Viagra gibt es mittlerweile nicht nur als Original, sondern auch in Form von Generika. Diese enthalten denselben Wirkstoff Sildenafil. Patienten suchen deshalb nach viagra generika schweiz, um ein günstigeres Präparat zu finden. Unterschiede bestehen oft nur in Verpackung und Preis.
Slide
•
Previous anesthesia experience?
Assessment: Assign an ASA physical status classification
•
Health History: Coronary artery disease, asthma, hypertension, kidney or liver
A normal, healthy patient
disease, or reflux?
A patient with mild systemic disease with minimal activity restriction.
•
Social History: Smoke, drink, or abuse drugs?
Examples include hypertension, asthma, chronic bronchitis, obesity or
•
Medications and allergies: Consumption on day of surgery?
diabetes mellitus.
•
Family History: Anesthesia complications?
A patient with a severe systemic disease that limits activity but is not
•
Last Meal?
Teeth status?
EKG?
Labs?
Examples include severe diabetes with systemic complications, history of
myocardial infarction, angina pectoris, or poorly controlled hypertension.
•
Airway Exam: Predicting the
ease of tracheal intubation is a function of:
A patient with severe systemic disease that is a constant threat to life
1.
Atlanto-occipital joint extension should be greater than 35 degrees to ensure
Examples include severe cardiac, pulmonary, renal, hepatic, or endocrine
exposure of the glottic opening during direct laryngoscopy.
2.
Thyromental distance is the distance from the notch of the thyroid cartilage to
ASA 5: A moribund patient who is not expected to survive 24 hours with or
the tip of the mentum and if greater than 6 cm is correlated with an easier direct
without the operation.
Examples include major multi-system or cerebral trauma, ruptured
3.
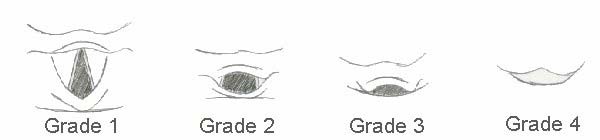
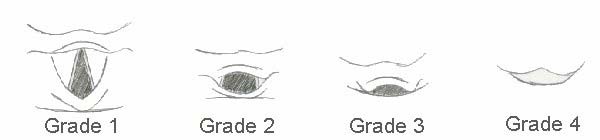
Mallampati airway evaluation
aneurysm, or large pulmonary embolism
serves as a predictor of difficult
ASA 6: A declared brain-dead patient whose organs are being removed for donor
intubations with class 1 being easier
Emergency Operation (E): Any patient in whom an emergency operation is required
Determine Anesthesia Type:
In holding before going to OR: obtain peripheral IV access
•
Pharmacologic Premedication: Midazolam AKA
Versed (.02-.08 mg/kg IV titrated in 1-
Involves blocking nerve conduction with local anesthetics producing analgesia
2 mg increments), a
Benzodiazepine, produces sedation, reduces anxiety, and causes
intra- and post-operatively. It can be used alone or in conjunction with IV
sedation or general anesthesia. Types include spinal anesthesia, epidural
Monitors: Applied in OR
anesthesia, femoral nerve block, and brachial plexus block. Drugs used include:
•
Pulse Oximeter: measures the peripheral arterial hemoglobin oxygen saturation
Bupivicaine (Marcaine), Lidocaine, and Mepivicaine. For information on specific
(SpO2) and reflects the arterial hemoglobin oxygen saturation (SaO2). Apply to a finger
nerve block techniques, consult www.nysora.com
on arm opposite the blood pressure cuff to prevent reading interruptions.
•
Monitored Anesthesia Care (MAC) or
IV Sedation:
•
Automated Arterial Blood Pressure Cuff: place on arm opposite the IV as not to
A cross between local anesthesia and general anesthesia, MAC or IV sedation
disrupt IV flow. Cuff width should measure 40% of the arm's circumference; too
enables the patient to breathe independently and stay "light" allowing the patient
small/large a cuff will over/underestimate blood pressure.
to respond to verbal commands and move with assistance. IV medications
•
Electrocardiogram: a V lead EKG is typically used. Place "white to right" (i.e. white
include Midazolam (Versed), Fentanyl, and Propofol.
lead to right shoulder), "smoke over fire" (i.e. black lead to left shoulder and red lead to
•
General Anesthesia:
left lower chest), "when driving, right pushes green gas, left pushes red brake" (i.e. green
Used for most longer surgeries, general anesthesia has three essential
lead to right lower chest, red to left lower chest), and brown lead at the apex.
characteristics: amnesia (or unconsciousness), analgesia, and lack of movement.
