Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Sm050000761p
The American Journal of Sports
Graft Fixation in Cruciate Ligament Reconstruction
Jeff Brand, Jr., Andreas Weiler, David N. M. Caborn, Charles H. Brown, Jr. and Darren L. Johnson
Am J Sports Med
The online version of this article can be found at:
can be found at:
The American Journal of Sports Medicine
Additional services and information for
0363-5465/100/2828-0761$02.00/0THE AMERICAN JOURNAL OF SPORTS MEDICINE, Vol. 28, No. 5 2000 American Orthopaedic Society for Sports Medicine
Graft Fixation in Cruciate Ligament
Reconstruction
Jeff Brand, Jr.,* MD, Andreas Weiler,† MD, David N. M. Caborn,* MD,
Charles H. Brown, Jr.,‡ MD, and Darren L. Johnson,*§ MD
From the *University of Kentucky School of Medicine, Lexington, Kentucky, †Sports
Traumatology & Arthroscopy Service, Humboldt-University, Berlin, Germany, and ‡Brigham
and Women's Hospital, Department of Orthopaedic Surgery, Boston, Massachusetts
s.Current rehabilitation protocols after knee ligament sur-gery stress immediate full range of motion, return of neu-
Cruciate ligament reconstruction has progressed dra-
romuscular function, proprioception, and early weight-
matically in the last 20 years. Anatomic placement of
bearing forces up the kinetic chain. In the early
ligament substitutes has fostered rehabilitation efforts
postoperative period, graft fixation is the weak link within
that stress immediate and full range of motion, imme-
the entire system. No commonly used graft fixation has
diate weightbearing, neuromuscular strength and co-
ultimate failure strength or stiffness comparable with the
ordination, and early return to athletic competition (3
native cruciate ligament (Table 1). Fixation methods must
months). This has placed extreme importance on se-cure graft fixation at the time of ligament reconstruc-
be rigid and stiff to allow current rehabilitation principles.
tion. Current ligament substitutes require a bony or soft
Current fixation techniques involve soft tissue and bone
tissue component to be fixed within a bone tunnel or on
within a bone tunnel or periosteal fixation away from joint
the periosteum at a distance from the normal ligament
attachment site. Fixation devices have progressed
Bone-patellar tendon-bone, quadrupled hamstring ten-
from metal to biodegradable and from far to near-
don, or quadriceps tendon-bone are the most commonly
normal native ligament attachment sites. Ideally, the
used ligamentous substitutes in cruciate ligament recon-
biomechanical properties of the entire graft construct
struction. Using these ligament substitutes with current
would approach those of the native ligament and facil-
fixation devices, we have been unable to reproduce the
itate biologic incorporation of the graft. Fixation should
normal transition zones of insertion of the ACL and PCL.
be done at the normal anatomic attachment site of the
Given that anatomic structure dictates function, the me-
native ligament (aperture fixation) and, over time, allow
chanical profile of the ligament substitute has not been
the biologic return of the histologic transition zone from
reproduced. Variables that we are able to measure in the
ligament to fibrocartilage, to calcified fibrocartilage, to
basic science laboratory at time zero of ligament recon-
bone. The purpose of this article is to review current
struction include data on ultimate failure load, yield point,
fixation devices and techniques in cruciate ligament
stiffness, displacement to failure, and mode of failure.
Correlation of these results with clinical outcome has notbeen reported.
Our purpose is to review all current information with
regard to ligament substitute fixation of bone and soft
The importance of secure graft fixation in ligament recon-
tissue grafts. It is important for the surgeon to be aware of
struction has changed dramatically in the last 20 year-
the difference in fixation techniques with the associatedbiologic consequences. Different graft substitutes may re-quire different fixation techniques that have direct bio-
§ Address correspondence and reprint requests to Darren L. Johnson, MD,
logic implications. Knowledge of these fixation techniques
Chairman of Orthopaedic Surgery, University of Kentucky School of Medicine,
will allow the clinician to make necessary intraoperative and
Kentucky Clinic, K-439, 740 Limestone, Lexington, KY 40536.
One author has commercial affiliation with a product named in this study.
postoperative decisions in cruciate ligament reconstruction.
Brand et al.
American Journal of Sports Medicine
There is evidence that less than 454 N is sufficient for
Ultimate Load to Failure and Stiffness of Current Graft
activities of daily living. In a clinical study, Shelbourne
Selections in Cruciate Ligament Surgery
and Gray79 reported use of a button for both the tibial and
Ultimate Strength
femoral fixation of a patellar tendon reconstruction, which
Graft Selection (ref.)
has a failure strength of 248 N.43 Excellent clinical and
objective knee stability was maintained with an acceler-
ated rehabilitation program in their series of patients.
Patellar tendon25
Quadrupled hamstring
tendon (semitendinosisand gracilis)35
Biomechanical Properties
Quadriceps tendon85
Stiffness is the slope of the linear region of the load-elongation curve and is usually reported in units such asnewtons per millimeter (N/mm). As a graft and its fixation
IDEAL GRAFT FIXATION
device are loaded with a tensile force, displacement in thegraft and fixation device occurs equal to an amount de-
scribed by its stiffness. Present graft fixation alternativesare less stiff than the native ACL and graft choices. This
Because there is only one means of graft fixation that
can be compared with a chain secured to posts by bungee
approaches the strength of the native ACL, the question
cords at either end of the chain. As force is applied to the
is, "How much strength is required of a cruciate ligament
chain, the bungee cords, not the chain, will displace under
reconstruction for activities of daily living and a progres-
tensile load. Mechanically, the majority of tendon fixation
sive rehabilitation program?"
constructs are less stiff than the interference screw
Noyes et al.69 have estimated the strength required for
against a bone plug, which has been considered the stan-
activities of daily living to be 454 N based on the failure
dard for fixation (see Tables 4, 7, 8, and 9). Thus, given
strength of the ACL. They state that, "It seems reasonable
that ultimate failure strength is comparable between the
to assume that under normal conditions biological tissues
two given fixation choices, tendon constructs may displace
are subjected to forces ranging from one-tenth to not more
or slip more before they fail, creating laxity in the graft
than one-fifth of their breaking loads." The same group
concludes "For the posterior cruciate ligament (PCL) these
Many tendon fixation devices are "indirect." They rely
force levels would be increased."
on linkage material to connect the tendon to the fixation
Morrison,64–66 a bioengineer, writing in the late 1960s
device. A biomechanical study compared strain that was
and early 1970s in a series of three articles relating force
induced by cyclic loading in a patellar tendon graft and a
plate and gait analysis data, made calculations and con-
quadrupled hamstring tendon graft and found that the
clusions regarding the forces in the ACL and PCL; theseare shown in Table 2. Markolf et al.58 used a cadavericmodel that ignored muscle forces and examined the forceson the ACL, a patellar tendon graft, and an overtensioned(45 N) patellar tendon graft. The patellar tendon graftexperienced higher forces than the native ACL (peakforce, 297 N) and overtensioning the graft increased theforces experienced by the graft (up to 497 N). In a similarstudy by Markolf et al.,59 the PCL forces were examined inthe intact PCL and a patellar tendon graft was used toreconstruct the PCL. The forces in the PCL study weremuch lower, generally less than 100 N. The higher forcesdeveloped in some grafts in hyperextension and hyperflex-ion, leading the authors to recommend avoiding thesemotions after reconstruction.
Estimations of Forces Present in the Cruciate Ligaments in
Activities of Daily Living64–66
Descending stairs
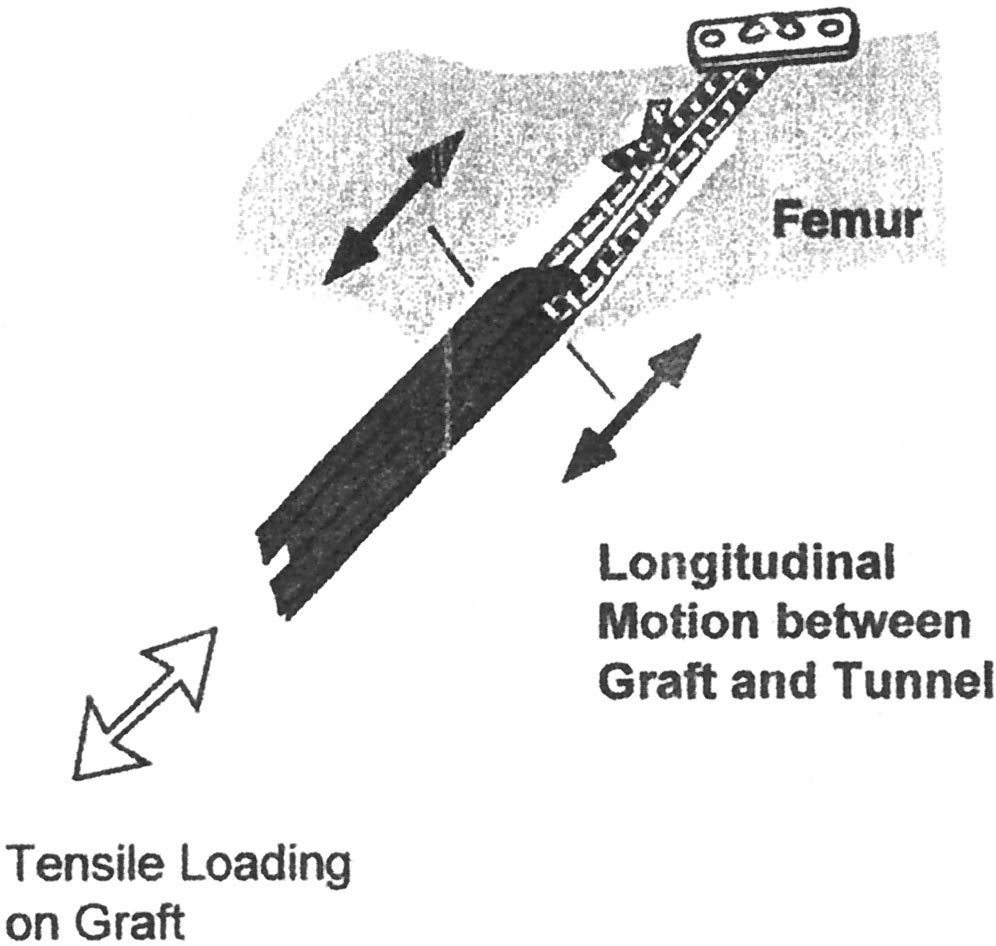
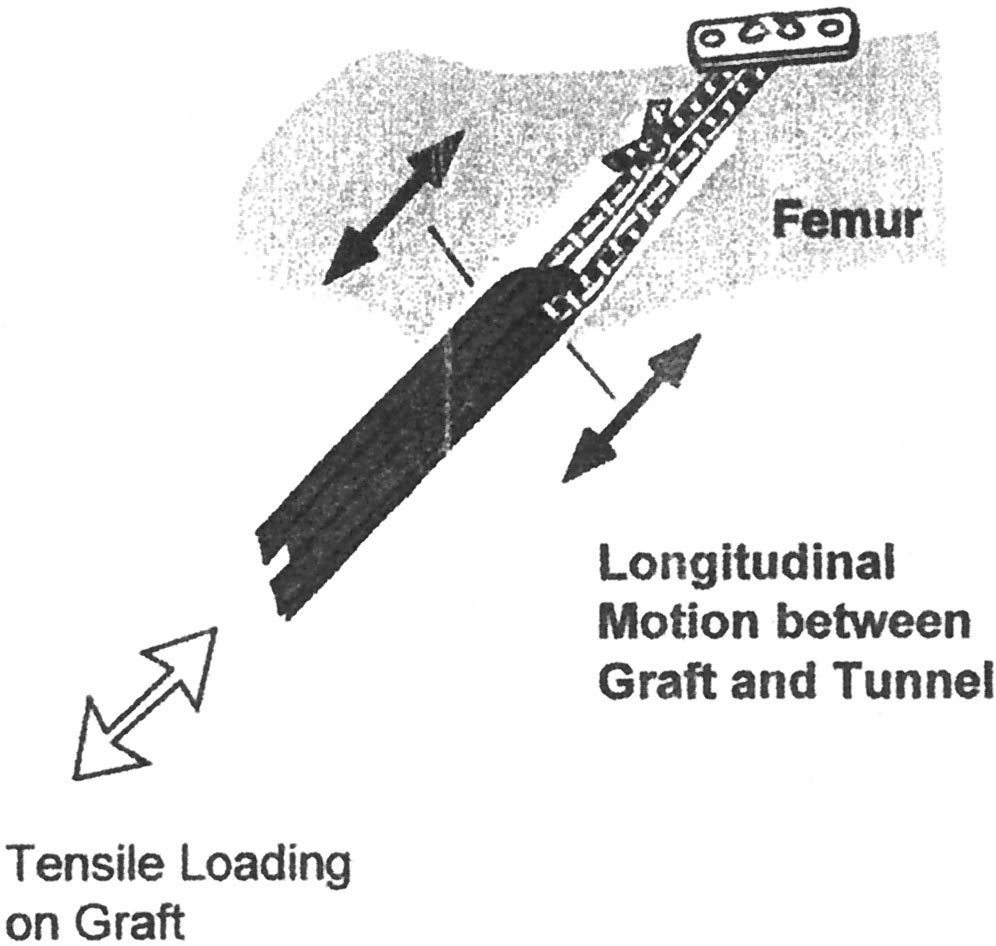
Figure 1. A schematic diagram demonstrating the bungee
effect or longitudinal graft-tunnel motion.
