerin/
49. Yuk JM, Shin DM, Lee HM, et al.
Williams LA, Woodhead S, Rhodes J.
osteoclastogenesis-inhibitory factor and
Vitamin D3 induces autophagy in
Vitamin D status in Crohn's disease:
is identical to TRANCE/RANKL. Proc
human monocytes/macrophages via
association with nutrition and disease
Natl Acad Sci U S A 1998; 95: 3597–
cathelicidin. Cell Host Microbe 2009; 6:
activity. Gut 1985; 26: 1197–203.
25. Tajika M, Matsuura A, Nakamura T,
37. Lips P. Vitamin D deficiency and
50. Wu S, Sun J. Vitamin D, vitamin D
et al. Risk factors for vitamin D
secondary hyperparathyroidism in the
receptor, and macroautophagy in
deficiency in patients with Crohn's
elderly: consequences for bone loss and
inflammation and infection. Discov Med
disease. J Gastroenterol 2004; 39: 527–33.
fractures and therapeutic implications.
2011; 11: 325–35.
26. Leichtmann GA, Bengoa JM, Bolt MJ,
Endocr Rev 2001; 22: 477–501.
51. Wang J, Lian H, Zhao Y, Kauss MA,
Sitrin MD. Intestinal absorption of
38. Ardizzone S, Bollani S, Bettica P,
Spindel S. Vitamin D3 induces
cholecalciferol and 25-
Bevilacqua M, Molteni P, Bianchi Porro
autophagy of human myeloid leukemia
hydroxycholecalciferol in patients with
G. Altered bone metabolism in
cells. J Biol Chem 2008; 283: 25596–
both Crohn's disease and intestinal
inflammatory bowel disease: there is a
resection. Am J Clin Nutr 1991; 54:
difference between Crohn's disease and
52. Sly LM, Lopez M, Nauseef WM, Reiner
ulcerative colitis. J Intern Med 2000;
NE. 1alpha,25-Dihydroxyvitamin D3-
27. Sentongo TA, Semaeo EJ, Stettler N,
247: 63–70.
induced monocyte antimycobacterial
Piccoli DA, Stallings VA, Zemel BS.
39. Bernstein CN, Leslie WD. Review
activity is regulated by
Vitamin D status in children, adolescents,
article: osteoporosis and inflammatory
phosphatidylinositol 3-kinase and
and young adults with Crohn disease. Am
bowel disease. Aliment Pharmacol Ther
mediated by the NADPH-dependent
J Clin Nutr 2002; 76: 1077–81.
2004; 19: 941–52.
phagocyte oxidase. J Biol Chem 2001;
28. Vogelsang H, Schofl R, Tillinger W,
40. Siffledeen JS, Fedorak RN, Siminoski K,
276: 35482–93.
Ferenci P, Gangl A. 25-hydroxyvitamin
et al. Bones and Crohn's: risk factors
53. Liu PT, Modlin RL. Human
D absorption in patients with Crohn's
associated with low bone mineral
macrophage host defense against
disease and with pancreatic
density in patients with Crohn's
Mycobacterium tuberculosis. Curr Opin
insufficiency. Wien Klin Wochenschr
disease. Inflamm Bowel Dis 2004; 10:
Immunol 2008; 20: 371–6.
1997; 109: 678–82.
54. Liu PT, Stenger S, Tang DH, Modlin RL.
29. Farraye FA, Nimitphong H, Stucchi A,
41. Reffitt DM, Meenan J, Sanderson JD,
Cutting edge: vitamin D-mediated
et al. Use of a novel vitamin D
Jugdaohsingh R, Powell JJ, Thompson
human antimicrobial activity against
bioavailability test demonstrates that
RP. Bone density improves with disease
Mycobacterium tuberculosis is dependent
vitamin D absorption is decreased in
remission in patients with inflammatory
on the induction of cathelicidin.
patients with quiescent Crohn's disease.
bowel disease. Eur J Gastroenterol
J Immunol 2007; 179: 2060–3.
Inflamm Bowel Dis 2011; 17: 2116–21.
Hepatol 2003; 15: 1267–73.
55. Arnedo-Pena A, Juan-Cerdan JV,
30. Wang TJ, Zhang F, Richards JB, et al.
42. Kong YY, Feige U, Sarosi I, et al.
Romeu-Garcia A, et al. Latent
Common genetic determinants of
Activated T cells regulate bone loss and
tuberculosis infection, tuberculin skin
vitamin D insufficiency: a genome-wide
joint destruction in adjuvant arthritis
test and vitamin D status in contacts of
association study. Lancet 2010; 376:
through osteoprotegerin ligand. Nature
tuberculosis patients: a cross-sectional
1999; 402: 304–9.
and case-control study. BMC Infect Dis
31. Kim S, Shevde NK, Pike JW. 1,25-
43. Redlich K, Hayer S, Ricci R, et al.
2011; 11: 349.