•Applied after intubation:
Temp. probe (esophageal, skin, or nasal),
Capnography
General anesthesia requires intubation with an endotracheal tube or laryngomask
(measures end-tidal CO2),
A-line (allows continuous recording of systemic BP and
airway and the use of volatile anesthetic gases.
provides access to obtain blood for analysis of ABG's, pH, and electrolytes),
BIS
monitor (a sensor strip placed on patient's forehead measures consciousness with a
Prepare the room: Using the pneumonic MS. MAID
score < 60 correlating with unconsciousness),
Twitch monitor (a black-distal and red-
Check
Machine
, Suction
, Monitors
, Airway supplies,
IV equipment, and
Drug
proximal electrode is placed over the ulnar nerve to measure neuromuscular blockade) B
Induction of general anesthesia is usually accomplished by IV meds
•Preoxygenation (100% x3 min with normal tidal volumes or 100% x1 min with 8 vital capacity breaths)
Positioning: To ensure the best view, elevate the
•Fentanyl (0.5-0.2 μg/kg)
patient's head 8-10 cm with pads under the occiput with
An Opioid, Fentanyl if given 3 minutes prior to induction 1. blunts the sympathetic response often induced by
extension of the head at the atlanto-occipital angle.
intubation and 2. preemptive analgesia with opioids may reduce the need for analgesics in the post-operative period.
Laryngoscope blade choices: 1. Curved (Macintosh)
•Lidocaine (1-1.5 mg/kg)
Blade: tip is advanced between the base of the tongue and
A Local Anesthetic, Lidocaine 1. decreases reflexes associated with airway stimulation and 2. decreases the
the valecula. 2. Straight (Miller) Blade: tip is advanced over
"burn" of propofol entering vein.
the epiglottis. Laryngoscopes are numbered according to
•Propofol (1.5-2.5 mg/kg)
their length; a #3 is used on most adult patients
The most common IV Anesthetic, Propofol produces unconsciousness within 30 seconds and is associated
Direct Laryngoscopy Views: Classified Grade 1-4
with hypotension, ventilation depression, and decreased incidence of post-op nausea. Emulsified in an egg
mixture, beware of egg allergy and propensity to support bacterial growth if used > 6 hours after opening. Can
burn while entering vein. Other IV Anesthetics include: Thiopental (3-5 mg/kg, a barbiturate, hypotension,
long-lasting), Etomidate (0.2-0.4 mg/kg, no BP changes, may cause seizure and adrenocortical supression),
Ketamine (1-2 mg/kg, causes "dissociative anesthesia").
•Succinylcholine (1-2 mg/kg)
Tracheal tube size and length: Tracheal tubes are sized according to the internal
A Depolarizing Muscle Relaxant, Succinylcholine is a competitive inhibitor of acetylcholine and depolarizes
the postjunctional membrane producing fasciculation and then skeletal muscle paralysis within 30-60 seconds.
diameter in mm. The typical sizes and distance from cuff to mouth is 7mm and 21cm
To prevent fasciculation, use 10-15% of a normal dose of Nondepolarizing Muscle Relaxant. As an alternative to
for females and 8mm and 23cm for males.
Succinylcholine, Nondepolarizing Muscle Relaxants can be used for induction: Vecuronium (0.1 mg/kg),
Confirmation of tube in correct position:
Rocuronium (0.6-1.2 mg/kg), Cisatracurium (0.1 mg/kg). Nondepolarizing Muscle Relaxants are
1. Symmetric bilateral movement of the chest with bilateral breath sounds
noncompetitive inhibitors of acetylcholine. They are longer-lasting than Succinylcholine and therefore you only want to use it if you are confident that you can intubate and/or bag-mask the patient.
2. Condensation in the tube3. Sustained end-tidal PCO2 > 30 mmHg x 6 breaths
*MAC=Minimum Alveolar Concentration of an inhaled anesthetic at 1
atm that prevents response to noxious stimulus in skeletal muscle
Dose Facts
Deliver patients to Post Anesthesia Care Unit (PACU). PACU nurses will place
Sevoflurane MAC*=1.8
Wel tolerated for inhalation induction; rapid onset/offset; decreases BP and HR; breakdown product compound A is nephrotoxic in animalsÆ keep
monitors on patient. The anesthesiologist will leave orders with the PACU nurses for
flows > 2L/min
medicines prn.