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
tape-tissue interface (5.4%) had notably more strain than
tendon graft incorporation has been shown to occur
the tape (2.9%) or the tissue (1.1%) alone.52 If strain or
sooner. A rabbit model with a free semitendinosus graft
laxity is in line with the linkage, it is referred to as the
intraarticularly placed through bone tunnels and fixed
bungee cord effect32 (Fig. 1). These shearing forces may be
with suture suggested that the graft healed in the tunnel
responsible for tunnel expansion, also known as the wind-
within 3 weeks.34 In a similar ACL reconstruction study
with a sheep model fixed with biodegradable interference
In the native cruciate ligament, the point of fixation is
screws directly against the free autologous Achilles ten-
at the joint surface. However, most tendon fixation con-
don graft, intraligamentous failure was demonstrated by 6
structs are placed at a distance from the joint surface with
weeks.92 Evidence of bone plug incorporation before soft
a staple, screw and suture, or soft tissue washer. When
tissue healing in a bone tunnel is not definite based on
interference fixation is placed closer to the joint surface,
animal studies. Weightbearing and rehabilitative exer-
there is increased knee stability at a variety of flexion
cises increase stress that the new, reconstructed ligament
angles and also improved graft isometry (Fig. 2) (Ref. 41;
will have to respond to and react. These activities occur at
C. Morgan, unpublished data, 1994).
the time when the weak link of the reconstruction is thefixation of the graft. In our laboratory experience, evenlow cyclic loads, up to 110 N, cause shear forces in the bone
Biologic Properties
tunnel on the graft.12 Strength and stiffness in the fixa-tion is the key to diminishing this graft-bone tunnel mo-
It has been stated that bone plug incorporation occurs
tion as healing progresses.
before tendon incorporation in a bone tunnel,76 but basicscience on this matter is not definite. In a study by Clancyet al.,23 bone plug-patellar tendon-bone plug in a bone
FEMORAL AND TIBIAL FIXATION
tunnel was histologically incorporated at 8 weeks aftersurgery in a rhesus monkey, when it was first histologi-
There are two key differences that need to be considered
cally examined. After 3 months, all biomechanical testing
between femoral and tibial fixation, that of bone density
resulted in interstitial failure of the reconstructed grafts,
and the angle at which force is applied to the graft attach-
with no bony avulsions occurring, thus implying bone plug
ment. The bone quality and geometry of the tibia is dif-
incorporation in the bone tunnel.
ferent from that of the femur.11 The Dual Photon Absorp-
In a dog extraarticular tendon model, the tendon graft
tometry (DEXA) of the tibial metaphysis has been
pulled out of the bone tunnel until 12 weeks postopera-
determined to be less than the femoral metaphysis in the
tively, indicating that the tendon was not healed in the
same knee of elderly cadavers11 and in young women.89
bone tunnel. The graft was an extraarticular, long digital
The line of force on the graft is directly in line with the
extensor tendon and was left attached distally under ten-
tibial tunnel. The line of force on the graft is obliquely
sion; it was not an intraarticular free graft.73 However,
orientated to the femoral tunnel in the weightbearingposition, which is extension. Based on radiographic stud-ies, the femoral tunnel does not become colinear with theligament graft until approximately 100° of knee flexion.57
Kohn and Rose46 have found a lower ultimate load of
tibial failure when using interference fixation for boneplug fixation.
Study methods of present biomechanical studies vary ex-tensively from institution to institution, making compar-ative statements of fixation methods and devices difficult(Table 3). Variables that we are able to measure in thebasic science laboratory at time zero of ligament recon-struction include data on ultimate failure load, yield point,stiffness, displacement to failure, and mode of failure.
Stiffness, an important descriptive variable that predictsthe displacement or slippage of a device before it fails, hasnot been reported in all biomechanical studies. Anothervariable, bone mineral density, with direct clinical appli-cations is varied throughout present studies. Bone min-eral density is correlated with the results of tendon inter-
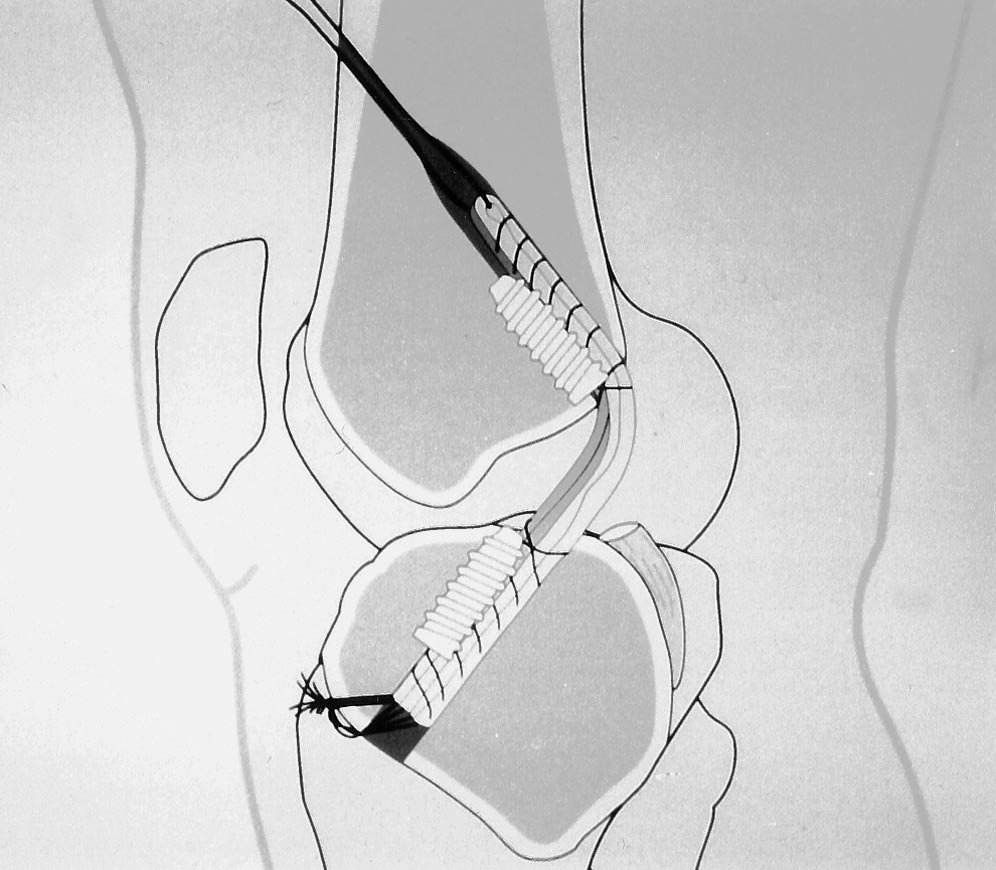
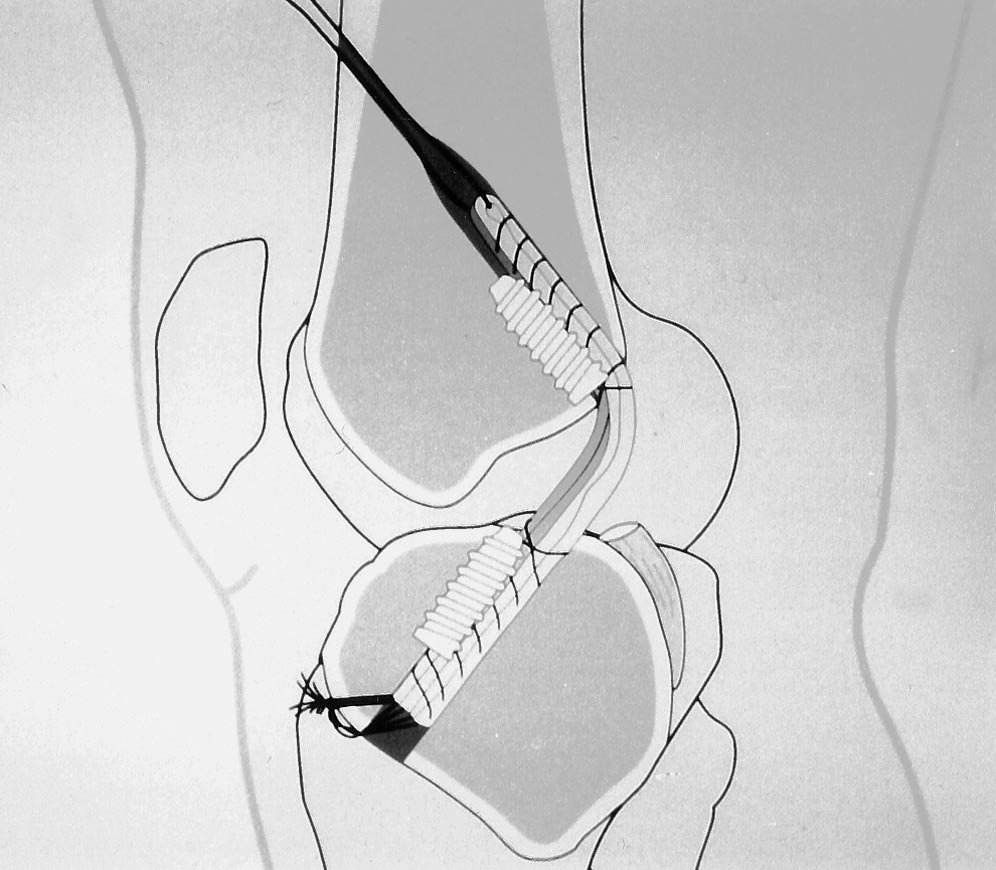
Figure 2. A schematic representation of a transtibial ACL
ference fixation and may be important in other forms of
reconstruction using a quadrupled hamstring tendon graft
fixation as well.11 The results of animal studies, which
and direct biodegradable interference screw fixation placed
have a higher and more consistent bone mineral density,
at joint surfaces.
have yielded higher failure values using interference fix-
Brand et al.