Dihydroxyvitamin D3 stimulates cyclic
Osteoclasts are essential for TNF-alpha-
56. Ganmaa D, Giovannucci E, Bloom BR,
vitamin D receptor/retinoid X receptor
mediated joint destruction. J Clin Invest
et al. Tuberculin skin test conversion,
DNA-binding, co-activator recruitment,
2002; 110: 1419–27.
and latent tuberculosis in Mongolian
and histone acetylation in intact
44. Jahnsen J, Falch JA, Mowinckel P,
school-age children: a randomized,
osteoblasts. J Bone Miner Res 2005; 20:
Aadland E. Vitamin D status,
parathyroid hormone and bone mineral
feasibility trial. Am J Clin Nutr 2012;
32. McDonnell DP, Pike JW, O'Malley BW.
density in patients with inflammatory
96: 391–6.
The vitamin D receptor: a primitive
bowel disease. Scand J Gastroenterol
57. Toss G, Symreng T. Delayed
steroid receptor related to thyroid
2002; 37: 192–9.
hypersensitivity response and vitamin D
hormone receptor. J Steroid Biochem
45. Zehnder D, Bland R, Williams MC,
deficiency. Int J Vitam Nutr Res 1983;
1988; 30: 41–6.
et al. Extrarenal expression of 25-
53: 27–31.
33. Cantorna MT, Mahon BD. D-hormone
hydroxyvitamin d(3)-1 alpha-
58. Zhang Y, Leung DY, Richers BN, et al.
and the immune system. J Rheumatol
hydroxylase. J Clin Endocrinol Metab
Vitamin D inhibits monocyte/
Suppl 2005; 76: 11–20.
2001; 86: 888–94.
macrophage proinflammatory cytokine
34. Christakos S. Recent advances in our
46. Liu PT, Stenger S, Li H, et al. Toll-like
production by targeting MAPK
understanding of 1,25-dihydroxyvitamin
receptor triggering of a vitamin D-
phosphatase-1. J Immunol 2012; 188:
D(3) regulation of intestinal calcium
mediated human antimicrobial
absorption. Arch Biochem Biophys 2011;
response. Science 2006; 311: 1770–3.
59. Brennan A, Katz DR, Nunn JD, et al.
523: 73–6.
47. Liu PT, Schenk M, Walker VP, et al.
Dendritic cells from human tissues
35. Takeda S, Yoshizawa T, Nagai Y, et al.
Convergence of IL-1beta and VDR
express receptors for the
Stimulation of osteoclast formation by
activation pathways in human TLR2/1-
immunoregulatory vitamin D3
1,25-dihydroxyvitamin D requires its
induced antimicrobial responses. PLoS
binding to vitamin D receptor (VDR)
ONE 2009; 4: e5810.
Immunology 1987; 61: 457–61.
in osteoblastic cells: studies using VDR
48. Adams JS, Ren S, Liu PT, et al.
60. Adorini L, Penna G, Giarratana N,
knockout mice. Endocrinology 1999;
Vitamin D-directed rheostatic
Uskokovic M. Tolerogenic dendritic
140: 1005–8.
regulation of monocyte antibacterial
cells induced by vitamin D receptor
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
V. P. Mouli and A. N. Ananthakrishnan
ligands enhance regulatory T cells
murine inflammatory bowel disease.
three regimens. J Clin Endocrinol Metab
inhibiting allograft rejection and
J Nutr 2000; 130: 2648–52.
2012; 97: 2134–42.
autoimmune diseases. J Cell Biochem
73. Liu N, Nguyen L, Chun RF, et al.
84. Driscoll RH Jr, Meredith SC, Sitrin M,
2003; 88: 227–33.
Altered endocrine and autocrine
Rosenberg IH. Vitamin D deficiency
61. Griffin MD, Lutz W, Phan VA,
metabolism of vitamin D in a mouse
and bone disease in patients with
Bachman LA, McKean DJ, Kumar R.
model of gastrointestinal inflammation.
Crohn's disease. Gastroenterology 1982;
Dendritic cell modulation by 1alpha,25
Endocrinology 2008; 149: 4799–808.