Airway irritant; decreases BP and HR; rapid onset/offset
Airway irritant; decreases BP and HR; long onset/offset
Nitrous Oxide
The prototype Opioid, Morphine produces analgesia, euphoria
Well tolerated for inhalation induction; decreases volatile anesthetic
sedation, decreased ability to concentrate, respiratory depression, an
requirement; diffuses into gas filled areas (pneumothorax, bowel, middle ear)
impairment of compensatory sympathetic response, nausea, and
: Ephedrine
10-25mg Indirect-acting sympathomimeticÆ stimulates norepinephrine releaseÆ
vomiting. More effective at relieving dull pain versus sharp,
intermittent pain.
Meperidine
An Opioid, Meperidine (Demerol) is about 1/10 as potent as morphine
Phenylephrine 0.05-0.2mg Direct-acting
sympathomimeticÆ alpha agonistÆ raises BP
GE Labetolol
and is unique in suppressing post-operative shivering. It is structurally
0.1-0.5 mg/kg Alpha-1 and nonselective beta antagonistÆ lowers BP and HR
similar to atropine and may cause tachycardia and mydriasis.
MANA Esmolol
0.2-0.5 mg/kg Beta-1 antagonistÆ lowers BP and HR
Hydromorphone 2-4 mg
An Opioid, Hydromorphone (Dilaudid) should be used in smaller
AnticholinergicÆ increases HR, antisialagogue effect
doses with renal or liver disease and geriatrics.
Dexamethasone 4 mg
Use in beginning of surgery; also used to decrease intra-cranial pressure
A NSAID, Ketorolac (Toradol) is effective in treating muscular pain
and can be used concomitantly with an opioid. As it is an NSAID, it
TICS: Ondansetron 4 mg
Use 20 minutes prior to the end of surgery
Duration to
causes platelet dysfunctionÆ beware of bleeding and should not be
T Vecuronium
Onset return to >25%
No cardiovascular side effects; hepatic/renal excretion 3-5 min 20-35 min
used with renal disease.
Renal failure can extend duration of action
Acetaminophen (Tylenol) is useful for mild to moderate pain and fever
Spontaneous hydrolysis in plasma
3-5 min 20-35 min
Neostigmine .04-.07 mg/kg An anticholinesterase, neostigmine "reverses" the depolarizing neuromuscular
blocking agents; increases the acetylcholine at muscarinic and nicotinic
Ondansetron (Zoffran) original y developed as an anti-emetic for
receptorsÆ causes tachycardia, salivation, and bronchoconstriction- therefore
chemotherapy is useful for post-op nausea and/or vomiting
use anticholinergic Glycopyrolate (@ 0.01 mg/kg) to minimize the muscarinic
Black box warning due to QT prolongation seen with large doses
receptor activation. Use if "train of four" shows 4-2 twitches.
Source: http://www.anesthesiology.vcu.edu/docs/Anesthesia%20Primer.pdf
Ann Onymous Initial Report of Findings March 2016 February 2008 BLUME HEALING CENTER Dr. Jason Passey, DC, CCSP 1611 Kresky Avenue Suite 108 Centralia, WA 98531 Phone: (360) 330-1800 Fax: (360) 330-5866 NUTRITION EVALUATION: 03/20/2016 DATA USED FOR ANALYSIS
Good to be healthy! JSC "Grindeks", LatviaRiga, LV-1057, 53 Krustpils St.Ph: +371 67 083 205; + 371 67 083 500Fax: + 371 67 083 505E-mail: [email protected] Carrying the name of Latvia into the world and developing national pharmaceutical values, Latvia can be proud of the leading pharmaceutical company in the Baltic States - "Grindeks". The successful operation of the company is not only verified by its performance, but is also acknowledged by the industry specialists, feedback from patients and received awards. In 2010 "Grindeks" received the title of most exportable company in Latvia, while in 2012 "Grindeks" received the International diamond prize for Excellence in Quality. Award was presented by the European Organisation for Quality Research. In terms of reputation, "Grindeks" is in the forefront of the best companies in Latvia by taking first place in the industry for several years. "Grindeks" is also among the best employers of Latvia. Medication and active pharmaceutical ingredients manufactured by the company are highly evaluated in Latvia and abroad.