American Journal of Sports Medicine
Biomechanical Study Methods for Fixation Devices
Comparison of "Pull-out" Studies
using Human Tissue
Brown et al., older cadavers
Semifix, bone mulch,
Anterior drawer to
interference fixation,
semitendinosis and
endobutton, press-fit
gracilis tendonpatellar tendon
Brown et al.,14 older cadaver
Interference screws,
Femur only, in line
compared rear entry
Caborn et al.,19 older cadavers
Femur only, in line
interference screw
Caborn et al.,18 older cadavers
BioScrew, titanium
Femur only, in line
interference screw
Gerich et al.,33 cadavers (ages
Interference screws,
Tibia only, "axial to
Patellar tendon bone
Johnson and vanDyk,44
Interference screw
Femoral preparation
cadavers (ages 47–70)
only, in line with
biodegradable screw
Kohn and Rose,46 cadavers,
Interference screw,
Tibia preparation
median age, 30 (22–60)
influence of screw
Femoral preparation,
diameter, compared
Kurosaka et al.,48 cadavers,
Anterior drawer to
interference fixation,
Magen et al.,56 cadavers (ages
Tibia preparation, in
Quadrupled hamstring
line with the tunnel
Matthews et al.,62 cadavers
Interference screw,
Tibia preparation,
suture and post with
femoral preparation,
graft tensionedperpendicularly tobone preparation
Pena et al.,70 cadavers (ages
Interference screw,
Femoral preparation,
BioScrew and metal
Rowden et al.,74 young
Interference screw
Anterior drawer to
cadavers (mean age, 26)
Steiner et al.,87 cadavers
Suture and post, post
Anterior drawer to
interference screw
quadrupled hamstring
Weiler et al.,97 cadaver (mean
Button, screw and
Anterior drawer to
Hamstring, hamstring
washer, RCI screw,
ation than comparable human studies.56 The bone min-
BONE PLUG GRAFT FIXATION—TIBIAL FIXATION
eral density of elderly cadavers may be as little as halfthat of a young healthy person who sustains cruciate
ligament damage as a teenager. Because of the scarcity ofspecimens, the same specimen is often tested multiple
Although there are alternative means of fixation in graft
times. Techniques vary from the clinical situation to the
tunnel-length mismatch, this mismatch is considered the
laboratory. For instance, the interference screw is often
primary indication for staple fixation of a bone plug. An-
placed under direct visualization, minimizing the possibil-
other method of fixation for graft tunnel-length mismatch
ity of divergence, which certainly occurs in vivo.51 If a
include a longer femoral tunnel with a proportionately
device is tested in line with the tunnel, the worst-case
longer interference screw to create aperture fixation. Var-
scenario, the failure load may be less than if the device is
ious means of shortening the graft to match tunnel length
loaded at an angle to the tunnel that will increase the
have also been described. A set of doubled staples in a
shear forces. Because of viscoelastic properties of the
shallow trough (with an ultimate load at failure of 588 N)
graft-bone construct, the rate the graft is loaded will affect
compared favorably with interference fixation (506 to 758
the stiffness. Rehabilitation and ambulation stresses are
N) in failure, and the staples were significantly stiffer
examples of cyclic loading and are not accounted for with
(86.3 N/mm) than interference fixation (49.2 to 54.9
static testing at time zero fixation of the graft
N/mm) in a young (mean age, 44) human cadaveric model.
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
Unfortunately, the incidence of bone block breakage (27%)
fixation may be combined with other types of fixation such
was significantly greater than that of the interference
as a suture and post, EndoButton (Acufex, Inc., Mansfield,
screw fixation (1%).33
Massachusetts), or screw and washer.
Currently, a screw 9 mm in diameter and at least 20
Screws Used as a Post
mm in length is the standard used for fixation. The dif-ference between the outside diameter of the screw and the
Steiner et al.87 did a study that reported a screw used as
core diameter is the most important consideration.97 Kohn
a post, linked with suture, and combined with an inter-
and Rose46 showed that a 9-mm tibial interference screw
ference screw against a bone plug. They found that this
disengaged from the bone tunnel at significantly more
had a failure strength (674 N), which approximated that of
maximum tensile strength and linear load to failure com-
the intact ACL (560 N) (Table 4). The angle at which the
pared with a 7-mm screw (Table 4). Screw length beyond
screw is placed determines whether the graft is tensioned
20 mm in conjunction with a bone plug does not appear to
as the screw is tightened or whether the graft is relaxed as
be necessary.14,39
the screw is tightened. Although a low-profile screw with
The gap between the bone plug and bone tunnel and the
a flatter head is available from many of the orthopaedic
interaction with screw diameter influences the fixation
manufacturers, conventional screws are often removed
strength. Brown et al.15 suggested that interference
because of pain. The post and suture can serve as a backup
(screw outer diameter minus tunnel bone block gap) was
to tibial interference fixation that is compromised by poor
correlated with failure, but gap size alone is not associated
bone quality or bone plug fracture.
with failure. Similarly, a separate porcine biomechanicalstudy showed that a 1- or 2-mm gap with a 7-mm screw
Interference Fixation
yielded equal failure strength to a 3- or 4-mm gap with a
Whatever fixation strength is required for activities of
9-mm screw.17 Alternatively, when faced with a gap or
daily living and a progressive rehabilitation program ap-
bone of poor quality, a bone shim may improve the fixation
pears to be met by the strength and stiffness of interfer-
ence fixation, which, for this reason, has been described as
Despite the clinical success of interference fixation,
the standard of graft fixation.87 Interference fixation was
complications, usually preventable, have been reported.
first described by Lambert50 in a study using a 6.5-mm
Counter tension through the bone plug sutures can reduce
cancellous screw. In 1987, Kurosaka et al.48 demonstrated
graft advancement as the interference screw is placed.61
superior strength with a larger diameter screw (9 mm) for
Screw laceration of either the bone plug suture or of the
interference fixation. When poor bone stock exists—which
graft itself are clinical concerns. If the sutures that are
may be due to revision, tunnel widening, or graft tunnel-
attached to the bone plug are lacerated with the threads
length mismatch— or additional fixation strength is
from the screw, poor graft fixation cannot be salvaged
needed for large or noncompliant patients, interference
with a suture-and-post construct. Suture laceration can be
Tibial Fixation Options for Bone-Patellar Tendon-Bone Plug in a Bone Tunnela
Suture (#5) to button48
Anterior drawer to knee
Button failed, suture pulled
through the bone plug
Staple1 patella tendon48
Anterior drawer to knee
Graft slipped under the staple
Doubled staples on patella
Tibia only, "axial to
Graft slipped under staple, 27%
tendon in a trough33
bone block breakage
Suture and post87
Anterior drawer to knee
Bone-tendon rupture, bone plug
fracture, tibial post pull-out
6.5 mm AO interference screw48
Anterior drawer to knee
Grafts pulled out of the tunnel
9 mm interference screw48
Anterior drawer to knee
Grafts pulled out of the tunnel
Interference screw and suture
Anterior drawer to knee
Bone plug fractured, pull-out
around tibial screw and suturerupture
7 mm interference screw46
Tibia only, parallel to
Tendon tearing, slipping of the
9 mm interference screw46
Tibia only, parallel to
Tendon tearing, slipping of the
9 ⫻ 30 mm interference screw33
Tibia only, "axial to
Tendon tearing or bone plug
9 ⫻ 25 mm biodegradable
Tibia only, parallel to
Bone plug slipped, tendon tearing
a The standard deviations or ranges of variability are reported in parentheses following the mean.
Brand et al.
American Journal of Sports Medicine
avoided with the use of 20-gauge wire through the holes in
ing to their degradation. Group one consists of slow de-
the bone plug. Graft laceration may require another graft
grading and highly crystalline poly-(L-lactide) and poly-
option.61 Two cases of bone plug comminution have been
(L-co-D,L-lactide) stereocopolymers with a low D,L amount.
reported: one was salvaged by reversing the graft and
These materials are considered to have high mechanical
placing the fractured bone plug on the tibial side and
properties among the poly-alpha-hydroxy acids, but their
fixing it with a suture and post, the other had to be revised
degradation can last up to several years and is incomplete
to another graft choice.5 Pain in the area of the tibial
because of a possible accumulation of insoluble crystalline
screw that was caused by hardware has been reported by
implant remnants.6,22,27,71 Group two is represented by
3% of patients, and screw removal was very successful in
amorphous poly-(L-co-D,L-lactide) stereocopolymers with a
relieving this pain.49
high D,L amount and the purous poly-(D,L-lactide). Thesematerials degrade completely within 1 to 2 years, but their
Biodegradable Interference Screws
mechanical properties are lower compared with the poly-(L-lactide).84 The third group consists of fast-degrading
The terms "biodegradable" or "bioabsorbable" are used
copolymers such as poly-(D,L-lactide-co-glycolide) or polyg-
interchangeably to characterize materials that disinte-
lycolide-co-trimethylencarbonate, whose strength reten-
grate after implantation and are subsequently excreted.
tion lasts for only several weeks.