83: 1252–8.
dihydroxyvitamin D3 and its analogs: a
74. Zhu Y, Mahon BD, Froicu M, Cantorna
85. Lamb EJ, Wong T, Smith DJ, et al.
vitamin D receptor-dependent pathway
MT. Calcium and 1 alpha,25-
Metabolic bone disease is present at
that promotes a persistent state of
dihydroxyvitamin D3 target the TNF-
diagnosis in patients with inflammatory
immaturity in vitro and in vivo. Proc
alpha pathway to suppress experimental
bowel disease. Aliment Pharmacol Ther
Natl Acad Sci U S A 2001; 98: 6800–5.
inflammatory bowel disease. Eur J
2002; 16: 1895–902.
62. Provvedini DM, Tsoukas CD, Deftos LJ,
Immunol 2005; 35: 217–24.
86. Siffledeen JS, Siminoski K, Steinhart H,
Manolagas SC. 1,25-dihydroxyvitamin
75. Daniel C, Sartory NA, Zahn N, Radeke
Greenberg G, Fedorak RN. The
D3 receptors in human leukocytes.
HH, Stein JM. Immune modulatory
frequency of vitamin D deficiency in
Science 1983; 221: 1181–3.
treatment of trinitrobenzene sulfonic
adults with Crohn's disease. Can J
63. Lemire JM, Adams JS, Kermani-Arab V,
acid colitis with calcitriol is associated
Gastroenterol 2003; 17: 473–8.
Bakke AC, Sakai R, Jordan SC. 1,25-
with a change of a T helper (Th) 1/Th17
87. Pappa HM, Gordon CM, Saslowsky
Dihydroxyvitamin D3 suppresses human
to a Th2 and regulatory T cell profile. J
TM, et al. Vitamin D status in children
T helper/inducer lymphocyte activity in
Pharmacol Exp Ther 2008; 324: 23–33.
and young adults with inflammatory
vitro. J Immunol 1985; 134: 3032–5.
76. El-Matary W, Sikora S, Spady D. Bone
bowel disease. Pediatrics 2006; 118:
64. Chen S, Sims GP, Chen XX, Gu YY,
mineral density, vitamin D, and disease
Chen S, Lipsky PE. Modulatory effects
activity in children newly diagnosed
88. Kuwabara A, Tanaka K, Tsugawa N,
of 1,25-dihydroxyvitamin D3 on human
with inflammatory bowel disease. Dig
et al. High prevalence of vitamin K and
B cell differentiation. J Immunol 2007;
Dis Sci 2011; 56: 825–9.
D deficiency and decreased BMD in
179: 1634–47.
77. Narula N, Marshall JK. Management of
inflammatory bowel disease. Osteoporos
65. Khalili H, Huang ES, Ananthakrishnan
inflammatory bowel disease with
Int 2009; 20: 935–42.
AN, et al. Geographical variation and
vitamin D: beyond bone health. J
89. Joseph AJ, George B, Pulimood AB,
incidence of inflammatory bowel
Crohns Colitis 2012; 6: 397–404.
Seshadri MS, Chacko A. 25(OH) vitamin
disease among US women. Gut 2012;
78. Verlinden L, Leyssens C, Beullens I,
D level in Crohn's disease: association
61: 1686–92.
et al. The vitamin D analog TX527
with sun exposure & disease activity.
66. Nerich V, Jantchou P, Boutron-Ruault
ameliorates disease symptoms in a
Indian J Med Res 2009; 130: 133–7.
MC, et al. Low exposure to sunlight is a
chemically induced model of
90. Pappa HM, Langereis EJ, Grand RJ,
risk factor for Crohn's disease. Aliment
inflammatory bowel disease. J Steroid
Gordon CM. Prevalence and risk
Pharmacol Ther 2011; 33: 940–5.
Biochem Mol Biol 2013; 136: 107–11.
factors for hypovitaminosis D in young
67. Kong J, Zhang Z, Musch MW, et al.
79. Zator ZA, Cantu SM, Konijeti GG, et al.
patients with inflammatory bowel
Novel role of the vitamin D receptor in
Pre-treatment 25-hydroxy vitamin D
disease. J Pediatr Gastroenterol Nutr
maintaining the integrity of the
levels and durability of anti-tumor
2011; 53: 361–4.
intestinal mucosal barrier. Am J Physiol
necrosis factor a therapy in
91. Atia A, Murthy R, Bailey BA, et al.
Gastrointest Liver Physiol 2008; 294:
inflammatory bowel diseases. JPEN J
Vitamin D status in veterans with
Parenter Enteral Nutr 2013 [Epub ahead
inflammatory bowel disease:
68. Dresner-Pollak R, Ackerman Z, Eliakim
relationship to health care costs and
R, Karban A, Chowers Y, Fidder HH.