Materials that disintegrate in the body have been used by
For many years, biodegradable implants have been
orthopaedic surgeons over the past 3 decades and these
thought to offer advantages over metal analogs. Metal
materials allow for better available implants. In cruciate
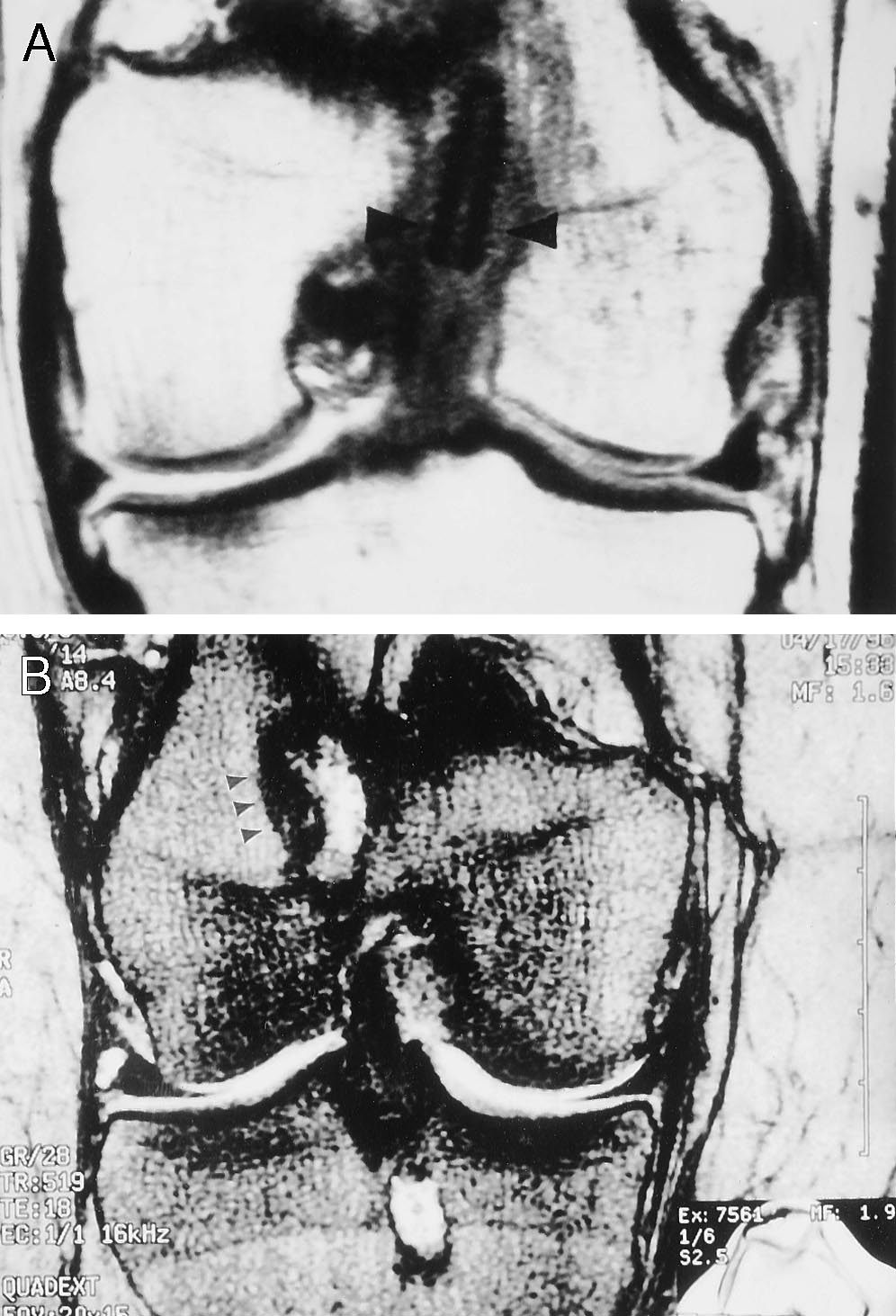
implants can distort magnetic resonance imaging (Fig. 3)
ligament surgery, several different biodegradable inter-ference screws consisting of different polymeric raw ma-
and release metal ions into the surrounding tissue.40, 80
terials are currently available (Table 5). A large number of
Further disadvantages include the need for a second sur-
studies have investigated their biomechanical and clinical
gical procedure for implant removal and a revision sur-
gery complicated by the presence of a metal implant. In
Biodegradable implants consist mainly of the poly-al-
cruciate ligament surgery, the major advantages of biode-
pha-hydroxy acids, polylactide and polyglycolide, includ-
gradable interference screws is an uncompromised revi-
ing their copolymers, poly-(D,L-lactide-co-glycolide) and
sion surgery. This is especially important because the
number of revisions has risen dramatically within the last
as poly-(L-lactide), poly-(L-co-D,L-lactide) and poly-(D,L-
few years.68,88 The difficulties encountered with retained
lactide) are also used (Table 5). These raw materials repre-
metal screws in revision surgery has been described.77 In
sent substantially different material characteristics, such
case of revision after using biodegradable interference
as degradation kinetics, mechanical properties, and bio-
screws, surgery may be performed like a primary proce-
compatibility. Generally, it is considered reasonable to
dure if the material has degraded and osseous replace-
divide these materials into three different groups accord-
ment has taken place with an appropriate amount of
Advantages and Disadvantages of Different Biodegradable Interference Screws
Implant (Manufacturer)
Raw material (Abbreviation)
Biologically Quiet Interference
Amorphous material, osseous
Low initial fixation strength, fast
Screw (Instrument Makar
glycolide) 85/15%
replacement within an
degradation,71 only one size
Inc., Okemos, MI)
appropriate time62
Bio-Interference Screw (Arthrex poly-(L-lactide) (PLLA)
High initial fixation strength,71
Semicrystalline PLLA with
Corp., Naples, FL)
different sizes available
recrystallization and possibleincomplete degradation
BioScrew (Linvatec Corp.,
poly-(L-lactide) (PLLA)
High initial fixation strength, high
Highly crystalline PLLA with
torsional strength,71 different
incomplete degradation62
Endo-Fix (Acufex Inc.,
High initial fixation strength71
Low torsional strength,
crystalline copolymer, fast
67.5/32.5% (PGA-co-
degradation with possible
adverse tissue response,20,30,71only one size available
Phantom Absorbable Screw
poly-(L-lactide) (PLLA)
High initial fixation strength
Highly crystalline PLLA with
(DePuy Orthopaedic
incomplete degradation
Technology Inc., Tracy, CA)
Phusiline Interference Screw
High initial fixation strength
Low torsional strength,
(Phusis mate´riaux
different sizes available71
semicrystalline polymer with
biore´sorbables, Le Versoud,
re-crystallization and
incomplete degradation71
Sysorb (Sulzer Orthopedics
High initial fixation strength, high
Possible viscoplastic deformation,
torsional strength, amorphous
only one size available
material, osseous replacementwithin an appropriate time62,71
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
incorporation of a bone-tendon-bone graft, and little isknown about the fixation properties of the biodegradablescrews within this period while the material is degrading.
Only a few in vivo studies have investigated changes infixation strength of biodegradable interference screwsover time. Walton and Cameron90 used polyglycolide-co-trimethylencarbonate screws (Endofix, Acufex Inc.) in asheep model and reported that the fixation strength ofthese screws remained comparable with that of metalscrews for 12 weeks. Therin et al. (unpublished data,1996) also investigated the in vivo biocompatibility anddegradation of a poly-(L-co-D,L-lactide) screw (Phusiline,Phusls mate´riaux biore´sorbables, St. Ismier, France) in asheep model and reported proper bone healing measuredby polychrome sequential labeling. Champion et al.21 in-vestigated the pushout loads of a poly-(L-lactide) interfer-ence screw (Phantom, DePuy Inc., Tracy, California) in acanine model over 24 weeks, and suggested that thesescrews withstand ACL forces during the healing stage ofreconstruction. The clinical use of biodegradable interfer-ence screws for bone-tendon-bone graft fixation was firstdescribed in the middle 1990s (Refs. 3, 44; Therin et al.,unpublished data, 1996). To date, several midterm studiescomparing metal and biodegradable interference screws inclinical studies have reported no significant difference inclinical outcome.3,31,60
The major disadvantage of biodegradable screws is
screw breakage or drive failure during insertion (Refs. 3,43, 82, 97; C. Morgan, unpublished data, 1994). A screw'sresistance to breakage may depend on several factors,including core diameter, drive diameter, and drive shape.
The drive designs of some biodegradable interference
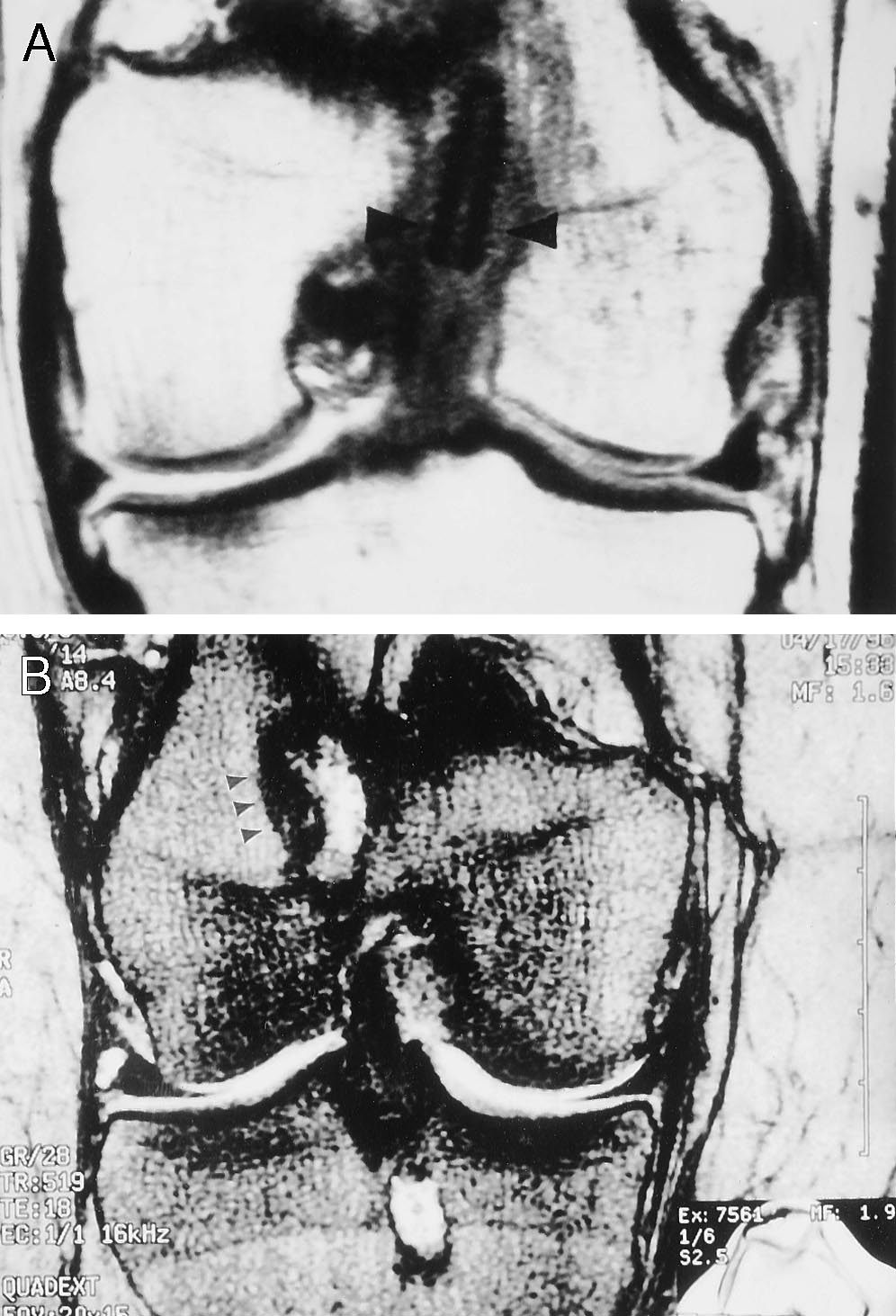
Figure 3. A, a coronal section MRI of the femoral tunnel at 2
screws are direct copies of their metallic counterparts.
months postoperatively of a biodegradable screw (arrows).
Others have specially designed drive systems that may
There is no artifact from the screw and it appears to be
provide a better force transmission to the screw core,
opposed to the quadrupled hamstring tendon graft. B, coro-
thereby increasing implant resistance to breakage (Table
nal section MRI of another patient with a biodegradable
5). A recent report demonstrated that implant design may
screw interference fixation at 1 year. The screws have nearly
be more important than the mechanical properties of the
completely degraded (arrows) leaving a bright signal, but
polymeric raw material to improve torsional strength.97
again the femoral graft is well opposed to the interference
To avoid screw breakage, care should be taken to insert
the screw convergent to the tunnel-bone block gap. Toreduce peak screw insertion torque, especially in thedense femoral bone, the manufacturer's recommendations
newly formed bone at the former implant site. In addition,
to use a notching device or a tap should be followed.
functional loads can be assumed earlier by the healing
There are still concerns about an appropriate biocom-
bone while the material is degrading.22 Another advan-
patibility of other biodegradable materials because of re-
tage in cruciate ligament surgery is a decreased potentialof graft laceration during screw insertion, which has been
ports on severe foreign-body reactions associated with the
described to occur when using metal screws.30,61
use of self-reinforced and highly crystalline polyglycolide
Several recent biomechanical studies compared the ini-
implants.8,20,36,91 Today, other materials such as polylac-
tial fixation strength of biodegradable and conventional
tide and its copolymers and stereocopolymers are consid-
titanium interference screws in human and animal cadav-
ered to have better biocompatibility,9,16,36,91 and clini-
eric models for bone-tendon-bone graft fixation. These
cally relevant foreign-body reactions have not yet been
studies showed that most biodegradable screws provide
described in the clinical reports on biodegradable interfer-
similar fixation strength and concluded that the use of
ence screws. However, further studies should take into
these screws may allow for an accelerated postoperative
consideration that foreign-body reactions may principally
rehabilitation program.1, 19, 70, 75, 97 While these investiga-
accompany the use of each biodegradable implant and, to
tions studied only the initial fixation strength, it is known
finally judge the appropriateness of such an implant, long-
that approximately 6 weeks are required for the bony
term studies are necessary.37
Brand et al.
American Journal of Sports Medicine
BONE PLUG GRAFT FIXATION—
Interference Fixation
Two studies with human tissue compared a metal 7-mm
diameter screw placed intraarticularly, as in endoscopicACL reconstruction, with an outside-in technique using a
The EndoButton is used primarily with bone plug fixation
9-mm screw and found similar strength and stiffness (Ta-
in femoral tunnel blow-out. Interference fixation is pref-
ble 7) (Ref. 87; Brown et al., unpublished data, 1996).
erable in routine femoral bone plug fixation. The En-
Although screw divergence from the bone plug is com-
doButton, a modification of the button, was designed to be
mon when postoperative radiographs are evaluated criti-
used in the endoscopic ACL reconstruction for femoral
cally,51 it is not considered a clinical concern. Dworsky et
fixation and now has been described for use in PCL recon-
al.28 described the endoscopically placed interference
struction as well.4,81 Doubling the linkage materials has
screw acting as a "wedge," effectively blocking the femoral
significantly increased their mechanical properties (Table
bone plug from being displaced into the joint. Further-
6) (C. H. Brown et al., unpublished data, 1996).
more, if the angle of screw divergence from the femoralbone plug is greater than 20°, there is a significant reduc-tion of the pullout strength in biomechanical testing.45
However, in the clinical situation, Fanelli et al.29 showed
The Mitek Anchor (Mitek, Westwood, Massachusetts) is a
that there was no increase in fixation failure with diver-
four-pronged device that is linked to a graft by suture or
gent interference screws placed endoscopically at angles
tape in a fashion similar to that of the EndoButton. When
greater than 20°.
comparing the Mitek device with the EndoButton in apatellar tendon-bone plug model, there was no significantdifference in failure or stiffness (Table 7) (Brown et al.,
SOFT TISSUE FIXATION—TIBIAL FIXATION
unpublished data, 1996). This device can be used similarlyto the EndoButton in cases of femoral fixation salvage for
femoral tunnel blow-out.
A single staple used with the semitendinosus tendon isneither strong nor stiff.48 The tendon graft looped over a
Press-Fit Femoral Bone Plug
second staple, now called the "belt-buckle" technique,markedly improved fixation in a porcine model.56 The
Malek et al.57 have reported press-fitting the femoral bone
failure load was 705 N with a stiffness of 174 N/mm (Table
plug in an effort to avoid the complications of interference
8). Staples can frequently cause pain at the site of implan-
screw fixation. Brown et al. (unpublished data, 1996) com-
tation and must be removed. Although the belt-buckle
pared the press-fit of the bone plug (ultimate load at
technique has been used successfully, fixation is perios-
failure, 350 N) with the patellar tendon bone plug with
teal and is at a distance from joint surfaces.
interference fixation (398 N), EndoButton (554 N), andMitek Anchor (511 N). No statistical difference was notedin failure or stiffness (Table 7). A clinical study with
Screws Used as a Post
press-fit fixation on the femoral side and interference
A screw can be used with a standard metal washer as a
screw fixation on the tibial side noted one case of femoral
post to tie suture around or it can be used with a soft
bone plug fracture.10 Two cases of revision to an interfer-
tissue washer against tendon. A screw with a soft tissue
ence screw were required because of "insufficient femoral
washer placed directly against a quadrupled tendon graft
is slightly stronger and stiffer than the screw used as apost with suture (821 ⫾ 219 N compared with 573 ⫾ 109N, respectively) (Table 8).87 A screw with a soft tissue
washer is the preferred method of tibial soft tissue fixa-
Linkage Material Propertiesa
tion, compared with a screw linked with suture, because of
its superior stiffness and avoidance of relatively elastic
Mersilene tape (Ethicon,
Inc., Sommerville, NJ)
Doubled Mersilene
Meadox (Meadox Medical
Inc., Oakland, NJ)
The washerplate, WasherLoc (Arthrotek, Biomet, Inc.,
Endotape (Smith and
Warsaw, Indiana), is a multiple-pronged washer and
Nephew Endoscopy,
screw used to fix the tibial end of the quadrupled ham-
Inc., Andover, MA)
string tendon graft. It is placed at the distal end of the
Three #5 Ethibond
tibial tunnel and can be recessed to diminish the promi-
sutures, (Ethicon, Inc.)
nence of the screw head. The ultimate failure load was 905
N (SD, 291 N) and the stiffness was 273 N (SD, 56 N),
From Brown et al., unpublished data, 1996. The standard
deviations are reported in parentheses following the mean.
which is similar to that of the native ACL (Table 8).56
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
Femoral Fixation Options for Bone-Patellar Tendon-Bone Plug in a Bone Tunnela
Anterior drawer to
Tibial bone block fracture or
suture breakage, tibial sidefixation failure
Mitek deviceb
Anterior drawer to
Patellar tendon failure, fracture
tibial bone block, sutures torethrough bone block
Anterior drawer to
Tibial bone plug pulled out,
fracture tibial bone block,patellar tendon failed
Interference screw from
Anterior drawer to
Pull-out around the screw
Endoscopic interference screw87
Anterior drawer to
Bone plug fractured, femoral
screw pull-out, bone tendonrupture
Interference screw outside-in14
Anterior drawer to
Bone block pull-out, bone block
Endoscopic interference screw14
Anterior drawer to
Bone block pull-out, bone block
Metal endoscopic interference
Femur only, parallel
Femoral fixation failure,
fracture of bone plug, tearingof graft
BioScrew endoscopic
Femur only, parallel
Femoral fixation failure,
interference screw19
fracture of bone plug, tearingof graft
Metal interference screw70
Femur only, parallel
Pullout and bone block fracture
BioScrew interference screw70
Femur only, parallel
Bone block pull-out
Metal interference screw44
Femur only, parallel
Failure between the cortical
and cancellous bone of thebone plug
Femur only, parallel
Failure between the cortical
and cancellous bone of thebone plug
a The standards deviations or ranges of variability are reported in parentheses following the mean.
b From Brown et al., unpublished data, 1996.
Tibial Fixation Options for a Soft Tissue Graft in a Bone Tunnela,b
Stapled semitendinosis48
Anterior drawer to knee
Tendon pulled out of staple
QHT with suture and post87
Anterior drawer to knee
Suture tendon stretches,
QHT with screw and a soft
Anterior drawer to knee
Tendon stretches or tibial
QHT with a washerplate56
Tibia only, parallel to
No failure mode given
QHT with the RCI titanium
Anterior drawer to knee
Tendons pulled out or
QHT with the RCI titanium
Tibia only, parallel to
No failure mode given
QHT with the RCI titanium
Anterior drawer to knee
Failed at the tibial socket
QHT with biodegradable
Tibia only, parallel to
Graft slipped around tibial
interference screw 1 mm
QHT with biodegradable
Tibia only, parallel to
Graft slipped around tibial
interference screw 1⁄2 mm
a QHT, quadrupled hamstring graft.
b The standard deviations are reported in parentheses following the mean.
c Brown et al., unpublished data, 1996.
Brand et al.
American Journal of Sports Medicine
Biomechanically, this is the only tibial soft tissue fixation
creased failure strength of the quadrupled hamstring ten-
that approximates the ACL in failure and stiffness.
don graft and an 89% increase in stiffness.35
Patients who have had ACL reconstruction with trans-
SOFT TISSUE FIXATION—FEMORAL
fixion devices have had outcomes similar to those reported
in the literature. Two patients had the pin repositionedafter migration.24 One of those patients and later another
Transfixion Fixation
patient had the pin removed because of iliotibial bandirritation. This device has since been modified to address
The Trans-Fix (Arthrex, Naples, Florida) and the Bone
the prominence of the pin head.24
Mulch Screw (Arthrotek) are examples of transfixion fix-
The cross-pin offers stiffness superior to the EndoBut-
ation. There was no significant difference in failure load or
ton linked with a continuous loop. In fact, stiffness of the
stiffness, Trans-Fix (523 N) versus the EndoButton with
cross-pin approaches that of the ACL. The device does
Endotape (520 N) (Smith & Nephew Endoscopy, Inc.). In
require a second counter incision to deploy the cross-pin.
paired knees, there was no difference in failure between
Fixation by this device is deeper in the tunnel, allowing for
the Bone Mulch screw (583 N) and EndoButton (628 N).
the graft to move in the tunnel, which has been associated
The Bone Mulch Screw was slightly stiffer; 24.4 N/mm
with tunnel expansion.