80. Miheller P, Muzes G, Hritz I, et al.
services. Mil Med 2011; 176: 711–4.
The BsmI vitamin D receptor gene
Comparison of the effects of 1,25
92. Suibhne TN, Cox G, Healy M,
polymorphism is associated with
dihydroxyvitamin D and 25
O'Morain C, O'Sullivan M. Vitamin D
ulcerative colitis in Jewish Ashkenazi
hydroxyvitamin D on bone pathology
deficiency in Crohn's disease:
patients. Genet Test 2004; 8: 417–20.
and disease activity in Crohn's disease
prevalence, risk factors and supplement
69. Naderi N, Farnood A, Habibi M, et al.
patients. Inflamm Bowel Dis 2009; 15:
use in an outpatient setting. J Crohns
Association of vitamin D receptor gene
Colitis 2012; 6: 182–8.
polymorphisms in Iranian patients with
81. Yang L, Weaver V, Smith JP, Bingaman
93. Fu YT, Chatur N, Cheong-Lee C, Salh
inflammatory bowel disease. J
S, Hartman TJ, Cantorna MT.
B. Hypovitaminosis D in adults with
Gastroenterol Hepatol 2008; 23: 1816–22.
Therapeutic effect of vitamin D
inflammatory bowel disease: potential
70. Simmons JD, Mullighan C, Welsh KI,
supplementation in a pilot study of
role of ethnicity. Dig Dis Sci 2012; 57:
Jewell DP. Vitamin D receptor gene
Crohn's patients. Clin Transl
polymorphism: association with
Gastroenterol 2013; 4: e33.
94. Laakso S, Valta H, Verkasalo M,
Crohn's disease susceptibility. Gut 2000;
82. Ross AC, Manson JE, Abrams SA, et al.
Toiviainen-Salo S, Viljakainen H,
47: 211–4.
The 2011 report on dietary reference
Makitie O. Impaired bone health in
71. Eloranta JJ, Wenger C, Mwinyi J, et al.
intakes for calcium and vitamin D from
inflammatory bowel disease: a case-
Association of a common vitamin D-
the Institute of Medicine: what
control study in 80 pediatric patients.
binding protein polymorphism with
clinicians need to know. J Clin
Calcif Tissue Int 2012; 91: 121–30.
inflammatory bowel disease. Pharma-
Endocrinol Metab 2011; 96: 53–8.
95. Hassan V, Hassan S, Seyed-Javad P,
cogenet Genomics 2011; 21: 559–64.
83. Pappa HM, Mitchell PD, Jiang H, et al.
et al. Association between Serum 25
72. Cantorna MT, Munsick C, Bemiss C,
Treatment of vitamin D insufficiency in
(OH) Vitamin D concentrations and
children and adolescents with
inflammatory bowel diseases (IBDs)
Dihydroxycholecalciferol prevents and
inflammatory bowel disease: a
activity. Med J Malaysia 2013; 68: 34–8.
ameliorates symptoms of experimental
randomized clinical trial comparing
Aliment Pharmacol Ther 2014; 39: 125-136
ª 2013 John Wiley & Sons Ltd
Source: http://www.observatoire-crohn-rch.fr/wp-content/uploads/2015/06/Vit-D-IBD-APT-2014.pdf
January 1, 2016At A Glance For Active Employees, Retirees, Vestees and Dependent Survivors, Enrollees covered under Preferred List Provisions, their enrolled Dependents, and for COBRA Enrollees and Young Adult Option Enrollees enrolled through Participating Agencies with Empire Plan benefits This guide briefly describes Empire Plan benefits. It is not a complete description and is subject to change. For a complete description of your benefits and your responsibilities, refer to your Empire Plan Certificate and all Empire Plan Reports and Certificate Amendments. For information regarding your NYSHIP eligibility or enrollment, contact your agency Health Benefits Administrator (HBA). If you have questions regarding specific benefits or claims, contact the appropriate Empire Plan administrator. (See page 23.)
A community-based factorial trial on Alzheimer's disease. Effects of expectancy, recruitment methods, co- morbidity and drug use. The Dementia Study in Northern Norway Fred Andersen, MD ‘Navigare necesse est. Vivere non est necesse' Pompeius 56 f. Kr Contents