compared with 21.2 N/mm for the EndoButton (Brown etal., unpublished data, 1996). In cyclic biomechanical test-
ing, both the Trans-Fix (238 N/mm) and the Bone MulchScrew (257 N/mm) possessed stiffness superior to the En-
A biomechanical study in young human cadavers found
doButton linked with either the Endotape (183 N/mm) or
that a hamstring tendon construct fixed with an EndoBut-
the continuous loop (179 N/mm). The Trans-Fix (1042 N)
ton and a tibial post failed at 612 N ⫾ 73 N compared with
and the Bone Mulch Screw (978 N) were stronger to fail-
416 N ⫾ 66 N in the patellar tendon group with interfer-
ure than the Endobutton linked with Endotape (644 N),
ence fixation.74 The stiffness did not significantly vary
but the highest level of failure was reported with the
between groups. It was commented in the study that ei-
EndoButton linked with a continuous loop (1342 N)
ther construct was only 20% to 30% of the failure strength
(Brown et al., unpublished data, 1999) (Table 9). In addi-
of the native ACL (2195 N ⫾ 427 N) (Table 9).74 Direct
tion to a favorable failure strength and stiffness, transfix-
biomechanical comparison between EndoButton linked
ion devices may allow independent tensioning of the four
with a continuous loop and linked with Endotape revealed
strands of the quadrupled hamstring tendon. In a labora-
similar stiffness data, but a much higher failure with the
tory study, this resulted in a statistically significant in-
continuous loop, 1345 N versus 644 N for the Endotape
Femoral Fixation Options for a Soft Tissue Graft in a Bone Tunnela,b
QHT with Trans-Fixc
Anterior drawer to
Cross-pin toggled graft slipped
off, tibial fixation failure
QHT with Bone Mulchc
Anterior drawer to
Tibial fixation failure, implant
QHT with an EndoButton,
Anterior drawer to
mersilene tapec
QHT with EndoButton
Anterior drawer to
Tape broke, tibial fixation failure,
and Endotapec
tendon failure, implant pulled
QHT with EndoButton
Anterior drawer to
Implant pulled through bone,
and three #5 suturec
tibial fixation failure, suturefailure, tendon failure
QHT with EndoButton
Anterior drawer to
Tibial fixation failure, implant
pulled through the bone, tape
Semitendinosus fixed with
Anterior drawer to
the EndoButton and
QHT with Mitekc
Anterior drawer to
Implant pulled through bone
Femur only, parallel to
No stiffness reported
Failed by graft slipping
QHT with BioScrew18
Femur only, parallel to
No stiffness reported
Failed by graft slipping
QHT BioScrew, 0.5 mm
Femur only, parallel to
No stiffness reported
Failed by graft slipping
a QHT, quadrupled hamstring graft.
b The standards deviations are reported in parentheses following the mean.
c From Brown et al., unpublished data, 1996.
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
linked EndoButton (Brown et al., unpublished data,
ured from the time of operative fixation to later follow-up
in some patients.53 The authors are considering back-up
Biomechanically, the EndoButton linked with tape has
fixation to the interference screw for patients with sus-
motion of the graft in the tunnel of up to 3 mm under
pected lower bone mineral density or with poor screw
physiologic cyclic loads.38 This longitudinal motion or bun-
purchase. Despite low loads found with biomechanical
gee effect has been associated with tunnel expansion in
testing, a recent clinical report comparing transtibial
clinical trials.54,67 The natural history of tunnel expan-
hamstring and patellar tendon graft interference screw
sion is undetermined at present, but it is of obvious con-
fixation found no significant difference in outcome.26
cern to surgeons using hamstring tendon fixation with
Several factors exist that influence the initial fixation
linked devices. Extensive tunnel expansion complicates
strength of hamstring tendon grafts fixed with interfer-
revision surgery because of bone loss and may jeopardize
ence screws. These factors are especially important to
fixation of the graft. Despite this reservation, the Endo-
increasing fixation strength on the tibial site, which has
Button has been a popular and clinically successful form of
been considered to be the weak link of such a reconstruc-
femoral hamstring tendon fixation.
tion. Initially, Morgan (unpublished data, 1994) intro-duced a bone-hamstring tendon-bone composite graft for
an all-inside ACL reconstruction. In a biomechanicalstudy of this technique, Liu et al.55 found substantially
Brown et al. (unpublished data, 1996) compared the Mitek
lower loads and a high slippage for this bone-hamstring
Anchor directly with the EndoButton in paired elderly
tendon-bone composite graft compared with a bone-patel-
human specimens with a quadrupled hamstring tendon
lar tendon-bone graft in a porcine knees model. Shin et al.
graft. The EndoButton was significantly stronger (618 N
(unpublished data, 1996) introduced the harvest of a ham-
compared with 412 N, P ⫽ 0.03), but stiffness was compa-
string tendon graft with a distally attached tibial bone
rable (Table 9). The Mitek Anchor failed by pulling
plug, a method that has been used by Sta¨helin and
through the bone.
Weiler83 for the tibial fixation of a hamstring tendon graftin an all-inside technique. In another recent biomechani-
Interference Fixation
cal study it was demonstrated that the harvest of a semi-tendinosus tendon graft with a distally attached bone plug
The use of interference screw fixation of a multiple-looped
provides similar fixation strength when compared with
hamstring tendon graft has recently raised strong interest
the conventional bone-tendon-bone graft fixation, given
in soft tissue fixation in cruciate ligament reconstruc-
that both grafts were fixed with biodegradable interfer-
tion.26,32,78,82,83 The direct tendon-to-bone interference
screw fixation allows an anatomic fixation close to the
To enhance the direct tendon-to-bone interference fit
joint line, which has been demonstrated to increase knee
fixation without bone blocks, a precise match of tunnel
stability and graft isometry.41,42,63,96 Additionally, an an-
size to graft diameter is necessary; a recent biomechanical
atomic interference fit fixation may overcome biomechani-
study compared 1- and 0.5-mm tunnel sizing and found
cal disadvantages of conventional extraarticular ham-
that sizing the tunnels in increments of 0.5 mm increases
string tendon graft fixation techniques, such as suture
fixation strength significantly.86 In a separate biome-
stretch-out, graft tunnel motion, and the so-called wind-
chanical study investigating the effect of screw geometry
shield-wiper effect.37,38,54,95,96 It has been hypothesized
on hamstring tendon interference fit fixation, it was dem-
that these biomechanical disadvantages may contribute to
onstrated that by increasing both screw length and screw
the creation of high shearing forces at the tunnel wall,
diameter, fixation strength was significantly improved. In
which may also delay an osseous graft incorporation and
this study the influence of screw length (23 versus 28 mm)
lead to tunnel enlargement.54,67,95
was greater than that of thread diameter (screw diameter ⫽
Recent biomechanical studies compared biodegradable
graft size versus screw diameter ⫽ graft size ⫹ 1 mm).93
and blunt-threaded titanium interference screws (RCI,
To further ascertain the appropriateness of this new
Smith & Nephew Donjoy, Carlsbad, California) for ham-
technique for hamstring tendon graft fixation in cruciate
string tendon interference fit fixation and found that bio-
ligament surgery, it is essential to understand tendon-to-
degradable and titanium screws provide similar or supe-
bone healing progression with interference screw fixation.
rior fixation strength over conventional hamstring tendon
In a recent animal study there was evidence that the
fixation.18,86,94 In these reports, the mean failure load of
healing under interference screw compression follows dif-
a transtibial ACL reconstruction with hamstring tendons
ferent patterns than what has been described in animal
and interference screw fixation exhibited substantially
models using noncompressing extraarticular fixation tech-
lower loads than the estimated forces in the native ACL or
niques.7,34,73,92 In this animal model, Weiler et al.92
the graft during daily activities (Refs. 2, 58, 69, 96; Brown
found that the healing progresses only partially via the
et al., unpublished data, 1996). Therefore, it has been
development of a so-called fibrous interface (Fig. 4) This
advocated by some that the initial strength of transtibial
usually develops between the tendon graft and the bone
hamstring tendon interference fit fixation may not allow
surface. Their findings indicate that direct contact healing
for an accelerated postoperative rehabilitation (Refs. 56,
between the graft and the bone surface may exist if com-
96; Brown et al., unpublished data, 1996). A clinical study
pression fixation is used and may also overcome the de-
showed an increase in anterior tibial translation meas-
layed tendon-bone healing if extraarticular fixation is used.
Brand et al.
American Journal of Sports Medicine
Graft fixation remains the weak link in the early postop-erative period of ligament reconstruction. Technologicaladvancements in surgical techniques have allowed for animmediate return of neuromuscular function within theextremity. Fixation must not only withstand these earlyphysiologic forces but must also facilitate biologic incorpo-ration of the graft construct in its entirety. The specificanatomic location of the attachment site will have pro-found effects on fiber recruitment patterns within theligament substitute. Fixation of a bone plug in a bonetunnel with a metal or bioabsorbable interference screwappears to meet our current demands. Present soft tissuefixation within a bone tunnel or extratunnel may notpossess the same biomechanical or biologic properties as abone in a bone tunnel fixed with an interference screw.
Devices that are linked to the graft or placed nonanatomi-cally have been associated with motion through the graftconstruct and have spurred the search for direct fixationat the joint surface.
Controversy remains as to the suitability of soft tissue
fixation for progressive rehabilitation. Other fixation de-vices are used and tested—such as transfixion femoralfixation, hybrid fixation, and tibial washerplate fixa-tion—to more closely achieve the normal mechanical char-acteristics of the native ligament graft.
FUTURE DIRECTIONS
Ideally, the biomechanical properties of the entire graftconstruct would approach those of the native ligament andfacilitate biologic incorporation of the graft. Fixation
Figure 4. A, transversal cut of the tibial tunnel at 6 weeks
should be done at the normal anatomic attachment site of
after ACL reconstruction in a sheep model. An Achilles ten-
the native ligament (aperture fixation) and, over time,
don split graft was directly fixed with a biodegradable poly-
allow the biologic return of the histologic transition zone
(D,L-lactide) interference screw. The graft is directly in contact
from ligament to fibrocartilage to calcified fibrocartilage
with the surrounding bone tissue. A fibrous interface between
to bone. The transition from ligament to bone may occur
the graft and the bone is only partially developed, suggesting
without a fibrous interzone with compressive interference
a different mechanism of graft incorporation as compared
fixation. Manipulating the biologic environment with gene
with conventional extracortical fixation techniques. At the top
therapy or tissue engineering may speed graft incorpora-
of the figure is the indentation from the biodegradable screw
tion. Biodegradable screws can serve as a carrier for these
in the tendon tissue (Masson Goldner's trichrome stain). B,
substances or other growth factors to aid in graft incorpo-
fluorescence microscopy of a specimen at 9 weeks. There is
ration in the bone tunnel and fill the bone defect that may
an intensive fluorochrome activity at the interface between
be left by biodegradable screw absorption.
the graft and the bone tissue, indicating an early closure of
Diminishing individual fiber movement within the ten-
the fibrous interface. The green stain (calcein green) was
don graft and the elimination of linkage materials will
administered at 1 week, the yellow stain (tetracycline) was
improve future soft tissue fixation. Combination of fixa-
administered at 5 weeks.
tion devices, for example, use of a screw and washer and abiodegradable interference screw directly against a ten-don graft, or "hybrid fixation," may be useful in the inter-
When using biodegradable interference screw fixation
mediate future. Biodegradable bone cement that allows
for a soft tissue graft, there are concerns about a possible
for immediate fixation of the graft and eventual replace-
compromise of the graft incorporation when the screw
ment with normal osseous tissue may be developed. This
degrades. In the model of Weiler et al.,92 an intermediate
biodegradable bone cement may need to be combined with
degrading poly-(D,L-lactide) interference screw was used;
current graft fixation choices until it cures and achieves
it disintegrated macroscopically at 24 weeks. At this time,
maximum strength. Fixation that allows immediate and
no graft pull-out from the tunnel was observed. This indi-
secure fixation will aid rehabilitation, hasten return of
cates that screw degradation may not compromise graft
muscle tone and force, and benefit patient outlook.
incorporation after all.
Critical evaluation of patient satisfaction through out-
Vol. 28, No. 5, 2000
Graft Fixation in Cruciate Ligament Reconstruction
come-based research received recent emphasis at the 66th
17. Butler JC, Branch TP, Hutton WC: Optimal graft fixation. The effect of gap
size and screw size on bone plug fixation in ACL reconstruction. Arthros-
annual meeting of the Academy of Orthopaedic Surgeons
copy 10: 524 –529, 1994
(D. W. Jackson, unpublished data, 1999). The relationship
18. Caborn DNM, Coen M, Neef R, et al: Quadrupled semitendinosus-gracilis
between less stiff and less strong graft fixation that is
autograft fixation in the femoral tunnel. A comparison between a metal anda bioabsorbable interference screw. Arthroscopy 14: 241–245, 1998
currently available, the interplay with rehabilitative ef-
19. Caborn DNM, Urban WP Jr, Johnson DL, et al: Biomechanical compari-
forts, and laxity of the reconstructed knee has not been
son between BioScrew and titanium alloy interference screws for bone-
established. At present, there is not a strong clinical as-
patellar tendon-bone graft fixation in anterior cruciate ligament reconstruc-tion. Arthroscopy 13: 229 –232, 1997
sociation between fixation that performs well in labora-
20. Casteleyn PP, Handelberg F, Haentjens P: Biodegradable rods versus
tory testing and objective knee stability. If this association
Kirschner wire fixation of wrist fractures. A randomised trial. J Bone Joint
is proven, the clinical association of laxity to clinical out-
Surg 74B: 858 – 861, 1992
21. Champion AR, Cutshall TA, Van Sickle DC: In vitro and vivo evaluation of
come and patient satisfaction can be investigated. Pres-
a bioresorbable interference screw. Trans Orthop Res Soc 20: 638, 1995
ently, there are few clinical studies directed to these is-
22. Claes LE: Mechanical characterization of biodegradable implants. Clin
sues. Comparative studies of different modes of graft
Mater 10: 41– 46, 1992
23. Clancy WG Jr, Narechania RG, Rosenberg TD, et al: Anterior and pos-
fixation will be important in this effort. Longitudinal stud-
terior cruciate ligament reconstruction in rhesus monkeys. A histological
ies, although difficult and fraught with methods problems,
microangiographic and biomechanical analysis. J Bone Joint Surg 63A:
will establish the relationship between patient satisfac-
1270 –1284, 1981
24. Clark R, Olsen RE, Larson BJ, et al: Cross-pin femoral fixation: A new
tion, residual laxity, and degenerative arthrosis.
technique for hamstring anterior cruciate ligament reconstruction of theknee. Arthroscopy 14: 258 –267, 1998
25. Cooper DE, Deng XH, Burstein AL, et al: The strength of the central third
patellar tendon graft: A biomechanical study. Am J Sports Med 21: 818 –824, 1993
Thank you to Paula Hurley, MS Ed, and Bruce Pohlig for
26. Corry IS, Webb JM, Clingeleffer AJ, et al: Arthroscopic reconstruction of
the anterior cruciate ligament—A comparison of patellar tendon autograft
editorial assistance. A large number of researchers have
and four-strand hamstring tendon autograft. Am J Sports Med 27: 444 –
contributed to the study of graft fixation who are not
recognized in this article because of space constraints. We
27. Daniels AU, Chang MK, Andriano KP: Mechanical properties of biode-
gradable polymers and composites proposed for internal fixation of bone.
apologize for these omissions.
J Appl Biomater 1: 57–78, 1990
28. Dworsky BD, Jewell BF, Bach BR Jr: Interference screw divergence in
endoscopic anterior cruciate ligament reconstruction. Arthroscopy 12:
29. Fanelli GC, Desai BM, Cummings PD, et al: Divergent alignment of the
1. Abate JA, Fadale PD, Hulstyn MJ, et al: Initial fixation strength of polylactic
femoral interference screw in single incision endoscopic reconstruction of
acid interference screws in anterior cruciate ligament reconstruction. Ar-
the anterior cruciate ligament. Contemp Orthop 28(1): 21–25, 1994
throscopy 14: 278 –284, 1998
30. Fellinger M, Passler J, Wilburger R, et al: Komplikationen und mogliche
2. Aune AK, Ekeland A, Cawley PW: Interference screw fixation of hamstring
Fehlerquellen bei der Anwendung von interferenzschrauben in der arthro-
vs patellar tendon grafts for anterior cruciate ligament reconstruction.
skopischen Kreuzbandchirurgie. Arthroskopie: 33–38, 1993
Knee Surg Sports Traumatol Arthrosc 6: 99 –102, 1998
31. Frank A: Arthroscopic ACL reconstruction with patellar tendon. Absorb-
3. Barber FA, Elrod BF, McGuire DA, et al: Preliminary results of an absorb-
able interference screw versus metal screws. Proc Europ Soc Sports
able interference screw. Arthroscopy 11: 537–548, 1995
Traumatol Knee Surg Arthrosc, 8th Congress, Nice, France, 1998
4. Barrett GR, Papendick L, Miller C: EndoButton button endoscopic fixation
32. Fu FH, Bennett CH, Ma B, et al: Current trends in anterior cruciate
technique in anterior cruciate ligament reconstruction [Technical Note].
ligament reconstruction. Part II: Operative procedures and clinical corre-
Arthroscopy 11: 340 –343, 1995
lations. Am J Sports Med 28: 124 –130, 2000
5. Berg EE: Autograft bone-patella tendon-bone plug comminution with loss
33. Gerich TG, Cassim A, Lattermann C, et al: Pullout strength of tibial graft
of ligament fixation and stability [abstract]. Arthroscopy 12: 232–235, 1996
fixation in anterior cruciate ligament replacement with a patellar tendon
6. Bergsma JE, de Bruijn WC, Rozema FK, et al: Late degradation tissue
graft: Interference screw versus staple fixation in human knees. Knee
response to poly(L-lactide) bone plates and screws. Biomaterials 16:
Surg Sports Traumatol Arthrosc 5: 84 – 89, 1997
34. Grana WA, Egle DM, Mahnken R, et al: An analysis of autograft fixation
7. Blickenstaff KR, Grana WA, Egle D: Analysis of a semitendinosus au-
after anterior cruciate ligament reconstruction in a rabbit model.
tograft in a rabbit model. Am J Sports Med 25: 554 –559, 1997
Am J Sports Med 22: 344 –351, 1994
8. Bo¨stman OM: Intense granulomatous inflammatory lesions associated
35. Hamner DL, Brown CH Jr, Steiner ME, et al: Hamstring tendon grafts for
with absorbable internal fixation devices made of polyglycolide in anklefractures. Clin Orthop 278: 193–199, 1992
reconstruction of the anterior cruciate ligament: Biomechanical evaluation
9. Bo¨stman OM, Pihlajama¨ki HK, Partio EK, et al: Clinical biocompatibility
of the use of multiple strands and tensioning techniques. J Bone Joint
and degradation of polyevolactide screws in the ankle. Clin Orthop 320:
Surg 81A: 549 –557, 1999
36. Hoffmann R, Krettek C, Hetkamper A, et al: Osteosynthesis of distal
10. Boszotta H: Arthroscopic anterior cruciate ligament reconstruction using a
radius fractures with biodegradable fracture rods. Results of two years
patellar tendon graft in press-fit technique: Surgical technique and follow-
follow-up [in German]. Unfallchirurg 95: 99 –105, 1992
up. Arthroscopy 13: 332–339, 1997
37. Hoffmann R, Weiler A, Helling HJ, et al: Local foreign-body reactions to
11. Brand JC, Caborn P, Steenlage E, et al: Interference screw fixation
biodegradable implants. A classification [in German]. Unfallchirurg 100:
strength of a quadrupled hamstring tendon is directly correlated to bone
658 – 666, 1997
mineral density measured by dual photon absorptometry (DEXA). Arthros-
38. Hoher J, Livesay GA, Ma CB, et al: Hamstring graft motion in the femoral
copy 15: 58, 1999
bone tunnel when using titanium button/polyester tape fixation. Knee Surg
12. Brand JC, Danaceau S, Hamilton D, et al: Comparison of interference
Sports Traumatol Arthrosc 7: 215–219, 1999
fixation of tendon and bone plug for the quadriceps tendon in cruciate
39. Hulstyn M, Fadale PD, Abate J, et al: Biomechanical evaluation of inter-
ligament reconstruction. Arthroscopy 15: 58, 1999
ference screw fixation in a bovine patellar bone-tendon-bone autograft
14. Brown CH Jr, Hecker AT, Hipp JA, et al: The biomechanics of interference
complex for anterior cruciate ligament reconstruction. Arthroscopy 9: 417–
screw fixation of patellar tendon anterior cruciate ligament grafts.
Am J Sports Med 21: 880 – 886, 1993
40. Imhoff A, Burkart A, Roscher E: Foreign-body reaction to the bioabsorb-
15. Brown G, Pen˜a F, Grøntvedt T, et al: Fixation strength of interference
able suretac device. Arthroscopy 16: 91–95, 2000
screw fixation in bovine, young human, and elderly human cadaver knees:
41. Ishibashi Y, Rudy TW, Livesay GA, et al: The effect of the anterior cruciate
Influence of insertion torque, tunnel-bone block gap, and interference.
ligament graft fixation site at the knee on knee stability: Evaluation using
Knee Surg Sports Traumatol Arthrosc 3: 238 –244, 1996
a robotic testing system. Arthroscopy 13: 177–182, 1997
16. Bucholz RW, Henry S, Henley MB: Fixation with bioabsorbable screws for
42. Johnson DH, Houle JB, Almazan A: Comparison of intraoperative AP
the treatment of fractures of the ankle. J Bone Joint Surg 76A: 319 –324,
translation of two different modes of fixation of the grafts used in ACL
reconstruction [abstract]. Arthroscopy 14: 425, 1998
Brand et al.
American Journal of Sports Medicine
43. Johnson DP: Operative complications from the use of biodegradable
72. Race A, Amis AA: The mechanical properties of the two bundles of the
Kurosawa screws. J Bone Joint Surg 80B (Suppl 1): 103, 1998
human posterior cruciate ligaments. J Biomech 27: 13–24, 1994
44. Johnson LL, vanDyk GE: Metal and biodegradable interference screws:
73. Rodeo SA, Arnoczky SP, Torzilli PA, et al: Tendon-healing in a bone
Comparison of failure strength. Arthroscopy 12: 452– 456, 1996
tunnel. A biomechanical and histological study in the dog. J Bone Joint
45. Jomha NM, Raso VJ, Leung P: Effect of varying angles on the pullout
Surg 75A: 1795–1803, 1993
strength of interference screw fixation. Arthroscopy 9: 580 –583, 1993
74. Rowden NJ, Sher D, Rogers GJ, et al: Anterior cruciate ligament graft
46. Kohn D, Rose C: Primary stability of interference screw fixation: Influence
fixation: Initial comparison of patellar tendon and semitendinosus au-
of screw diameter and insertion torque. Am J Sports Med 22: 334 –338,
tografts in young fresh cadavers. Am J Sports Med 25: 472– 478, 1997
75. Rupp S, Krauss PW, Fritsch EW: Fixation strength of a biodegradable
47. Kousa P, Ja¨rvinen TLN, Pohjonen T, et al: Fixation strength of a biode-
interference screw and a press-fit technique in anterior cruciate ligament
gradable screw in anterior cruciate ligament reconstruction. J Bone Joint
reconstruction with a BPTB graft. Arthroscopy 13: 61– 65, 1997
Surg 77B: 901–905, 1995
76. Safran MR: Graft selection in knee surgery [current concepts]. Am J Knee
48. Kurosaka M, Yoshiya S, Andrish JT: A biomechanical comparison of
Surg 8: 168 –180, 1995
different surgical techniques of graft fixation anterior cruciate ligament
77. Safran MR, Harner CD: Technical considerations of revision anterior
reconstruction. Am J Sports Med 15: 225–229, 1987
cruciate surgery. Clin Orthop 325: 50 – 65, 1996
49. Kurzweil PR, Frogameni AD, Jackson DW: Tibial interference screw re-
78. Scranton PE Jr, Pinczewski L, Auld MK, et al: Outpatient endoscopic
moval following anterior cruciate ligament reconstruction. Arthroscopy 11:
quadruple hamstring anterior cruciate ligament reconstruction. Oper Tech
Orthop 6: 177–180, 1996
50. Lambert KL: Vascularized patellar tendon graft with rigid internal fixation
79. Shelbourne KD, Gray T: Anterior cruciate ligament reconstruction with
for anterior cruciate ligament insufficiency. Clin Orthop 172: 85– 89, 1983
autogenous patellar tendon graft followed by accelerated rehabilitation. A
51. Lemos MJ, Albert J, Simon T, et al: Radiographic analysis of femoral
two- to nine-year followup. Am J Sports Med 25: 786 –795, 1997
interference screw placement during ACL reconstruction: Endoscopic ver-
80. Shellock FG, Mink JH, Curtin S, et al: MR imaging and metallic implants
sus open technique. Arthroscopy 9: 154 –158, 1993
for anterior cruciate ligament reconstruction: Assessment of ferromag-
52. Levine RE, Simonian PT, Wright TM, et al: Cyclic creep response of
netism and artifact. J Magn Reson Imaging 2: 225–228, 1992
hamstring and patellar tendon ACL grafts. Arthroscopy 14: 436, 1998
53. Liew A, Johnson D: Bioabsorbable interference screw fixation of ham-
81. Shino K, Nakagawa S, Nakamura N, et al: Arthroscopic posterior cruciate
string graft in ACL reconstruction. Arthroscopy 15: 547–548, 1999
ligament reconstruction using hamstring tendons: One-incision technique
54. L'Insalata JC, Klatt BF, Fu FH, et al: Tunnel expansion following anterior
with EndoButton [technical note]. Arthroscopy 12: 638 – 642, 1996
cruciate ligament reconstruction: A comparison of hamstring and patellar
82. Stahelin AC, Feinstein R, Friederich NF: Clinical experience using bioab-
tendon autografts. Knee Surg Sports Traumatol Arthrosc 5: 234 –238,
sorbable interference screw for ACL reconstruction. Orthop Trans 19:
55. Liu SH, Kabo JM, Osti L: Biomechanics of two types of bone-tendon-bone
83. Sta¨helin AC, Weiler A: All-inside anterior cruciate ligament reconstruction
graft for ACL reconstruction. J Bone Joint Surg 77B: 232–235, 1995
using semitendinosus tendon and soft threaded biodegradable interfer-
56. Magen HE, Howell SM, Hull ML: Structural properties of six tibial fixation
ence screw fixation [technical note]. Arthroscopy 13: 773–779, 1997
methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med
84. Sta¨helin AC, Weiler A, Ru¨fenacht H, et al: Clinical degradation and bio-
27: 35– 43, 1999
compatibility of different bioabsorbable interference screws: A report of six
57. Malek MM, DeLuca JV, Verch DL, et al: Arthroscopically assisted ACL
cases. Arthroscopy 13: 238 –244, 1997
reconstruction using central third patellar tendon autograft with press fit
85. Sta¨ubli HU, Schatzmann L, Brunner P, et al: Quadriceps tendon and
femoral fixation. Instr Course Lect 45: 287–295, 1996
patellar ligament: Cryosectional anatomy and structural properties in
58. Markolf KL, Burchfield DM, Shapiro MM, et al: Biomechanical conse-
young adults. Knee Surg Sports Traumatol Arthrosc 4: 100 –110, 1996
quences of replacement of the anterior cruciate ligament with a patellar
86. Steenlage E, Brand JC, Caborn D, et al: Interference screw fixation of a
ligament allograft. Part II: Forces in the graft compared with forces in the
quadrupled hamstring graft is improved with precise match of tunnel to
intact ligament. J Bone Joint Surg 78A: 1728 –1734, 1996
graft diameter. Arthroscopy 15: 59, 1999
59. Markolf KL, Slauterbeck JR, Armstrong KL, et al: A biomechanical study of
87. Steiner ME, Hecker AT, Brown CH Jr, et al: Anterior cruciate ligament
replacement of the posterior cruciate ligament with a graft. Part II: Forces
graft fixation: Comparison of hamstring and patellar tendon grafts.
in the graft compared with forces in the intact ligament. J Bone Joint Surg
Am J Sports Med 22: 240 –247, 1994
79A: 381–386, 1997
88. Uribe JW, Hechtman KS, Zvijac JE, et al: Revision anterior cruciate
60. Marti C, Imhoff AB, Bahrs C, et al: Metallic versus bioabsorbable interfer-
ligament surgery: Experiences from Miami. Clin Orthop 325: 91–99, 1996
ence screw for fixation of bone-patellar tendon-bone autograft in arthro-
89. Vuori I, Heinonen A, Sievanen H, et al: Effects of unilateral strength
scopic anterior cruciate ligament reconstruction: A preliminary report.
training and detraining on bone mineral density and content in young
Knee Surg Sports Traumatol Arthrosc 5: 217–221, 1997
women. A study of mechanical loading and deloading on human bones.
61. Matthews LS, Soffer SR: Pitfalls in the use of interference screws for
Calcif Tissue Int 55: 59 – 67, 1994
anterior cruciate ligament reconstruction: Brief report. Arthroscopy 5: 225–
90. Walton M, Cameron M: Efficacy of an absorbable interference screw for
graft fixation anterior cruciate ligament reconstruction: A study using a
62. Matthews LS, Yahiro MA, Lawrence SJ, et al: Fixation strengths of bone-
sheep model. J Bone Joint Surg 78B (Suppl 2 & 3): 126, 1996
patellar tendon-bone grafts [abstract]. Am J Sports Med 18: 556 –557,
91. Weiler A, Helling H-J, Kirch U, et al: Foreign-body reaction and the course
of osteolysis after polyglycolide implants for fracture fixation. Experimental
63. Morgan CD, Kalmam VR, Grawl DM: Isometry testing for anterior cruciate
study in sheep. J Bone Joint Surg 78B: 369 –376, 1996
ligament reconstruction revisited. Arthroscopy 11: 647– 659, 1995
92. Weiler A, Hoffman RFG, Bail HJ, et al: Tendon healing in a bone tunnel.
64. Morrison JB: The mechanics of the knee joint in relation to normal walking.
Histological analysis after biodegradable interference fit fixation. Arthros-
J Biomech 3: 51– 61, 1970
copy 15: 548 –549, 1999
65. Morrison JB: Function of the knee joint in various activities. Biomed Eng 4:
93. Weiler A, Hoffmann RFG, Siepe CJ, et al: The influence of screw geom-
etry on hamstring tendon interference fit fixation. Am J Sports Med 28:
66. Morrison JB: Bioengineering analysis of force actions transmitted by the
knee joint. Biomed Eng (April): 164, 1968
67. Nebelung W, Becker R, Merkel M, et al: Bone tunnel enlargement after
94. Weiler A, Hoffmann RFG, Sta¨helin AC, et al: Hamstring tendon fixation
anterior cruciate ligament reconstruction with semitendinosus tendon us-
using interference screws. A biomechanical study in calf tibial bone.
ing EndoButton fixation on the femoral side. Arthroscopy 14: 810 – 815,
Arthroscopy 14: 29 –37, 1998
95. Weiler A, Hoffmann RFG, Sudkamp NP, et al: Replacement of the anterior
68. Noyes FR, Barber-Westin SD: Revision anterior cruciate ligament sur-
cruciate ligament. Biomechanical study for patellar and semitendinosus
gery: Experiences from Cincinnati. Clin Orthop 325: 116 –129, 1996
tendon fixation with poly(D,L-lactide) interference screw [in German].
69. Noyes FR, Butler DL, Grood ES, et al: Biomechanical analysis of human
Unfallchirurg 102: 115–123, 1999
ligament grafts used in knee-ligament repairs and reconstructions. J Bone
96. Weiler A, Scheffler S, Go¨ckenjan A, et al: Different hamstring tendon graft
Joint Surg 66A: 344 –352, 1984
fixation techniques under incremental cyclic loading conditions [abstract].
70. Pena F, Gro¨ntvedt T, Brown GA, et al: Comparison of failure strength
Arthroscopy 14: 425– 426, 1998
between metallic and absorbable interference screws. Influence of inser-
97. Weiler A, Windhagen HJ, Raschke MJ, et al: Biodegradable interference
tion torque, tunnel-bone block gap, bone mineral density, and interfer-
screw fixation exhibits pull-out force and stiffness similar to titanium
ence. Am J Sports Med 24: 329 –334, 1996
screws. Am J Sports Med 26: 119 –128, 1998
71. Pistner H, Bendix RR, Muhling J, et al: Poly(L-Lactide): A long term study
98. Woo SL-Y, Hollis JM, Adams DJ, et al: Tensile properties of the human
in vivo. Part III. Analytical characterization. Biomaterials 14: 291–298,
femur-anterior cruciate ligament-tibia complex: The effects of specimen
age and orientation. Am J Sports Med 19: 217–225, 1991
Source: http://www.knee.ae/wp-content/themes/international_knee_joint/pdf/ACL_graft%20_fixation_current_concepts.pdf
Commentary/ Walker: A refined model of sleep and the time course of memory formation which settles the debate about the exclusiveness of memory con- tical inversion of the visual field. In the second study, the persons solidation during sleep. who experienced incorporations of the inverted visual field in In describing the findings regarding procedural memory and
Modeling the Invasion of Community-AcquiredMethicillin-Resistant Staphylococcus aureus intoHospitals Erica M. C. D'Agata,1 Glenn F. Webb,2 Mary Ann Horn,2,3 Robert C. Moellering, Jr.,1 and Shigui Ruan4 1Division of Infectious Diseases, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts; 2Department ofMathematics, Vanderbilt University, Nashville, Tennessee; 3Division of Mathematical Sciences, National Science Foundation, Arlington, Virginia;and 4Department of Mathematics, University of Miami, Coral Gables, Florida